Abstract
Background
This study surveyed Dutch orthopedic surgeons on the management of cartilage defects in the knee and the adherence to the recently updated Dutch knee cartilage repair consensus statement (DCS).
Methods
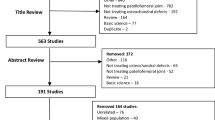
A web-based survey was sent to 192 Dutch knee specialists.
Results
The response rate was 60%. Microfracture, debridement and osteochondral autografts are performed by the majority, 93%, 70% and 27% of respondents, respectively. Complex techniques are used by < 7%. Microfracture is mainly considered in defects 1–2 cm2 (by > 80%) but also in 2–3 cm2 (by > 40%). Concomitant procedures, e.g., malalignment corrections, are performed by 89%. Twenty-one percent of surgeons treat patients aged 40–60 years. Microfracture, debridement and autologous chondrocyte implantation are not considered to be highly affected by age > 40 years by any of the respondents (0–3%). Moreover, for the middle-aged there is a large spread in treatments considered. In case of loose bodies, the majority (84%) only performs refixation in the presence of attached bone.
Conclusion
Small cartilage defects in ideal patients may be well treated by general orthopedic surgeons. The matter becomes complicated in older patients, or in case of larger defects or malalignment. The current study reveals some knowledge gaps for these more complex patients. Referral to tertiary centers might be indicated, as is stated by the DCS, and this centralization should enhance knee joint preservation. Since the data from present study are subjective, registration of all separate cartilage repair cases should fuel objective analysis of clinical practice and adherence to the DCS in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Articular cartilage defects in the knee occur frequently and may cause considerable pain and disability [1,2,3]. Cartilage regeneration or repair techniques may be indicated when cartilage defects become symptomatic.
Current techniques used in clinical practice include marrow stimulating repair techniques such as microfracture (MF) and its augmentations, regenerative techniques such as autologous chondrocyte implantation (ACI) and regenerative osteochondral scaffolds, and bone-based repair techniques—i.e., depending on osseointegration—such as osteochondral grafting using autografts or allograft transplantations (OAT and OCA) and focal knee resurfacing implants (FKRIs) [4]. MF augmentations include interventions such as autologous matrix-induced chondrogenesis. Regenerative osteochondral scaffolds include treatments such as Trufit™ (Smith and Nephew), MaioRegen (Finceramica) amd Agili-C™ (CartiHeal). Non-degradable bone-based FKRIs include HemiCAP® (Arthrosurface), Episealer® (Episurf) and BioPoly® RS Femoral Condyle (BioPoly).
In an attempt to provide guidance within the complex field of cartilage regeneration and repair, several international cartilage experts have composed guidelines or ‘treatment algorithms’. The Dutch Orthopedic Society (Nederlandse Orthopedie Vereniging—NOV) cartilage repair consensus statement for (osteo)chondral surgical repair (abbreviated Dutch Consensus Statement; DCS) was first published in 2011 and were updated in 2019 (Table 1) [5]. Although the Netherlands is known for its excellent healthcare quality and registration [6], there is no separate registration of cartilage repair, i.e., there are no cartilage specific procedural terminology (CPT) billing codes. There is consequently no information about the perception and adherence to the DCS.
The objective of this survey study was to provide insight in the applied cartilage repair techniques and adherence to the DCS in the Netherlands. In addition, this study emphasized the patient age-related considerations by orthopedic surgeons. With relatively little literature available related to the treatment of the middle-aged population, insights by orthopedic surgeons concerning their patient age-related considerations in cartilage repair aid in understanding this knowledge gap [3].
Methods
Participants
The survey recipients consisted of members of the Dutch Knee Society (DKS), which is part of the Dutch Orthopedic Society (Nederlandse Orthopeden Vereniging—NOV) and the Dutch Association for Arthroscopy (Nederlandse Vereniging voor Arthroscopie—NVA), totaling 192 orthopedic knee surgeons.
Questions
Three specialized cartilage orthopedic surgeons (JC, RC, and PE) and two residents in training (RJ and PvW) prepared questions for this survey. Questions were critically analyzed during one general meeting and three digital meetings until consensus was reached. The survey consisted of a total of 19 questions related to the treatment of cartilage defects. Questions were written in Dutch. For the purpose of the current international publication, answers were translated into English by a native English-speaking author (AW), as shown in Appendix 1.
