Abstract
Introduction
Treatment of older adult hip fracture patients can be challenging and requires early postoperative mobilisation to prevent complications. Simple clinical tools to predict mobilisation/weight-bearing difficulties after hip fracture surgery are scarcely available and analysis of handgrip strength could be a feasible approach. In the present study, we hypothesised that patients with reduced handgrip strength show incapability to follow postoperative weight-bearing instructions.
Materials and methods
Eighty-four patients aged ≥ 65 years with a proximal femur fracture (trochanteric, n = 45 or femoral neck, n = 39), who were admitted to a certified orthogeriatric center, were consecutively enrolled in a prospective study design. Five days after surgery (intramedullary nailing or arthroplasty), a standardised assessment of handgrip strength and a gait analysis (via insole forcesensors) was performed.
Results
Handgrip strength showed positive correlation with average peak force during gait on the affected limb (0.259), postoperative Parker Mobility Score (0.287) and Barthel Index (0.306). Only slight positive correlation was observed with gait speed (0.157). These results were congruent with multivariate regression analysis.
Conclusion
Assessment of handgrip strength is a simple and reliable tool for early prediction of postoperative mobilisation complications like the inability to follow weight-bearing instructions in older hip fracture patients. Follow-up studies should evaluate if these findings also match with other fracture types and result in personalised adjustment of current aftercare patterns. In addition, efforts should be made to combine objectively collected data as handgrip strength or gait speed in a prediction model for long-term outcome of orthogeriatric patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are a life-changing event especially in older people and are associated with a high risk of mortality. According to latest epidemiologic data, related health loss expressed as disease adjusted life years (DALY) is expected to double from 2020 to 2040 [6]. At worst, an independent and mobile person becomes completely dependent on external help after suffering a hip fracture [28]. This is explained by the complexity of these patients: age-related physiological changes and various comorbidities like sarcopenia, visual impairment or cardiovascular diseases aggravate a return to the prefracture status of mobility and independency in activities of daily living (ADL).
Different forms of orthogeriatric treatment were implemented over the last years to address these special needs and to improve outcome of elderly trauma patients [21]. One main treatment goal of this interdisciplinary approach is early mobilisation with full weight-bearing after surgery, as immobilisation leads to complications like pneumonia, urinary tract infections or muscle atrophy associated with an increased mortality [1, 8, 18].
To assess individuals’ status of mobility and activities of daily living, various scores like Parker Mobility Score or Barthel Index are approved for a long time [16, 20]. Although these scores are frequently used, they only represent subjective tests and are dependent on the cooperation of the patient. Especially with regard to physical activity, various studies indicate that there are discrepancies between questionnaires and objective measurements of physical activity and patients significantly overestimated their daily activities [12, 26]. To address the needs of elderly hip fracture patients sufficiently, objective parameters for evaluation of individual mobility and mobilisation are essential. Real-time assessment of weight-bearing on the affected limb with insole force sensors has proven to be a feasible approach and provides objective data as well as a biofeedback. Braun et al. could demonstrate, using these sensors, that adherence to weight-bearing instructions in elderly trauma patients is low [2]. Although full weight-bearing is generally the aim after hip fracture surgery in these patients, some fracture patterns require modification of weight-bearing instructions. Thus, early identification of patients at risk to follow weight-bearing instructions would be desirable, as it might change the choice of treatment.
Besides gait speed, which has shown a significant correlation with the risk of mortality, handgrip strength appears as a promising value to predict outcome in elderly patients [17, 27, 29]. It is commonly used as a simple clinical parameter for physical function and muscle strength assessment [7]. Following the European Working Group on Sarcopenia in Older People 2 (EWGSOP2) also probable presence of sarcopenia can be defined herewith [4]. Furthermore, handgrip strength was proven as prognostic factor after hip fracture surgery [5, 23].
