Abstract
Purpose
The recreational and medical use of cannabis is being legalized worldwide. Its use has been linked to an increased risk of developing opioid use disorders. As opioids continue to be prescribed after total hip arthroplasty (THA), the influence that preoperative cannabis use may have on postoperative opioid consumption remains unknown. The purpose of this study was to assess the relationship between preoperative cannabis use and opioid utilization following primary THA.
Methods
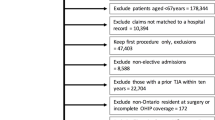
We identified all patients over the age of 18 who underwent unilateral, primary THA for a diagnosis of osteoarthritis at a single institution from February 2019 to April 2021. Our cohort was grouped into current cannabis users (within 6 months of surgery) and those who reported never using cannabis. One hundred and fifty-six current users were propensity score matched 1:6 with 936 never users based on age, sex, BMI, history of chronic pain, smoking status, history of anxiety/depression, ASA classification and type of anesthesia. Outcomes included inpatient and postdischarge opioid use in morphine milligram equivalents.
Results
Total inpatient opioid utilization, opioids refilled, and total opioids used within 90 postoperative days were similar between the groups.
Conclusion
In propensity score matched analyses, preoperative cannabis use was not independently associated with an increase in inpatient or outpatient, 90-days opioid consumption following elective THA.
Similar content being viewed by others
References
Swift A (2013) For first time, Americans favor legalizing marijuana. Gallup Politics, 2019–02
Coffman KL (2008) The debate about marijuana usage in transplant candidates: recent medical evidence on marijuana health effects. Curr Opin Organ Transplant 13(2):189–195. https://doi.org/10.1097/MOT.0b013e3282f56139
Jennings JM, Williams MA, Levy DL, Johnson RM, Eschen CL, Dennis DA (2019) Has self-reported marijuana use changed in patients undergoing total joint arthroplasty after the legalization of marijuana? Clin Orthop Relat Res 477(1):95. https://doi.org/10.1097/CORR.0000000000000339
Deckey DG, Lara NJ, Gulbrandsen MT, Hassebrock JD, Spangehl MJ, Bingham JS (2021) Prevalence of cannabinoid use in patients with hip and knee osteoarthritis. J Am Acad Orthop Surg Glob Res Rev 5(2):e20.00172. https://doi.org/10.5435/JAAOSGlobal-D-20-00172
Gellad WF, Good CB, Shulkin DJ (2017) Addressing the opioid epidemic in the United States: lessons from the Department of Veterans Affairs. JAMA Intern Med 177(5):611–612. https://doi.org/10.1001/jamainternmed.2017.0147
Anand U, Pacchetti B, Anand P, Sodergren MH (2021) Cannabis-based medicines and pain: a review of potential synergistic and entourage effects. Pain Manag 11(4):395–403. https://doi.org/10.2217/pmt-2020-0110
Olfson M, Wall MM, Liu SM, Blanco C (2018) Cannabis use and risk of prescription opioid use disorder in the United States. Am J Psychiatry 175(1):47–53. https://doi.org/10.1176/appi.ajp.2017.17040413
Wilson J, Mills K, Freeman TP, Sunderland M, Visontay R, Marel C (2021) Weeding out the truth: a systematic review and meta-analysis on the transition from cannabis use to opioid use and opioid use disorders, abuse or dependence. Addiction. https://doi.org/10.1111/add.15581
Jennings JM, McNabb DC, Johnson RM, Brady AC, Kim RH, Dennis DA (2022) Use of cannabis does not decrease opioid consumption in patients who underwent total joint arthroplasty. Arthroplasty today 15:141–146. https://doi.org/10.1016/j.artd.2022.03.018
Wu L, Li M, Zeng Y, Si H, Liu Y, Yang P, Shen B (2021) Prevalence and risk factors for prolonged opioid use after total joint arthroplasty: a systematic review, meta-analysis, and meta-regression. Arch Orthop Trauma Surg 141(6):907–915. https://doi.org/10.1007/s00402-020-03486-4
Huang PS, Copp SN (2019) Oral opioids are overprescribed in the opiate-naive patient undergoing total joint arthroplasty. J Am Acad Orthop Surg 27(15):e702–e708. https://doi.org/10.5435/JAAOS-D-18-00404
Liu CW, Bhatia A, Buzon-Tan A, Walker S, Ilangomaran D, Kara J et al (2019) Weeding out the problem: the impact of preoperative cannabinoid use on pain in the perioperative period. Anesth Analg 129(3):874–881. https://doi.org/10.1213/ANE.0000000000003963
Hickernell TR, Lakra A, Berg A, Cooper HJ, Geller JA, Shah RP (2018) Should cannabinoids be added to multimodal pain regimens after total hip and knee arthroplasty? J Arthroplasty 33(12):3637–3641. https://doi.org/10.1016/j.arth.2018.07.027
Runner RP, Luu AN, Nassif NA, Scudday TS, Patel JJ, Barnett SL, Gorab RS (2020) Use of tetrahydrocannabinol and cannabidiol products in the perioperative period around primary unilateral total hip and knee arthroplasty. J Arthroplasty 35(6):S138–S143. https://doi.org/10.1016/j.arth.2020.01.077