The survey consisted of 12 general questions, including questions related to the surgeon’s experience, characteristics of typically treated patients, defect type, utilization of available therapies, and application of concomitant treatments. The general questions were followed by seven in-depth questions related to the treatment choice for different defect characteristics using the International Cartilage Repair and Joint Preservation Society (ICRS) scoring, the strategy for patients in different age categories and treatment preference for rare defects and loose cartilage bodies. In addition, a qualitative assessment was performed to assess specific rehabilitation protocols. The adherence of orthopedic surgeons to existing guidelines was evaluated using the general and in-depth questions such as cut-off points for age and body mass index (BMI), treatment choice for a given size and depth of defect, the indication and application of additional surgical techniques, and the utilization of rehabilitation protocols.
Survey distribution
The web-based survey was created in SurveyMonkey® (San Mateo, CA, USA). Orthopedic surgeons were invited by e-mail to participate in the survey. To increase the response rate, two subsequent follow-up e-mails were sent after 3 and 6 weeks. Using IP-based duplicate protection, orthopedic surgeons were prevented from completing the questionnaire twice. This study was performed according to Best Practices for Survey Research Reports [7].
Results
Participants and general questions
The response rate was 60% and 75% of respondents (n = 115) completed the survey, resulting in an overall completion rate of 44%. Respondent demographics are shown in Table 2.
Ninety-nine per cent of the respondents perform cartilage repair on the medial femoral condyle, 93% on the lateral femoral condyle, 34% on the trochlea, 16% on the patella and 13% on the tibia plateau, see Fig. 1. When asked which surgical techniques surgeons utilize, 95% of the respondents indicated they use MF, 71% use debridement, 2% use osteochondral autografts, 6% use ACI and degradable FKRIs, 6% use MF augmentations, 2% use fresh frozen osteochondral allografts and 1% use non-degradable FKRIs, see Fig. 2.
Utilization of typical cartilage repair techniques. The question leading up to these results was A: ‘I use the following techniques for cartilage repair of symptomatic cartilage defects’. MF microfracture, ACI autologous chondrocyte implantation; Regenerative osteochondral scaffolds include treatments such as Trufit™ (Smith and Nephew), MaioRegen (Finceramica), Agili-C™ (CartiHeal); MF Augmentations: MF augmentations such as autologous matrix-induced chondrogenesis. Focal implants metal/polymer includes treatments such as HemiCAP® (Arthrosurface), Episealer® (Episurf) and BioPoly® RS Femoral Condyle (BioPoly)
When faced with ICRS grade I/II defects, most respondents opt for debridement regardless of the defect size, see Fig. 3a. For ICRS grade III/IV defects up to 3 cm2, debridement and MF are both popular techniques, while the DCS maintains 2 cm2 as upper limit. Most surgeons indicate that they treat defects of 3–4 cm2 using osteochondral autografts and defects larger than 4 cm2 with ACI, see Fig. 3b. When indicated, 89% of surgeons perform concomitant surgeries; 70% perform meniscal augmentations, 64% perform ligamental reconstructions, 57% perform correction of the leg axis and six per cent answered other, see Fig. 4.
Use of different cartilage defect repair techniques for defects with ICRS 1/2 or 3/4 depths and different sizes. The question leading up to these results was A: ‘I would treat symptomatic, ICRS grade 1/2, cartilage defects with a maximum size of, with the following techniques’; and B: ‘I would treat symptomatic, ICRS grade 3/4, cartilage defects with a maximum size of, with the following techniques’. MF microfracture, ACI autologous chondrocyte implantation; Regenerative osteochondral scaffolds include treatments such as Trufit™ (Smith and Nephew), MaioRegen (Finceramica), Agili-C™ (CartiHeal); MF Augmentations: MF augmentations such as autologous matrix-induced chondrogenesis. Focal implants Metal/Polymer includes treatments such as HemiCAP® (Arthrosurface), Episealer® (Episurf) and BioPoly® RS Femoral Condyle (BioPoly)
Utilization of additional surgeries. The question leading up to these results was ‘In patients with a symptomatic cartilage defect I apply the following techniques in addition to cartilage repair:’. Ligamental reconstruction includes cruciate and or collateral ligaments; Meniscus surgery includes all meniscus surgeries such as suturing, regenerative procedures, allografts and biomaterial implants
An upper BMI (kg/m2) limit of 30 has been adopted by 46% of the respondents in accordance with the DCS. BMI was set at unlimited by 24%, at 35 by 21%, at 40 by 5% and at 25 by 4%. Seventy-two per cent of the respondents treat patient who smoke and 28% indicated they do not treat smoking patients.
