Abstract
Objective
The aim of the present study was to compare the morphometric differences between patients with or without anterior cruciate ligament (ACL) injury, and identify the anatomic risk factors associated with ACL injury in active individuals.
Methods
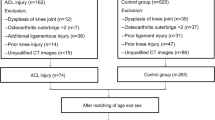
The knee joint magnetic resonance images (MRI) of 100 subjects were included in this study. Data from the ACL-injured group (50 patients) and matched controls (50 subjects) were obtained from the same hospital. These data were analyzed by univariable analysis or multivariable conditional logistic regression analysis to examine the effects of the following variables on the risk of suffering ACL injury for the first time: TT-TG distance, medial and lateral tibial slope, intercondylar notch width and depth, femur condylar width, lateral femoral condylar depth, notch width index (NWI), notch shape index (NSI), notch depth index (NDI), and cross-sectional area (CSA).
Results
In the univariable analysis, the ACL-injured group had a larger TT-TG distance, increased medial and lateral tibial slope, narrower intercondylar notch width, deeper lateral femoral condylar depth, lesser NWI and NSI, and CSA when compared with the control group (P < 0.05). However, there were no significant between-group differences in intercondylar notch depth (P = 0.174), femur condylar width (P = 0.797), and NDI (P = 0.436). The multivariable analysis revealed that TT-TG distance [odds ratio (OR) = 1.37, 95% CI = 1.04–1.81, P = 0.028], medial tibial slope (OR = 1.30, 95% CI = 1.02–1.66, P = 0.036) and NWI (OR = 0.46, 95% CI = 0.24–0.91, P = 0.025) had significant multivariable associations with the sole independent risk of ACL injury.
Conclusion
Larger TT-TG distance, increased MTS, and lesser NWI are independent anatomic risk factors for active individuals with ACL injury.
Level of evidence
Case-control study; Level of Evidence, III.




Similar content being viewed by others
References
Mehl J, Diermeier T, Herbst E, Imhoff AB, Stoffels T, Zantop T, Petersen W, Achtnich A, (2018) Evidence-based concepts for prevention of knee, and ACL injuries. (2017) guidelines of the ligament committee of the German knee society (DKG). Arch Orthop Trauma Surg 138(1):51–61. https://doi.org/10.1007/s00402-017-2809-5
Granan LP, Bahr R, Steindal K, Furnes O, Engebretsen L (2008) Development of a national cruciate ligament surgery registry: the Norwegian national knee ligament registry. Am J Sports Med 36(2):308–315. https://doi.org/10.1177/0363546507308939
Clayton RA, Court-Brown CM (2008) The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury 39(12):1338–1344. https://doi.org/10.1016/j.injury.2008.06.021
Maradit Kremers H, Bryan A, Larson D, Dahm D, Levy B, Stuart M, Krych A (2016) Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 44(6):1502–1507. https://doi.org/10.1177/0363546516629944
Barie A, Kopf M, Jaber A, Moradi B, Schmitt H, Huber J, Streich NA (2018) Long-term follow-up after anterior cruciate ligament reconstruction using a press-fit quadriceps tendon-patellar bone autograft. BMC Musculoskelet Disord 19(1):368. https://doi.org/10.1186/s12891-018-2271-8
Levine JW, Kiapour AM, Quatman CE, Wordeman SC, Goel VK, Hewett TE, Demetropoulos CK (2013) Clinically relevant injury patterns after an anterior cruciate ligament injury provide insight into injury mechanisms. Am J Sports Med 41(2):385–395. https://doi.org/10.1177/0363546512465167
Andriacchi TP, Briant PL, Bevill SL, Koo S (2006) Rotational changes at the knee after ACL injury cause cartilage thinning. Clin Orthopaedics Related Res 442:39–44. https://doi.org/10.1097/01.blo.0000197079.26600.09
Agel J, Arendt EA, Bershadsky B (2005) Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med 33(4):524–530. https://doi.org/10.1177/0363546504269937
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16(5):442–448. https://doi.org/10.1007/s00167-008-0498-x
Gottlob CA, Baker CL Jr (2000) Anterior cruciate ligament reconstruction: socioeconomic issues and cost effectiveness. Am J Orthopedics (Belle Mead, NJ) 29(6):472–476
Lohmander LS, Englund PM, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35(10):1756–1769. https://doi.org/10.1177/0363546507307396
Jaecker V, Zapf T, Naendrup JH, Kanakamedala AC, Pfeiffer T, Shafizadeh S (2018) Differences between traumatic and non-traumatic causes of ACL revision surgery. Arch Orthop Trauma Surg 138(9):1265–1272. https://doi.org/10.1007/s00402-018-2954-5
Alentorn-Geli E, Pelfort X, Mingo F, Lizano-Diez X, Leal-Blanquet J, Torres-Claramunt R, Hinarejos P, Puig-Verdie L, Monllau JC (2015) An evaluation of the association between radiographic intercondylar notch Narrowing and anterior cruciate ligament injury in men: the notch angle is a better parameter than notch width. Arthroscopy 31(10):2004–2013. https://doi.org/10.1016/j.arthro.2015.04.088
Al-Saeed O, Brown M, Athyal R, Sheikh M (2013) Association of femoral intercondylar notch morphology, width index and the risk of anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 21(3):678–682. https://doi.org/10.1007/s00167-012-2038-y
