Abstract
Objective
Peroneus longus tendon (PLT) has become a reliable autologous graft option for various ligament reconstructions. But there are potential risks and complications associated with its use as a graft. This retrospective study aimed to examine the complications and donor site morbidity following PLT harvesting.
Patients and methods
A retrospective review was performed on an institutional digital patient database, and all patients who underwent ligament reconstruction using PLT autograft were identified. Intraoperative, early, and late complications were reviewed using digital patient notes and patients underwent a complete physical examination during their final follow-up. Ankle function was assessed using the AOFAS score, and manual ankle muscle testing was performed on both sides. Sural nerve iatrogenic injury was evaluated with a dermatomal light touch examination. Cosmetic satisfaction due to incision scar and footwear complaints were also assessed.
Results
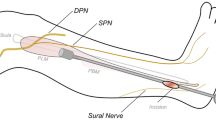
82 patients (74 male, eight female) with a mean age of 31.9 ± 10.4 years (range, 16–66) were included in the final analysis. The mean follow-up time was 46.6 ± 30.3 months (range, 6–109). The mean AOFAS score for the donor side was 98.7 ± 3.3 (range, 87–100), and the contralateral side score was 100, with manual muscle testing graded as 5 in all movements and similar to the contralateral side. Fifteen patients (18.3%) had hypoesthesia over the dorsolateral aspect of the foot distal to the incision scar, two patients (2.4%) had hyperalgesia over the distal incision scar, and one patient (1.2%) had mild ankle instability. There were two cases (2.4%) of compartment syndrome, both of which were treated with fasciotomy and had complete regression of symptoms after 5 days. One patient (1.2%) had a transient peroneal nerve injury and foot drop that resolved in the sixth month.
Conclusions
The results of this retrospective study suggest that harvesting the PLT is associated with a high rate of complications and donor site morbidity. The most common complication was hypoesthesia around the lateral side of the foot, although the ankle functions were not affected significantly. Two cases of compartment syndrome and one transient peroneal nerve injury were observed. Care should be taken while harvesting PLT autograft, and it should be kept in mind that peroneal nerve injury might occur.
Level of evidence
Level IV, retrospective case series.

Similar content being viewed by others
Data availability
The data used in this study is available on reasonable request from the authors.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACLR:
-
Anterior cruciate ligament reconstruction
- AOFAS:
-
American Orthopedic Foot and Ankle Society
- CPN:
-
Common peroneal nerve
- FADI:
-
Foot and Ankle Disability Index
- PB:
-
Peroneus Brevis
- PCL:
-
Posterior cruciate ligament
- PLT:
-
Peroneus longus tendon
References
Baawa-Ameyaw J, Plastow R, Begum FA, Kayani B, Jeddy H, Haddad F (2021) Current concepts in graft selection for anterior cruciate ligament reconstruction. EFORT Open Rev 6(9):808–815. https://doi.org/10.1302/2058-5241.6.210023
Buerba RA, Boden SA, Lesniak B (2021) Graft selection in contemporary anterior cruciate ligament reconstruction. J Am Acad Orthop Surg Glob Res Rev 5(10):e21.00230. https://doi.org/10.5435/JAAOSGlobal-D-21-00230
Lin KM, Boyle C, Marom N, Marx RG (2020) Graft selection in anterior cruciate ligament reconstruction. Sports Med Arthrosc Rev 28(2):41–48. https://doi.org/10.1097/JSA.0000000000000265
Kerimoglu S, Aynaci O, Saracoolu M, Aydin H, Turhan AU (2008) Anterior cruciate ligament reconstruction with the peroneus longus tendon. Acta Orthop Traumatol Turc 42(1):38–43. https://doi.org/10.3944/aott.2008.038