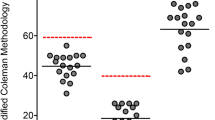
The median angle at which the respondents performed leg axis correction is 6°, the mode 5°, of which the latter is in accordance with the DCS, see Fig. 5. The majority (57%) of respondents prescribes a specific rehabilitation protocol for cartilage repair with varying strategies, but none of them mentioned specifically to employ an ICRS trained physiotherapist as dictated by the DCS, see Table 3. When indicated, 95% of respondents indicated to refer to a tertiary center.
In-depth questions
When the respondents were asked if they would fixate a loose body, 84% responded that they fixate an osteochondral loose body, 9% fixate a chondral loose body and 7% would not attempt any fixation, see Fig. 6. Twelve per cent of the respondents treat ICRS grade 5 lesions (deeper than 6.5 mm). Eighty-four per cent of the respondents treats single lesions, 35% treats multiple lesions, and 8% treats kissing lesions. Sub-analysis revealed that 75% of respondents who work in a tertiary cartilage expert clinic would treat multiple and kissing lesions, whereas 28% of surgeons in a non-expert clinic would do this.
Patient age-related considerations
The vast majority of the respondents (96%) treat patients aged 18–30 years and 67% treats patients 30–40 years. Fifty per cent treats patients under the age of 18 years, 21% treats patients 40–60 years, and one per cent treats patients older than 60 years, see Fig. 7.
When stratifying the different treatments by age group, most surgeons indicated to consider microfracture, debridement, MF augmentations, osteochondral autografts and allografts, ACI, in the categories ≤ 10 up to 40 years of age. The ultimate treatment choice thus appears to be dictated by defect characteristics in accordance with the treatment algorithms for this age group. For the age groups 40–50 and 50–60 years, the degree of agreement between respondents appears to decline, see Fig. 8. On a 5-point scale, debridement and MF augmentations are considered (58% of respondents) least affected by being middle-aged (40–65). Common treatments (debridement, MF) are not considered highly affected by middle age by any of the respondents (0–3% of respondents). Nine per cent of respondents considered allografts and biodegradable osteochondral scaffolds to be highly affected by age.
Techniques that were considered by the respondents for different patients’ age. The question leading up to these results was ‘I would consider the following techniques for the following age categories, irrespective of ICRS grade:’ ACI autologous chondrocyte implantation; MF augmentations: for example autologous matrix-induced chrondrogenesis; Focal Implants (Metal/Polymer): focal implants such as HemiCAP® (Arthrosurface), Episealer® (Episurf) and BioPoly® RS Femoral Condyle (BioPoly); Focal implants (Degradable): Regenerative osteochondral scaffolds include treatments such as Trufit™ (Smith and Nephew), MaioRegen (Finceramica), Agili-C™ (CartiHeal)
Discussion
This was the first national survey on cartilage repair in the Netherlands. The response rate of 60% was considered to be adequate, given the typical response rate of 37–51% for e-mail-based surveys [8, 9]. Such response rate highlights the widely accepted challenge in addressing cartilage defects.
Debridement and MF were the treatments employed by most surgeons and most surgeons indicate to treat the medial femoral condyle with a single lesion. This is in accordance with the incidence of cartilage defects as reported from large epidemiologic database studies [10,11,12,13,14]. For symptomatic ICRS I/II defects, no surgical intervention, debridement and to a lesser extend MF were most considered as treatment when correspondents were asked. Debridement and MF were also most considered for ICRS III/IV defects up to 3 cm2. Similar trends were previously found in a German and Turkish survey [15, 16]. However, due to the mounting evidence of its ineffectiveness [17], both the 2011 and the 2019 DCS discouraged the use of MF in defects larger than 2 cm2. Hence, Dutch orthopedic surgeons seem to deviate from the DCS on this point.
In accordance with the DCS, the BMI limit for cartilage repair was set at 30 kg/m2 by 72% of the respondents. Although it has been well established that a BMI of 30 or larger is correlated with inferior outcomes after cartilage repair procedures [18], the prevalence of patients with such a BMI and the growth of this group is significant. [19].