The aim of this study was to connect these parameters and to evaluate if patients with deficient handgrip strength also show deficits to follow postoperative weight-bearing instructions. We hypothesised that correlation between handgrip strength, objective (weight-bearing on affected limb, postoperative gait speed) and subjective parameters (mobility/ADL scores) helps to identify patients at risk for mobilisation complications after hip fracture surgery.
Methods
Study population
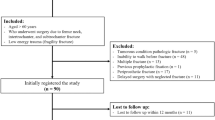
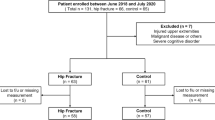
All patients aged 65 years and older, who were admitted to our certified orthogeriatric unit at a level-one trauma center with a proximal femur fracture (femoral neck or trochanteric region) between October 2017 and April 2018 were consecutively included in this prospective observational study after written informed consent. The study followed the Declaration of Helsinki and was registered at the German Clinical Trials Register (DRKS) under DRKS00012800 after approval of the local ethics review committee (Ref.-No.: 214-16). Instructions of the STROBE panel were followed for arrangement of this manuscript.
Exclusion criteria were fracture fixation of a femoral neck fracture, cognitive disorders (dementia, delirium, etc., defined by Mini-Mental State Examination < 26), language barrier, preexisting immobility and additional fractures of the upper or lower extremity.
Standardised and validated questionnaires were used to asses cognitive impairment (Mini-Mental State Examination), mobility and activities of daily living prior/after fracture [Parker Mobility Score (PMS)/Barthel Index (BI)]. Correct understanding and answering was verified by explicit inquiries for each patient.
Surgical treatment of trochanteric fractures was performed by intramedullary nailing [PFNA (Proximal Femoral Nail Antirotation); DePuy Synthes, Umkirch, Germany], femoral neck fractures were treated by arthroplasty (in case of total hip replacement: pinnacle acetabular cup, Biolox femoral head and Corail cemented stem/in case of bipolar hemiarthroplasty cemented Corail stem; DePuy Synthes, Umkirch, Germany).
On the first day after hip fracture surgery, all included patients were mobilised by physiotherapists with full weight-bearing as possible and training was continued each day. No other mobility restrictions were recommended, all patients received same postoperative care including standardised pain medication following WHO treatment guidelines, which was adjusted individually to facilitate painless walking.
Assessment of handgrip strength and gait analysis
Standardised assessment was performed for handgrip strength and gait analysis on the fifth postoperative day. Handgrip strength was measured with a JAMAR Hydraulic Hand Dynamometer (Sammons Preston Inc., Bolinbrook, IL, USA) at the second handle position. Patients were in seating position, shoulder adducted and in neutral rotation, elbow flexed at 90 degrees, wrist between 0 and 30 degrees of flexion and between 0 and 15 degrees of ulnar deviation. Following instruction through the physiotherapy staff, three attempts of maximal voluntary squeezing were performed on both hands and highest result of dominant hand used for statistical analysis. Cut-off for probable presence of sarcopenia was set at 16 kg for woman/27 kg for men regarding to EWGSOP2 recommendation.
Insole force sensors (loadsoal®, Novel GmbH, Germany), fitted to the individuals foot size were placed in both shoes and used for gait analysis on a predefined walk of 40 m distance (starting from a chair, level walking, turning and returning to the chair). If necessary, the patient could use a walking aid of choice. Real-time data transmission (via Bluetooth to a tablet computer) of multiple parameters like gait speed, average peak force (average of maximum force values over the entire gait analysis in each step) and loading rate for each foot allows immediate analysis and storage (Fig. 1). Plantar force (in N) was measured in static and dynamic situations, the foot was scanned with up to 200 Hz and the capacitive sensors covered the complete plantar surface of the foot.
Statistical analysis
Statistical analysis was performed using R (R Core Team 2019, R Foundation for Statistical Computing, Vienna, Austria). Normally distributed continuous variables are reported as mean with standard deviation (SD), categorical data as absolute frequency with a percentage distribution. Pearson and Spearman correlation coefficients (depending on data distribution) were used to analyse the association of handgrip strength with postoperative mobility (PMS, BI, average peak force loading on the affected leg, gait speed). Additionally, multivariate linear regression analysis, adjusted for age, gender and BMI, was performed to evaluate the influence of handgrip strength. Significance was set at a level of α = 0.05.