He J, Tang Q, Ernst S, Linde MA, Smolinski P, Wu S, Fu F (2021) Peroneus longus tendon autograft has functional outcomes comparable to hamstring tendon autograft for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 29(9):2869–2879. https://doi.org/10.1007/s00167-020-06279-9
Yadav U, Nemani M, Devgun A, Malik M, Agrawal GK (2022) Iatrogenic foot drop after anterior cruciate ligament reconstruction with peroneus longus tendon autograft: report of a rare case. Cureus. 14(6):e26476. https://doi.org/10.7759/cureus.26476
Zhao J, Huangfu X (2012) The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med 40(3):662–671. https://doi.org/10.1177/0363546511428782
Angthong C, Chernchujit B, Apivatgaroon A, Chaijenkit K, Nualon P, Suchao-in K (2015) The anterior cruciate ligament reconstruction with the peroneus longus tendon: a biomechanical and clinical evaluation of the donor ankle morbidity. J Med Assoc Thai 98(6):555–560
Liu CT, Lu YC, Huang CH (2015) Half-peroneus-longus-tendon graft augmentation for unqualified hamstring tendon graft of anterior cruciate ligament reconstruction. J Orthop Sci 20(5):854–860. https://doi.org/10.1007/s00776-015-0744-2
Khajotia BL, Chauhan S, Sethia R, Chopra BL (2018) Functional outcome of arthroscopic reconstruction of anterior cruciate ligament tear using peroneus longus tendon autograft. Int J Res Orthop 4(6):898–903. https://doi.org/10.18203/issn.2455-4510.IntJResOrthop20184382
Shi FD, Hess DE, Zuo JZ, Liu SJ, Wang XC, Zhang Y, Meng XG, Cui ZJ, Zhao SP, Li CJ, Hu WN (2019) Peroneus longus tendon autograft is a safe and effective alternative for anterior cruciate ligament reconstruction. J Knee Surg 32(8):804–811. https://doi.org/10.1055/s-0038-1669951
Bi M, Zhao C, Zhang S, Yao B, Hong Z, Bi Q (2018) All-inside single-bundle reconstruction of the anterior cruciate ligament with the anterior half of the peroneus longus tendon compared to the semitendinosus tendon: a two-year follow-up study. J Knee Surg 31(10):1022–1030. https://doi.org/10.1055/s-0038-1627466
Trung DT, Manh SL, Thanh LN, Dinh TC, Dinh TC (2019) Preliminary result of arthroscopic anterior cruciate ligament reconstruction using anterior half of peroneus longus tendon autograft. Open Access Maced J Med Sci 7(24):4351–4356. https://doi.org/10.3889/oamjms.2019.390
Setyawan R, Soekarno NR, Asikin AIZ, Rhatomy S (2019) Posterior cruciate ligament reconstruction with peroneus longus tendon graft: 2-years follow-up. Ann Med Surg (Lond) 43:38–43. https://doi.org/10.1016/j.amsu.2019.05.009
Rhatomy S, Asikin AIZ, Wardani AE, Rukmoyo T, Lumban-Gaol I, Budhiparama NC (2019) Peroneus longus autograft can be recommended as a superior graft to hamstring tendon in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27(11):3552–3559. https://doi.org/10.1007/s00167-019-05455-w
Kumar VK, Narayanan SK, Vishal RB (2020) A study on peroneus longus autograft for anterior cruciate ligament reconstruction. Int J Res Med Sci 8(1):183–188. https://doi.org/10.18203/2320-6012.ijrms20195904
Shao X, Shi LL, Bluman EM, Wang S, Xu X, Chen X, Wang J (2020) Satisfactory functional and MRI outcomes at the foot and ankle following harvesting of full thickness peroneus longus tendon graft. Bone Jt J 102-B(2):205–211. https://doi.org/10.1302/0301-620X.102B2.BJJ-2019-0949.R1
Joshi S, Shetty UC, Salim MD, Meena N, Kumar RS, Rao VK (2021) Peroneus longus tendon autograft for anterior cruciate ligament reconstruction: a safe and effective alternative in nonathletic patients. Niger J Surg 27:42–47. https://doi.org/10.4103/njs.NJS_22_20
Sahu MM, Pragassame AS, Mohanty P, Sahoo PK (2021) Evaluation of donor ankle function after harvesting peroneus longus tendon graft for anterior cruciate ligament reconstruction-a prospective cohort study. J Clin Diagn Res 15(9):13–17. https://doi.org/10.7860/JCDR/2021/49882.15383