Concomitant surgeries like meniscal repair and leg axis corrections were performed by a large majority of respondents. This is in accordance with recent German registry data [20]. Although the question related was asked from a symptomatic cartilage defect perspective, this survey did not scrutinize if cartilage repair could also have been concomitant to an anterior cruciate ligament (ACL) repair for instance. Such situation is conceivable when an unexpected cartilage defect is encountered during arthroscopy. The incidence of severe cartilage defects with ACL injuries for instance was previously found to be 16–46% [21]. On the other hand, there is also an increasing notion that combined treatments might decrease the risk for reoperation and improve outcomes [20, 22,23,24]. With a leg axis corrections considered at 5°–6° malalignment, most correspondents follow the DCS. Similar cut-offs were found in a previous West European study [16]. Some experts in the field, however, have advocated to correct malalignment in the mechanical axis from 2 degrees or more to unload the treated compartment and enhance repair. [22, 25] In a recent German database study the cut-off for varus axis correction was 3° [23]. Emphasized by the obesity pandemic, it is of great relevance to further clarify the indication and cut-off values for alignment corrections or overcorrections since unloading is potentially beneficial for the repair [22, 26]. In addition, the large spread in the cut-off values indicated by the respondents further confirms that there is yet no consensus for when to perform a corrective osteotomy in cartilage repair.
In general, respondents indicated a low employment of more complex techniques such as ACI, MF augmentations, allografts and FKRIs. At the same time, when specifically asked, these very treatments were indicated by the respondents for larger defects with higher ICRS scores, or, in older patients. This discrepancy suggests that there is a lack of availability of treatments. In addition, the previous debate in the Netherlands concerning the cost-effectiveness and hence reimbursement of ACI is possibly related to this [27]. Similar issues were also previously reported by Elmali et al. [15] Other explanations include the availability of allografts in Europe which is—contrary to the US—hampered due to regulatory issues [28]. But perhaps the best explanation for this is the centralization of cartilage repair in the Netherlands, highlighted by a 95% referral rate on indication. Indeed, due to regulation in the Netherlands, more complex techniques such as ACI or combined surgeries are only allowed to be performed in expertise centers. Hence, the orthopedic surgeon working in the periphery may only use debridement, MF and small osteochondral autografts.
Only half of the respondents would treat patellofemoral defects, which is a surprising finding given the fact that over 1/3 of patients present with patellofemoral defects [29]. Perhaps surgeons are discouraged by the inferior outcomes in this compartment [30]. At the same time, respondents also indicated to treat tibial defects, which are considered expert level treatments with only limited evidence and often inferior outcomes [31]. Hence, the latest DCS discouraged the surgical treatment of tibial defects. In line with this is the 8% of respondents treating kissing lesions which is also discouraged. Perhaps the fact that 28% of respondents seeing patients with multiple or kissing lesions did not work in a tertiary center contributed to these unadvised treatment indications.
Loose cartilage bodies were only fixed by the majority of the respondents if there was residual bone present, i.e., osteochondral shells. This is a critically important finding since a recent study indicated that pure chondral loose bodies could in fact serve as a functional autograft, even without the need for anchoring biomaterials [32]. Moreover, the patients’ own cartilage could potentially also serve as chondrocyte or chondron source for ACI and the novel minced cartilage repair options [33].
Patient age-related considerations
Cartilage defects have been shown to be a major risk factor for osteoarthritis (OA) [3, 4]. One of the great challenges in the orthopedic community is to prevent or delay the onset of knee (early-) OA and thus prevent or delay total knee arthroplasty (TKA) [3]. Particularly, middle-aged patients—i.e., undergoing TKA in their 50s—have a high risk for revision surgery later in life [34]. Unfortunately, the fastest growing age-group undergoing cartilage repair or TKAs are the middle-aged patients [3]. Postponing TKA by means of long-lasting cartilage repair has therefore become a pressing topic. Not coincidentally, the International Cartilage Repair Society changed their society name by including ‘joint preservation’ in 2018.