Results
Study population
In total, 122 patients were screened for eligibility, 84 of them met the inclusion criteria. Mean age was 79.71 (SD ± 6.769) years, 66.7% (n = 56) were female. Average ASA score was 2.67 (SD ± 0.545) and mean BMI 23.195 (SD ± 3.76). Most of the patients used a walking aid for postoperative mobilisation, only 4.8% were able to walk free. Barthel Index and Parker Mobility Score decreased significantly compared to prefracture/-operative status. A mean handgrip strength of 19.275 kg (SD ± 7,138) was observed, 59.5% (n = 50) of the patients were defined for probable presence of sarcopenia according to the EWGSOP2 criteria (see Table 1 for additional information).
Radiographic examination presented good implant positioning and fracture reduction in all patients, no wound healing disorder or other condition preventing mobilisation occurred during clinical course.
Association of handgrip strength and postoperative mobilisation/mobility parameters
Handgrip strength showed positive correlation with average peak force loading on the affected limb (Fig. 2), postoperative PMS and BI (see Table 2 for detailed information). Only slight positive correlation was observed between handgrip strength and postoperative gait speed. These findings were congruent with multivariate regression analysis (see Table 3 for detailed information).
Discussion
Prompt mobilisation with adherence to weight-bearing instructions is essential to avoid in-hospital and long-term complications of older hip fracture patients. Early objective detection of patients at risk for mobilisation complications therefore is crucial, yet it can be challenging at the same time. Given the findings of the present study, assessment of handgrip strength could be used as simple and easy to implement identification tool to predict difficulties in mobilisation/weight-bearing in elderly hip fracture patients.
More than half of the study population presented with probable concomitant sarcopenia regarding to the EWGSOP2 criteria. This is higher than recent studies assessed in the perioperative setting, but consistent with results in postoperative setting [3, 24]. The observed high prevalence could be one major reason for recurrent falls following hip fracture surgery. Therefore, our findings should lead to a higher awareness for the presence of sarcopenia in acute care setting of orthogeriatric patients. Following the EWGSOP2 criteria, in clinical practice, detection of low muscle strength is enough to start further assessment and interventions (evaluation of nutritional status, administration of high caloric food, specific designed exercise programs [13, 25]). To determine muscle mass more precisely and confirm the diagnosis of sarcopenia, CT-based measurements could be used in addition, as a CT scan is performed in numerous patients at admission for supplementary fracture pattern evaluation and therefore is easily available [22].
Positive correlation of handgrip strength with subjective and objective parameters of postoperative mobility (PMS, loading on affected leg) and activities of daily living (BI) was observed in the present study. Correlation with peak force loading indicates that patients with superior handgrip strength can bear more weight on the affected limb during mobilisation and are able to follow the instruction of full weight-bearing. Vice versa, patients with reduced handgrip strength are more likely incapable to follow these instructions and therefore at risk for inappropriate surgical treatment and aftercare. Depending on the fracture pattern, modification of treatment concepts could be necessary. There is large consensus that aftercare treatment of hip fracture patients should follow full weight-bearing instructions. Fracture fixation of tibia plateau or pilon fractures frequently requires partial weight-bearing, whereas compliance to recommended weight-bearing limits in older trauma patients is low [2]. Taking findings of the present study into account, patients with reduced preoperative handgrip strength should be considered for joint replacement or joint fusion surgery in these fracture patterns to allow full weight-bearing. While previous studies evaluating the adherence of older trauma patients to weight-bearing recommendations with force sensors showed smaller number of patients, this study provides objective insights in a larger collective [2, 9].