Bi M, Zhao C, Zhang Q, Cao L, Chen X, Kong M, Bi Q (2021) All-inside anterior cruciate ligament reconstruction using an anterior half of the peroneus longus tendon autograft. Orthop J Sports Med 9(6):2325967121991226. https://doi.org/10.1177/2325967121991226
Goyal T, Paul S, Choudhury AK, Sethy SS (2023) Full-thickness peroneus longus tendon autograft for anterior cruciate reconstruction in multi-ligament injury and revision cases: outcomes and donor site morbidity. Eur J Orthop Surg Traumatol 33(1):21–27. https://doi.org/10.1007/s00590-021-03145-3
Rajani AM, Shah UA, Mittal AR, Rajani A, Punamiya M, Singhal R (2022) Functional and clinical outcome of anterior cruciate ligament reconstruction with peroneus longus autograft and correlation with MRI after 3 years. J Orthop 34:215–220. https://doi.org/10.1016/j.jor.2022.08.027
Singh H, Agarwal KK, Tyagi S, Bhrambhatt P, Rampurwala A, Unjia R, Agarwal N (2022) A study of the functional outcome of supplementation of hamstring graft with anterior half of the peroneus longus tendon in arthroscopic anterior cruciate ligament reconstruction. Cureus 14(10):e30138. https://doi.org/10.7759/cureus.30138
Rhatomy S, Hartoko L, Setyawan R, Soekarno NR, Zainal Asikin AI, Pridianto D, Mustamsir E (2020) Single bundle ACL reconstruction with peroneus longus tendon graft: 2-years follow-up. J Clin Orthop Trauma 11(Suppl 3):S332–S336. https://doi.org/10.1016/j.jcot.2019.09.004
Keyhani S, Qoreishi M, Mousavi M, Ronaghi H, Soleymanha M (2022) Peroneus longus tendon autograft versus hamstring tendon autograft in anterior cruciate ligament reconstruction: a comparative study with a mean follow-up of two years. Arch Bone Jt Surg 10(8):695–701. https://doi.org/10.22038/ABJS.2022.59568.2938
Lu Y, Xu H, Zhou Z, Fang L, Tao R (2022) The promotive effect of grafts with the double-stranded peroneus longus tendon and with the four-stranded hamstring tendon on reconstruction of the posterior cruciate ligament injury. Orthop Traumatol Surg Res 108(8):103336. https://doi.org/10.1016/j.otsr.2022.103336
Nazem K, Barzegar M, Hosseini A, Karimi M (2014) Can we use peroneus longus in addition to hamstring tendons for anterior cruciate ligament reconstruction? Adv Biomed Res 3:115. https://doi.org/10.4103/2277-9175.132696
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley AJ, Myerson MS, Sanders M, Lutter LD (1997) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 18(3):187–188. https://doi.org/10.1177/107110079701800315
Rider LG, Koziol D, Giannini EH et al (2010) Validation of manual muscle testing and a subset of eight muscles for adult and juvenile idiopathic inflammatory myopathies. Arthr Care Res (Hoboken) 62(4):465–472. https://doi.org/10.1002/acr.20035
Grassi A, Perdisa F, Samuelsson K, Svantesson E, Romagnoli M, Raggi F, Gaziano T, Mosca M, Ayeni O, Zaffagnini S (2018) Association between incision technique for hamstring tendon harvest in anterior cruciate ligament reconstruction and the risk of injury to the infra-patellar branch of the saphenous nerve: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 26(8):2410–2423. https://doi.org/10.1007/s00167-018-4858-x
He J, Byrne K, Ueki H, Kanto R, Linde MA, Smolinski P, Wu S, Fu F (2022) Low to moderate risk of nerve damage during peroneus longus tendon autograft harvest. Knee Surg Sports Traumatol Arthrosc 30(1):109–115. https://doi.org/10.1007/s00167-021-06698-2
Wu S, Rothrauff B, Li J, He J (2022) Minimizing risk of iatrogenic nerve injury during peroneus longus tendon autograft harvest: a cadaveric study at different ankle or knee positions. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-07202-0
Correia AGDS, Vieira JGS, Rodrigues BCM, Fortes LHS, Garção DC (2022) Variations in the compartmental location of the superficial fibular nerve: a cadaveric study with meta-analysis. Surg Radiol Anat 44(11):1431–1437. https://doi.org/10.1007/s00276-022-03041-3