The middle-aged patient is underrepresented in most of the studies investigating cartilage repair [3, 35]. It is not surprising therefore that in present survey there was a smaller degree of agreement in the results of respondents choosing treatments for older patients. Roughly 60% of respondents would consider MF as treatment in patients over 40 years of age. Importantly, when asked, most respondents did not see being middle-aged as a negative variable in cartilage repair. In fact, almost none (0-3%) of the respondents indicated that they believed any of the treatments to be highly affected by advancing age. Previous studies, however, have shown a negative effect by age on MF outcomes [3], and the detrimental effects of failed MF on consecutive treatments [3]. A recent systematic review concluded that more complex therapies such as cell-based therapies (ACI, bone marrow aspirate therapies), allografts or FKRIs have greater potential in older individuals [3].
With the aging population, it is also becoming increasingly important to evaluate the outcome of various cartilage repair treatments for different patient age categories. A major drawback in such age categorized research is that chronological age and biological age are obviously not the same. Biomarkers which differentiate in joint homeostasis are critically needed as they potentially can determine the ‘joint age’ rather than only relying on chronological age [36]. Combining biomarker data with a non-biased international registries could aid in understanding the prognostic factors of each treatment on individual level and age.
Limitations
The major limitation of present study are its subjective outcomes, which is inherent to the nature of a survey study [37]. In the absence of CPT codes to register individual cases and different repair techniques, we are unable to compare current results to objective epidemiologic values. The results of the present study should therefore be interpreted as Dutch orthopedic surgeons describing how they would treat a given patient and defect, not as a completely objective measure of how to they actually treat their patients. Nevertheless, with the assumption of relatively similar demographics, the results of present studies can be compared to large database studies [11,12,13,14] and other survey studies [15, 16]. A nationwide registry system, analogous to or combined with the Dutch Arthroplasty Register, for different cartilage defects and prognostic factors could provide objective data, rather than relying merely on subjective data.
Since we restricted the inclusion to members of orthopedic knee associations we only included surgeons with affinity for knee surgery. The very low volume orthopedic surgeon operating in a small peripheral hospital may therefore not be included. However, only a small number of respondents indicated to work in an expertise center and the results of the non-experts could consequently be extrapolated to the general orthopedic surgeon. Perhaps the knowledge gaps in present study would be even more profound in those who are not a member of a knee association.
Conclusion
In the absence of a nationwide cartilage repair registry, this survey gives an impression of cartilage repair in the Netherlands. The present survey study showed that cartilage defects are treated by experts and many by non-experts. Both groups revealed a relative adherence to (inter)national guidelines. Small (< 2 cm2) and simple cartilage defects in the absence of additional injuries or malalignment may therefore be treated by general orthopedic surgeons if they follow the latest national recommendations. However, several knowledge gaps for specific defect and patient characteristics were shown, indicating that not everyone is fully aware of the latest insights. Caution should be exercised concerning the opportunistic use of MF, treating rare defects such as defects > 2 cm2 or those in the presence of loose viable cartilage bodies. Particularly patients with suboptimal characteristics such as an increased age (> 40 years), high BMI or malalignment should be considered for referral. This survey indicated that the recently introduced centralization of cartilage care is widely adopted in the Netherlands, which potentially aids in better knowhow and availability of advanced treatments, consequently better outcomes, and perhaps, joint preservation. Future research should focus more on dominant demographics such as older patients with typical comorbidities. This study should encourage orthopedic surgeons to engage in (inter-) national cartilage registries. Combining these registries with the Dutch Arthroplasty Register could aid in understanding the conversions to arthroplasties. Structural support from both the government and industry is necessary to enable the proper registration of all cartilage surgeries and products.
Data availability
Data from this study can be made available by authors upon request.