Other than expected handgrip strength showed only slight positive correlation with postoperative gait speed. This is in contrast to recent findings by Orwig et al. [19]. One possible explanation might be found in different times of acquisition; in the present study, gait speed was assessed five days after surgery when patients still suffer from pain and toddle with following slow gait speed, whereas the acquisition period by Orwig et al. was two and six months after surgery. Although early identification of delayed mobilisation is essential, which favours analysis five days after surgery, selective correlation of grip strength with gait analysis/relevant scores at this time has to be regarded as a weakness of the present study. For future studies, a longitudinal observation, from admission to hospital until retrieval of individuals’ status of mobility, would be desirable to prove results and encourage long-term prediction of outcome via handgrip strength analysis.
Future combination of objective parameters like gait speed, weight-bearing on the affected limb and handgrip strength could lead to a prediction model for postoperative and long-term mobility. As recurrent falls are common following hip fracture, this model could also be used for secondary fracture prevention by identification of patients with low muscle strength and gait speed [15]. Lindemann et al. could show, that simple assessment of gait speed by visual categorisation is possible with reliable results, so even smaller hospitals could use the prediction model without technical expense [14]. In consequence, this should affect aftercare of each patient and lead to an individualised treatment plan. Given current technological developments, also individualised feedback regarding the recovery process could be possible beyond hospital stay with wearable devices and connected apps in the long run [10]. Regarding to Klenk et al. sensor-based assessment of physical activity is applicable for individual progress monitoring and might become an effective approach to further improve outcome in hip fracture patients [11].
To the best of the authors knowledge, the present trial remains the first study in which handgrip strength assessment in hip fracture patients was correlated with objective weight-bearing data, obtained with mobile sensors. Key findings are positive correlation of handgrip strength with postoperative weight-bearing and mobility measurements. As a consequence, handgrip strength assessment should be performed for every orthogeriatric patient already at admission to identify patients at risk for mobilisation complications. In the future, it could be a predictive model for postoperative and long-term mobilisation and mobility, consisting of easily accessible parameters like gait speed, weight-bearing and handgrip strength.
References
Beliveau MM, Multach M (2003) Perioperative care for the elderly patient. Med Clin North Am 87(1):273–289
Braun BJ, Veith NT, Rollmann M et al (2017) Weight-bearing recommendations after operative fracture treatment-fact or fiction? Gait results with and feasibility of a dynamic, continuous pedobarography insole. Int Orthop 41(8):1507–1512
Chiles Shaffer N, Huang Y, Abraham DS et al (2020) Comparing longitudinal sarcopenia trends by definitions across men and women after hip fracture. J Am Geriatr Soc 68:1537
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48(1):16–31
Di Monaco M, Castiglioni C, De Toma E, Gardin L, Giordano S, Tappero R (2015) Handgrip strength is an independent predictor of functional outcome in hip-fracture women: a prospective study with 6 month follow-up. Medicine (Baltimore) 94(6):e542
Hagen G, Magnussen J, Tell G, Omsland T (2020) Estimating the future burden of hip fractures in Norway. A NOREPOS study Bone 131:115156
Hirschfeld HP, Kinsella R, Duque G (2017) Osteosarcopenia: where bone, muscle, and fat collide. Osteopor Int:J Established As Result Of Cooperation Between The European Foundation For Osteoporosis and the National Osteoporosis Foundation of the USA 28(10):2781–2790
Kamel HK, Iqbal MA, Mogallapu R, Maas D, Hoffmann RG (2003) Time to ambulation after hip fracture surgery: relation to hospitalization outcomes. J Gerontol A Biol Sci Med Sci 58(11):1042–1045
Kammerlander C, Pfeufer D, Lisitano LA, Mehaffey S, Bocker W, Neuerburg C (2018) Inability of older adult patients with hip fracture to maintain postoperative weight-bearing restrictions. The J Bone Joint Surg Am 100(11):936–941