Steele R, Coker C, Freed B, Wright B, Brauer P (2021) Anatomy of the sural nerve complex: Unaccounted anatomic variations and morphometric data. Ann Anat 238:151742. https://doi.org/10.1016/j.aanat.2021.151742
Zhao D, Pan JK, Lin FZ et al (2022) Risk factors for revision or rerupture after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. https://doi.org/10.1177/03635465221119787
Sakti M, Biakto KT, Usman MA, Tedjajuwana MJ, Pasallo P, Subagio ES (2020) Predicting the peroneus longus tendon autograft size in ACL reconstruction by using anthropometric parameters: a study in South Sulawesi population. J Orthop 22:1–4. https://doi.org/10.1016/j.jor.2020.03.011
Ertilav D (2021) Relation of peroneus longus autograft dimensions with anthropometric parameters in anterior cruciate ligament reconstruction: importance of the distal leg diameter. Jt Dis Relat Surg 32(1):137–143. https://doi.org/10.5606/ehc.2021.79580
Song X, Li Q, Wu Z, Xu Q, Chen D, Jiang Q (2018) Predicting the graft diameter of the peroneus longus tendon for anterior cruciate ligament reconstruction. Medicine (Baltimore) 97(44):e12672. https://doi.org/10.1097/MD.0000000000012672
Rhatomy S, Tanzil H, Setyawan R, Amanda C, Phatama KY, Andrianus J, Rukmoyo T, Kisworo B (2019) Influence of anthropometric features on peroneus longus graft diameter in Anterior Cruciate Ligament reconstruction: a cohort study. Ann Med Surg (Lond) 48:77–80. https://doi.org/10.1016/j.amsu.2019.10.023
Khan MJ, Asif N, Firoz D, Khan AQ, Sabir AB, Siddiqui YS (2021) Prediction of peroneus longus graft diameter for anterior cruciate ligament reconstruction by inframalleolar harvest and from anthropometric data. Int J Burns Trauma 11(5):377–384
Goldstein K, Jones C, Kay J, Shin J, de Sa D (2022) Tranexamic acid administration in arthroscopic surgery is a safe adjunct to decrease postoperative pain and swelling: a systematic review and meta-analysis. Arthroscopy 38(4):1366-1377.e9. https://doi.org/10.1016/j.arthro.2021.10.001
Ziai P, Benca E, von Skrbensky G, Graf A, Wenzel F, Basad E, Windhager R, Buchhorn T (2013) The role of the peroneal tendons in passive stabilisation of the ankle joint: an in vitro study. Knee Surg Sports Traumatol Arthrosc 21(6):1404–1408. https://doi.org/10.1007/s00167-012-2273
Alanen J, Orava S, Heinonen OJ, Ikonen J, Kvist M (2001) Peroneal tendon injuries. Report of thirty-eight operated cases. Ann Chir Gynaecol 90(1):43–46
Patterson MJ, Cox WK (1999) Peroneus longus tendon rupture as a cause of chronic lateral ankle pain. Clin Orthop Relat Res 365:163–166. https://doi.org/10.1097/00003086-199908000-00021
Kerimoğlu S, Koşucu P, Livaoğlu M, Yükünç I, Turhan AU (2009) Magnetic resonance imagination of the peroneus longus tendon after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 17(1):35–39. https://doi.org/10.1007/s00167-008-0626-7
Funding
No funds have been received for this study.
Author information
Authors and Affiliations
Contributions
Study conception and design: AC, OK, HS. Acquisition of data: HS, OFE, ET, FD. Analysis and interpretation of data: OK, ET, AC. Drafting of the manuscript: OK, AC, ET, OFE, HS, FD. Critical revision: OK, AC, ET, HS, OFE, FD (Initials of authors’ names).
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest to declare.
Ethical approval
Institutional Review Board approved the study protocol (Date/Issue: 2023/26.01-2/4).
Informed consent
Written informed consent was provided by the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cakar, A., Kose, O., Selcuk, H. et al. Complications of peroneus longus tendon harvesting: a retrospective review of 82 cases. Arch Orthop Trauma Surg 143, 6675–6684 (2023). https://doi.org/10.1007/s00402-023-04988-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04988-7