References
Heir S et al (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38(2):231–237
Makris EA et al (2015) Repair and tissue engineering techniques for articular cartilage. Nat Rev Rheumatol 11(1):21–34
Jeuken RM et al (2021) A systematic review of focal cartilage defect treatments in middle-aged versus younger patients. Orthop J Sports Med 9(10):23259671211031244
Jeuken RM et al (2016) Polymers in cartilage defect repair of the knee: current status and future prospects. Polymers (Basel) 8(6):219
Caron JJ, CRJH, Emans PJ (2019) Chirurgische behandeling van (osteo)chondrale defecten in de knie. Nederlandse Orthopaedische Vereniging. https://www.orthopeden.org/downloads/761/standpunt-chirurgische-behandeling-osteochondrale-defecten-knie.pdf (orthopeden.org)
Barber RM et al (2017) Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet 390(10091):231–266
Draugalis JR, Coons SJ, Plaza CM (2008) Best practices for survey research reports: a synopsis for authors and reviewers. Am J Pharm Educ 72(1):11
Meyer VM et al (2020) Global overview of response rates in patient and health care professional surveys in surgery: a systematic review. Ann Surg 275:e75
Sheehan KB (2001) E-mail survey response rates: a review. J Comput Mediat Commun 6(2):0–0
Widuchowski W, Widuchowski J, Trzaska T (2007) Articular cartilage defects: study of 25,124 knee arthroscopies. Knee 14(3):177–182
DeFroda SF et al (2020) Trends in the surgical treatment of articular cartilage lesions in the United States from 2007 to 2016. J Knee Surg 34:1609
McCormick F et al (2014) Trends in the surgical treatment of articular cartilage lesions in the United States: an analysis of a large private-payer database over a period of 8 years. Arthroscopy 30(2):222–226
Montgomery SR et al (2014) Trends in the surgical treatment of articular cartilage defects of the knee in the United States. Knee Surg Sports Traumatol Arthrosc 22(9):2070–2075
Niemeyer P et al (2016) Cartilage repair surgery for full-thickness defects of the knee in Germany: indications and epidemiological data from the German Cartilage Registry (KnorpelRegister DGOU). Arch Orthop Trauma Surg 136(7):891–897
Elmali N et al (2016) Cartilage repair strategies in the knee: a survey of Turkish surgeons. Acta Orthop Traumatol Turc 50(5):533–538
Salzmann GM et al (2011) Cartilage repair approach and treatment characteristics across the knee joint: a European survey. Arch Orthop Trauma Surg 131(3):283–291
Lacy KW et al (2016) Medial femoral condyle cartilage defect biomechanics: effect of obesity, defect size, and cartilage thickness. Am J Sports Med 44(2):409–416
Chahal J et al (2013) Managing the patient with failed cartilage restoration. Sports Med Arthrosc Rev 21(2):62–68
Crowninshield RD, Rosenberg AG, Sporer SM (2006) Changing demographics of patients with total joint replacement. Clin Orthop Relat Res 443:266–272
Zellner J et al (2021) Current practice of concomitant surgeries in cartilage repair of the femorotibial compartment of the knee: baseline data of 4968 consecutive patients from the German cartilage registry (KnorpelRegister DGOU). Arch Orthop Trauma Surg
Brophy RH et al (2010) Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: incidence and treatment. Arthroscopy 26(1):112–120
Weber AE et al (2016) Malalignment: a requirement for cartilage and organ restoration. Sports Med Arthrosc Rev 24(2):e14-22
Faber S et al (2021) Comparison of clinical outcome following cartilage repair for patients with underlying varus deformity with or without additional high tibial osteotomy: a propensity score-matched study based on the German Cartilage Registry (KnorpelRegister DGOU). Cartilage 13(1_suppl):1206S-1216S
Sofu H et al (2022) Lesion size and varus malalignment are the major determinants leading to poorer clinical outcomes after combined microfracture treatment for focal cartilage lesions during anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg 142(8):1941–1949
Rosenberger RE et al (2008) Repair of large chondral defects of the knee with autologous chondrocyte implantation in patients 45 years or older. Am J Sports Med 36(12):2336–2344
Waller C et al (2011) Unload it: the key to the treatment of knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 19(11):1823–1829
van der Linden MH et al (2013) Treatment of cartilaginous defects in the knee: recommendations from the Dutch Orthopaedic Association. Ned Tijdschr Geneeskd 157(3):A5719
Hulet C, Pereira H, Peretti G, Denti M (eds) (2016) Surgery of the meniscus. Springer, London
Curl WW et al (1997) Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy 13(4):456–460
Mestriner AB, Ackermann J, Gomoll AH (2018) Patellofemoral cartilage repair. Curr Rev Musculoskelet Med 11(2):188–200
Wang KC, Frank RM, Cole BJ (2019) Tibial cartilage defects. In: Yanke AB, Cole BJ (eds) Joint preservation of the knee: a clinical casebook. Springer, Cham, pp 255–265
Jeuken RM et al (2019) The modified hedgehog technique to repair pure chondral shear-off lesions in the pediatric knee. Cartilage 13:1947603519855762
Bonasia DE et al (2015) Use of chondral fragments for one stage cartilage repair: a systematic review. World J Orthop 6(11):1006–1011
Bayliss LE et al (2017) The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet 389(10077):1424–1430
Engen CN, Engebretsen L, Aroen A (2010) Knee cartilage defect patients enrolled in randomized controlled trials are not representative of patients in orthopedic practice. Cartilage 1(4):312–319
Kraus VB, Karsdal MA (2020) Osteoarthritis: current molecular biomarkers and the way forward. Calcif Tissue Int 109:329
Tempelaar D, Rienties B, Nguyen Q (2020) Subjective data, objective data and the role of bias in predictive modelling: Lessons from a dispositional learning analytics application. PLoS ONE 15(6):e0233977
Acknowledgements
We gratefully acknowledge the Nederlandse Vereniging voor Orthopedie (NOV), Dutch Knee Society (DKS) and Nederlandse Vereniging voor Arthroscopie (NvA) for providing the correspondence details of all the Dutch orthopedic knee specialists.