Morrow M (2020) The effects of cannabinoid use on acute orthopaedic pain: a review of the current literature. JBJS J Orthop Phys Assist 8(2):e0006. https://doi.org/10.2106/JBJS.JOPA.20.00006
Yu JS, Premkumar A, Liu S, Sculco P (2021) Rates of self-directed perioperative cannabidiol use in patients undergoing total hip or knee arthroplasty. Pain Manage. https://doi.org/10.2217/pmt-2021-0018
Kelly P, Jones RT (1992) Metabolism of tetrahydrocannabinol in frequent and infrequent marijuana users. J Anal Toxicol 16(4):228–235. https://doi.org/10.1093/jat/16.4.228
Aleissa MM, Ahern KL, Stern GM (2020) Peri-operative opioid and sedation requirements in patients who use marijuana and are undergoing total knee or total hip arthroplasty: a retrospective study. J Clin Anesth 66:109953–109953. https://doi.org/10.1016/j.jclinane.2020.109953
Chalmers BP, Lebowitz J, Chiu YF, Joseph AD, Padgett DE, Bostrom MP, Valle AGD (2021) Changes in opioid discharge prescriptions after primary total hip and total knee arthroplasty affect opioid refill rates and morphine milligram equivalents: an institutional experience of 20,000 patients. Bone Joint J 103(7 Supple B):103–110. https://doi.org/10.1302/0301-620X.103B7.BJJ-2020-2392.R1
Kandel DB (2003) Does marijuana use cause the use of other drugs? JAMA 289(4):482–483. https://doi.org/10.1001/jama.289.4.482
Salottolo K, Peck L, Tanner Ii A, Carrick MM, Madayag R, McGuire E, Bar-Or D (2018) The grass is not always greener: a multi-institutional pilot study of marijuana use and acute pain management following traumatic injury. Patient Saf Surg 12(1):1–8. https://doi.org/10.1186/s13037-018-0163-3
Tanda G, Pontieri FE, Chiara GD (1997) Cannabinoid and heroin activation of mesolimbic dopamine transmission by a common µ1 opioid receptor mechanism. Science 276(5321):2048–2050. https://doi.org/10.1126/science.276.5321.2048
Goesling J, Moser SE, Zaidi B, Hassett AL, Hilliard P, Hallstrom B et al (2016) Trends and predictors of opioid use following total knee and total hip arthroplasty. Pain 157(6):1259. https://doi.org/10.1097/j.pain.0000000000000516
Kugelman DN, Mahure SA, Feng JE, Rozell JC, Schwarzkopf R, Long WJ (2021) Total knee arthroplasty is associated with greater immediate post-surgical pain and opioid use than total hip arthroplasty. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03951-8
Giordano NA, Highland KB, Nghiem V, Scott-Richardson M, Kent M (2021) Predictors of continued opioid use 6 months after total joint arthroplasty: a multi-site study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04261-9
Urits I, Gress K, Charipova K, Habib K, Lee D, Lee C, Jung JW, Kassem H, Cornett E, Paladini A, Varrassi G, Kaye AD, Viswanath O (2020) Use of cannabidiol (CBD) for the treatment of chronic pain. Best Pract Res Clin Anaesthesiol 34(3):463–477. https://doi.org/10.1016/j.bpa.2020.06.004
Bolarinwa SA, Casp AA, Cancienne JM, Werner BC, Browne JA (2019) Narcotic use and total hip arthroplasty. HIP Int 29(4):379–384. https://doi.org/10.1177/1120700018781759
Acknowledgements
This study was funded by the generous donations of Mr. Kim Davis and Mr. Baryn Futa. We are grateful to the members of the HSS ARJR Perioperative Outcomes Group who contributed to the design of this study and to the surgeons of the ARJR Service who contributed patients to this study.
Funding
Author Alejandro Gonzalez Della Valle received research support from company Naviswiss. This research was partially funded by donations from Mr. Kim Davis and Mr. Baryn Futa. Myself and my co-authors have the following disclosures to report: Author Alejandro Gonzalez Della Valle received royalties from company Orthodevelopment-Stryker. Author Alejandro Gonzalez Della Valle is a paid consultant for companies Link Bio, Johnson and Johnson and Naviswiss.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by CO. Data analysis was performed by Y-FC. The first draft of the manuscript was written by CO and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no relevant conflicts of interest to disclose.
Ethical approval
The methodology for this study was approved by the Human Research Ethics Committee/Institutional Review Board of our institution.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of their deidentified medical data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ong, C.B., Puri, S., Lebowitz, J. et al. Preoperative cannabis use does not increase opioid utilization following primary total hip arthroplasty in a propensity matched analysis. Arch Orthop Trauma Surg 143, 3629–3635 (2023). https://doi.org/10.1007/s00402-022-04619-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04619-7


