Abstract
Background
Iatrogenic nerve lesions during surgical interventions are avoidable complications that may cause severe functional impairment. Hereby, awareness of physicians and knowledge of structures and interventions at risk is of utmost importance for prevention. As current literature is scarce, we evaluated all patients treated surgically due to peripheral nerve injuries in our specialized nerve center for the presence of iatrogenic nerve lesions.
Methods
We evaluated a total of 5026 patients with peripheral nerve injuries treated over a time period of 8 years in our facility for the prevalence of iatrogenic nerve injuries, their clinical presentations, time to treatment, mechanisms and intraoperative findings on nerve continuity.
Results
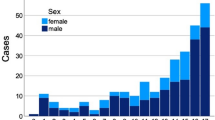
A total of 360 (6.1%) patients had an iatrogenic cause resulting in 380 injured nerves. 76.6% of these lesions affected the main branch of the injured nerve, which were mainly the radial (30.5%), peroneal (13.7%) and median nerve (10.3%). After a mean delay of 237 ± 344 days, patients presented 23.2% with a motor and 27.9% with a mixed sensory and motor deficit. 72.6% of lesions were in-continuity lesions. Main interventions at risk are displayed for every nerve, frequently concerning osteosyntheses but also patient positioning and anesthesiologic interventions.
Discussion
Awareness of major surgical complications such as iatrogenic nerve injuries is important for surgeons. An often-seen trivialization or “watch and wait” strategy results in a huge delay for starting an adequate therapy. The high number of in-continuity lesions mainly in close proximity to osteosyntheses makes diagnosis and treatment planning a delicate challenge, especially due to the varying clinical presentations we found. Diagnostics and therapy should therefore be performed as early as possible in specialized centers capable of performing nerve repair as well as salvage therapies.




Similar content being viewed by others
References
Kretschmer T, Antoniadis G, Braun V et al (2001) Evaluation of iatrogenic lesions in 722 surgically treated cases of peripheral nerve trauma. J Neurosurg 94:905–912. https://doi.org/10.3171/jns.2001.94.6.0905
Weber RV, Mackinnon SE (2007) Median nerve mistaken for palmaris longus tendon: restoration of function with sensory nerve transfers. HAND 2:1–4. https://doi.org/10.1007/s11552-006-9011-5
McGeorge D, Sturzenegger M, Buchler U (1992) Tibial nerve mistakenly used as a tendon graft. Reports of three cases. J Bone Joint Surg Br 74:365–366. https://doi.org/10.1302/0301-620X.74B3.1587878
Antoniadis G, Kretschmer T, Pedro MT et al (2014) Iatrogenic nerve injuries. Dtsch Ärztebl Int. https://doi.org/10.3238/arztebl.2014.0273
Stöhr M (1996) Iatrogene Nervenläsionen: Injektion, Operation, Lagerung, Strahlentherapie ; 33 Tabellen, 2., vollst. überarb. Aufl. Thieme, Stuttgart New York
Khan R, Birch R (2001) Iatropathic injuries of peripheral nerves. J Bone Joint Surg Br 83:1145–1148. https://doi.org/10.1302/0301-620X.83B8.0831145
Harhaus L, Daeschler SC, Aman M, et al (2022) [Differential therapeutic approaches in treatment of carpal tunnel syndrome]. Handchir Mikrochir Plast Chir Organ Deutschsprachigen Arbeitsgemeinschaft Handchir Organ Deutschsprachigen Arbeitsgemeinschaft Mikrochir Peripher Nerven Gefasse Organ V 54:236–243. https://doi.org/10.1055/a-1839-8297
Aman M, Boecker AH, Thielen M et al (2021) Single incision thenar muscle reconstruction using the free functional pronator quadratus flap. BMC Surg 21:310. https://doi.org/10.1186/s12893-021-01308-x
Boecker AH, Lukhaup L, Aman M et al (2022) Evaluation of MR-neurography in diagnosis and treatment in peripheral nerve surgery of the upper extremity: a matched cohort study. Microsurgery 42:160–169. https://doi.org/10.1002/micr.30846
Aman M, Schwarz D, Stolle A et al (2022) Modern MRI diagnostics of upper-extremity-related nerve injuries-a prospective multi-center study protocol for diagnostics and follow up of peripheral nerve injuries. J Pers Med 12:1548. https://doi.org/10.3390/jpm12101548
Lefebvre R, Russo F, Navo P, Stevanovic M (2020) Characteristics of iatrogenic nerve injury from orthopedic surgery correlate with time to subspecialty presentation. Plast Reconstr Surg Glob Open 8:e2678. https://doi.org/10.1097/GOX.0000000000002678
Bage T, Power DM (2021) Iatrogenic peripheral nerve injury: a guide to management for the orthopaedic limb surgeon. EFORT Open Rev 6:607–617. https://doi.org/10.1302/2058-5241.6.200123
Dahlin LB, Wiberg M (2017) Nerve injuries of the upper extremity and hand. EFORT Open Rev 2:158–170. https://doi.org/10.1302/2058-5241.2.160071
van der Avoort DJJC, Hovius SER, Selles RW et al (2013) The incidence of symptomatic neuroma in amputation and neurorrhaphy patients. J Plast Reconstr Aesthetic Surg JPRAS 66:1330–1334. https://doi.org/10.1016/j.bjps.2013.06.019
Watson J, Gonzalez M, Romero A, Kerns J (2010) Neuromas of the hand and upper extremity. J Hand Surg 35:499–510. https://doi.org/10.1016/j.jhsa.2009.12.019
Radtke C, Vogt PM (2014) Nerve injuries and posttraumatic therapy. Unfallchirurg 117:539–555. https://doi.org/10.1007/s00113-014-2574-7
Amrami KK, Khanna A, Frick MA, Spinner RJ (2023) Imaging peripheral nerve injuries of the lower extremities: what surgeons need to know. Semin Ultrasound CT MR 44:347–363. https://doi.org/10.1053/j.sult.2023.04.001
Aman M, Böcker A, Kneser U, Harhaus L (2021) Selective nerve transfers for thenar branch reconstruction. Oper Orthop Traumatol 33:384–391. https://doi.org/10.1007/s00064-020-00689-1
Funding
The authors received no financial support for the research, authorship and publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a potential conflict of interest with respect to the research, authorship, mentioned products or devices and publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aman, M., Zimmermann, K.S., Pennekamp, A. et al. Mechanisms, interventions at risk and clinical presentation of iatrogenic nerve lesions in trauma patients. Arch Orthop Trauma Surg 143, 7245–7253 (2023). https://doi.org/10.1007/s00402-023-05009-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05009-3