Funding
There was no funding applicable to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R.M. Jeuken, P.P.W. Van Hugten, A. K. Roth, T.A.E.J. Boymans, J. Caron A. Weber R.J.H. Custers and P.J. Emans do not have any conflict of interest.
Ethical approval
Since there were no study subjects and participation to the survey was voluntary, there was no ethical committee involved. This study was conducted in accordance with the World Medical Association Declaration of Helsinki.
Informed consent
Participation to the survey was voluntary, and respondents were anonymized. Respondents were informed prior to the survey that the results would be made available for international publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1: Survey questions
Appendix 1: Survey questions
General
-
1.
You are:
-
(a)
Orthopedic surgeon
-
(b)
Resident
-
(a)
-
2.
I use the following techniques for cartilage repair of symptomatic cartilage defects: (multiple answers possible)
-
(a)
Debridement/nettoyage
-
(b)
Microfracture
-
(c)
Autologous Chondrocyte Implantation (all generations)
-
(d)
Microfracture augmentations (such as Autologous Matrix-Induced Chondrogenesis [AMIC])
-
(e)
Osteochondral Allografts
-
(f)
Mosaicplasty (Osteochondral Autograft Transfer System [OATS])
-
(g)
Non-degradable cartilage implants (Metal/Polymer)
-
(h)
Biodegradable osteochondral scaffolds (such as Trufit™, MaioRegen, Agili-C™)
-
(a)
-
3.
My experience with the treatment of cartilage defects is:
-
(a)
None
-
(b)
0–1 year
-
(c)
1–5 year
-
(d)
> 5 years
-
(a)
-
4.
Approximately how many cartilage defects have you treated in the past year? (open)
-
5.
In general I treat cartilage defects within the following age categories: (multiple answers possible)
-
(a)
< 18 years
-
(b)
18–30 years
-
(c)
30–40 years
-
(d)
40–60 years
-
(e)
> 60 years
-
(a)
-
6.
I carry out cartilage repair in patients who smoke:
-
(a)
Yes
-
(b)
No
-
(a)
-
7.
When treating cartilage defects, I apply an upper limit for BMI (kg/m2) of:
-
(a)
≤ 25
-
(b)
< 30
-
(c)
< 35
-
(d)
< 40
-
(e)
No limit
-
(a)
-
8.
I apply cartilage repair to the following compartments of the knee: (multiple answers possible)
-
(a)
Medial femoral condyle
-
(b)
Lateral femoral condyle
-
(c)
Trochlea
-
(d)
Patella
-
(e)
Tibia plateau
-
(a)
-
9.
Within the same knee I would address: (multiple answers possible)
-
(a)
Single lesions
-
(b)
Multiple lesions
-
(c)
Kissing lesions
-
(a)
-
10.
In patients with a symptomatic cartilage defect I apply the following techniques in addition to cartilage repair: (multiple answers possible)
-
(a)
Surgical correction leg axis (tibiofemoral and patellofemoral)
-
(b)
Ligamental correction (cruciate, medial patellofemoral ligament, collaterals)
-
(c)
Meniscus surgery (nettoyage, sutures, allograft implants)
-
(d)
Other (please elaborate)
-
(a)
-
11.
Starting from how many degrees (varus/valgus) would you carry out a surgical correction of the leg axis?: (open)
-
12.