Keppler AM, Holzschuh J, Pfeufer D et al (2020) Postoperative physical activity in orthogeriatric patients - new insights with continuous monitoring. Injury 51:628
Klenk J, Wekenmann S, Schwickert L, Lindemann U, Becker C, Rapp K (2019) Change of objectively-measured physical activity during geriatric rehabilitation. Sensors (Basel) 19(24):5451
Koolhaas CM, van Rooij FJ, Cepeda M, Tiemeier H, Franco OH, Schoufour JD (2018) Physical activity derived from questionnaires and wrist-worn accelerometers: comparability and the role of demographic, lifestyle, and health factors among a population-based sample of older adults. Clin Epidemiol 10:1–16
Lichtenberg T, von Stengel S, Sieber C, Kemmler W (2019) The favorable effects of a high-intensity resistance training on sarcopenia in older community-dwelling men with osteosarcopenia: the randomized controlled FrOST study. Clin Interv Aging 14:2173–2186
Lindemann U, Rapp K, Becker C (2019) A simple method to categorize gait speed of older persons based on visual inspection of stepping. Aging Clin Exp Res 31(12):1843–1846
Lloyd BD, Williamson DA, Singh NA et al (2009) Recurrent and injurious falls in the year following hip fracture: a prospective study of incidence and risk factors from the sarcopenia and hip fracture study. J Gerontol A Biol Sci Med Sci 64(5):599–609
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Mueller A, Hoefling HA, Muaremi A et al (2019) Continuous digital monitoring of walking speed in frail elderly patients: noninterventional validation study and longitudinal clinical trial. JMIR Mhealth Uhealth 7(11):e15191
Oldmeadow LB, Edwards ER, Kimmel LA, Kipen E, Robertson VJ, Bailey MJ (2006) No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg 76(7):607–611
Orwig D, Magaziner J, Fielding RA et al (2020) Application of SDOC cut-points for low muscle strength for recovery of walking speed after hip fracture. J Gerontol A Biol Sci Med Sci 75:1379
Parker MJ, Palmer CR (1993) A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br 75(5):797–798
Pioli G, Giusti A, Barone A (2008) Orthogeriatric care for the elderly with hip fractures: where are we? Aging Clin Exp Res 20(2):113–122
Poros B, Irlbeck T, Probst P et al (2019) Impact of pathologic body composition assessed by CT-based anthropometric measurements in adult patients with multiple trauma: a retrospective analysis. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-019-01264-5
Savino E, Martini E, Lauretani F et al (2013) Handgrip strength predicts persistent walking recovery after hip fracture surgery. Am J Med 126(12):1068–1075 ((e1061))
Selakovic I, Dubljanin-Raspopovic E, Markovic-Denic L et al (2019) Can early assessment of hand grip strength in older hip fracture patients predict functional outcome? PLoS ONE 14(8):e0213223
Sieber CC (2019) Malnutrition and sarcopenia. Aging Clin Exp Res 31(6):793–798
Sievi NA, Brack T, Brutsche MH et al (2017) Accelerometer- versus questionnaire-based assessment of physical activity and their changes over time in patients with COPD. Int J Chron Obstruct Pulmon Dis 12:1113–1118
Studenski S, Perera S, Patel K et al (2011) Gait speed and survival in older adults. JAMA 305(1):50–58
van Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ (2001) Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res 390:232–243
Veronese N, Stubbs B, Volpato S et al (2018) Association between gait speed with mortality, cardiovascular disease and cancer: a systematic review and meta-analysis of prospective cohort studies. J Am Med Dir Assoc 19(11):981–988 ((e987))
Acknowledgements
The authors would like to thank Maximilian Weigert, Statistical Consulting Unit StaBLab, LMU Munich, for his help and advice for statistical analysis.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study was approved by the ethics review committee of the Munich university, LMU (Ref.-No.: 214-16) and registered at the German Clinical Trials Register (DRKS) under DRKS00012800.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gleich, J., Pfeufer, D., Keppler, A.M. et al. Identification of hip fracture patients at risk for postoperative mobilisation complications via handgrip strength assessment. Arch Orthop Trauma Surg 142, 997–1002 (2022). https://doi.org/10.1007/s00402-021-03756-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03756-9