I refer patients to one of the specialized centers:
-
(a)
Yes
-
(b)
No
-
(c)
I work in such a center myself
-
(a)
Specific
-
13.
I would treat symptomatic, ICRS grade 1/2, cartilage defects with a maximum size of, with the following techniques: (multiple answers possible)
< 1 cm2 | 1–2 cm2 | 2–3 cm2 | 3–4 cm2 | > 4 cm2 | Not | |
|---|---|---|---|---|---|---|
Debridement/nettoyage | ||||||
Microfracture | ||||||
Autologous chondrocyte implantation (all generations) | ||||||
Microfracture augmentations [(such as autologous matrix-induced chondrogenesis (AMIC)] | ||||||
Osteochondral allografts | ||||||
Mosaicplasty [osteochondral autograft transfer system (OATS)] | ||||||
Non-degradable cartilage implants (metal/polymer) | ||||||
biodegradable osteochondral scaffolds (e.g., Trufit™, MaioRegen, Agili-C™) |
-
14.
I would treat symptomatic, ICRS grade 3/4, cartilage defects with a maximum size of, with the following techniques: (multiple answers possible)
< 1 cm2 | 1–2 cm2 | 2–3 cm2 | 3–4 cm2 | > 4 cm2 | Not | |
|---|---|---|---|---|---|---|
Debridement/nettoyage | ||||||
Microfracture | ||||||
Autologous chondrocyte implantation (all generations) | ||||||
Microfracture augmentations [such as autologous matrix-induced chondrogenesis (AMIC)] | ||||||
Osteochondral allografts | ||||||
mosaicplasty [osteochondral autograft transfer system (OATS)] | ||||||
Non-degradable cartilage implants (metal/polymer) | ||||||
Biodegradable osteochondral scaffolds (as Trufit™, MaioRegen, Agili-C™) |
-
15.
I would treat deep cartilage defects myself (ICRS grade 5/deeper than 6.5 mm):
-
(a)
Yes
-
(b)
No
-
(a)
-
16.
In case of a cartilage corpus liberum I attempt refixation: (multiple answers possible)
-
(a)
No
-
(b)
Yes in case of an osteochondral corpus liberum
-
(c)
Yes in case of a chondral corpus liberum
-
(a)
-
17.
I would consider the following techniques for the following age categories, irrespective of ICRS grade): (multiple answers possible)
< 10 years of age | 10–20 years of age | 20–30 years of age | 30–40 years of age | 40–50 years of age | 60–70 years of age | > 70 years of age | |
|---|---|---|---|---|---|---|---|
Debridement/nettoyage | |||||||
Microfracture | |||||||
Autologous Chondrocyte Implantation (all generations) | |||||||
Microfracture augmentations [such as autologous matrix-induced chondrogenesis (AMIC)] | |||||||
Osteochondral Allografts | |||||||
Mosaicplasty [osteochondral autograft transfer system (OATS)] | |||||||
Non-degradable cartilage implants (Metal/Polymer) | |||||||
Biodegradable osteochondral scaffolds (such as Trufit™, MaioRegen, Agili-C™) |
-
18.
I consider the effect of middle age (40–65 year) on the success rate on the following techniques to be:
Low | Average | High | |||
|---|---|---|---|---|---|
1 | 2 | 3 | 4 | 5 | |
Debridement/nettoyage | |||||
Microfracture | |||||
Autologous chondrocyte implantation (all generations) | |||||
Microfracture augmentations [such as autologous matrix-induced chondrogenesis (AMIC)] | |||||
Osteochondral Allografts | |||||
Mosaicplasty [osteochondral autograft transfer system (OATS)] | |||||
Non-degradable cartilage implants (metal/polymer) | |||||
Biodegradable osteochondral scaffolds (such as Trufit™, MaioRegen, Agili-C™) | |||||
-
19.
My clinic has a specific cartilage repair rehabilitation protocol
-
(a)
No
-
(b)
Yes, please elaborate (brace, loading etc.)
-
(a)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jeuken, R.M., van Hugten, P.P.W., Roth, A.K. et al. Cartilage repair strategies in the knee according to Dutch Orthopedic Surgeons: a survey study. Arch Orthop Trauma Surg 143, 5175–5188 (2023). https://doi.org/10.1007/s00402-023-04800-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04800-6