Beynnon BD, Hall JS, Sturnick DR, Desarno MJ, Gardner-Morse M, Tourville TW, Smith HC, Slauterbeck JR, Shultz SJ, Johnson RJ, Vacek PM (2014) Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of noncontact ACL injury in females but not in males: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med 42(5):1039–1048. https://doi.org/10.1177/0363546514523721
Dare DM, Fabricant PD, McCarthy MM, Rebolledo BJ, Green DW, Cordasco FA, Jones KJ (2015) Increased lateral tibial slope is a risk factor for pediatric anterior cruciate ligament injury: an MRI-based case-control study of 152 patients. Am J Sports Med 43(7):1632–1639. https://doi.org/10.1177/0363546515579182
Geng B, Wang J, Ma JL, Zhang B, Jiang J, Tan XY, Xia YY (2016) Narrow intercondylar notch and anterior cruciate ligament injury in female nonathletes with knee osteoarthritis aged 41–65 years in plateau region. Chin Med J 129(21):2540–2545. https://doi.org/10.4103/0366-6999.192771
Rahnemai-Azar AA, Yaseen Z, van Eck CF, Irrgang JJ, Fu FH, Musahl V (2016) Increased lateral tibial plateau slope predisposes male college football players to anterior cruciate ligament injury. J Bone Joint Surg Am 98(12):1001–1006. https://doi.org/10.2106/JBJS.15.01163
Saper MG, Popovich JM Jr, Fajardo R, Hess S, Pascotto JL, Shingles M (2016) The Relationship between tibial tubercle-trochlear groove distance and noncontact anterior cruciate ligament injuries in adolescents and young adults. Arthroscopy 32(1):63–68. https://doi.org/10.1016/j.arthro.2015.06.036
Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM (2010) A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech 43(9):1702–1707. https://doi.org/10.1016/j.jbiomech.2010.02.033
van Eck CF, Martins CA, Vyas SM, Celentano U, van Dijk CN, Fu FH (2010) Femoral intercondylar notch shape and dimensions in ACL-injured patients. Knee Surg Sports Traumatol Arthrosc 18(9):1257–1262. https://doi.org/10.1007/s00167-010-1135-z
Souryal T, Freeman T (1993) Intercondylar notch size and anterior cruciate ligament injuries in athletes. A prospective study. Am J Sports Med 21 (4):535–539
Chandrashekar N, Mansouri H, Gill B, Slauterbeck J, Schutt R, Dabezies E, Beynnon B (2010) Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med 38(1):54–62. https://doi.org/10.1177/0363546509349055
Evans KN, Kilcoyne KG, Dickens JF, Rue JP, Giuliani J, Gwinn D, Wilckens JH (2012) Predisposing risk factors for non-contact ACL injuries in military subjects. Knee Surg Sports Traumatol Arthrosc 20(8):1554–1559. https://doi.org/10.1007/s00167-011-1755-y
Sturnick DR, Vacek PM, DeSarno MJ, Gardner-Morse MG, Tourville TW, Slauterbeck JR, Johnson RJ, Shultz SJ, Beynnon BD (2015) Combined anatomic factors predicting risk of anterior cruciate ligament injury for males and females. Am J Sports Med 43(4):839–847. https://doi.org/10.1177/0363546514563277
Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J (2006) The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 13(1):26–31. https://doi.org/10.1016/j.knee.2005.06.003
Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP (2009) Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res 467(8):2066–2072. https://doi.org/10.1007/s11999-009-0711-3
Cao J, Zhang J, Yang D, Yang L, Shen Y (2017) Multivariate analysis of factors associated with kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kyphotic alignment. Sci Rep 7:43443. https://doi.org/10.1038/srep43443
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39(2):175–191
Suomalainen JS, Regalado G, Joukainen A, Kaariainen T, Kononen M, Manninen H, Sipola P, Kokki H (2018) Effects of knee flexion and extension on the tibial tuberosity-trochlear groove (TT-TG) distance in adolescents. J Exp Orthop 5(1):31. https://doi.org/10.1186/s40634-018-0149-1
Atarod M, Frank CB, Shrive NG (2014) Kinematic and kinetic interactions during normal and ACL-deficient gait: a longitudinal in vivo study. Ann Biomed Eng 42(3):566–578. https://doi.org/10.1007/s10439-013-0914-3
Chen CH, Li JS, Hosseini A, Gadikota HR, Gill TJ, Li G (2012) Anteroposterior stability of the knee during the stance phase of gait after anterior cruciate ligament deficiency. Gait Posture 35(3):467–471. https://doi.org/10.1016/j.gaitpost.2011.11.009
Bicer EK, Lustig S, Servien E, Selmi TA, Neyret P (2010) Current knowledge in the anatomy of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 18(8):1075–1084. https://doi.org/10.1007/s00167-009-0993-8
Kondo E, Merican AM, Yasuda K, Amis AA (2014) Biomechanical analysis of knee laxity with isolated anteromedial or posterolateral bundle-deficient anterior cruciate ligament. Arthroscopy 30(3):335–343. https://doi.org/10.1016/j.arthro.2013.12.003
Hashemi J, Chandrashekar N, Gill B, Beynnon BD, Slauterbeck JR, Schutt RC Jr, Mansouri H, Dabezies E (2008) The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am 90(12):2724–2734. https://doi.org/10.2106/JBJS.G.01358
Jaecker V, Drouven S, Naendrup J-H, Kanakamedala AC, Pfeiffer T, Shafizadeh S (2018) Increased medial and lateral tibial posterior slopes are independent risk factors for graft failure following ACL reconstruction. Arch Orthop Trauma Surg 138(10):1423–1431. https://doi.org/10.1007/s00402-018-2968-z
Blanke F, Kiapour AM, Haenle M, Fischer J, Majewski M, Vogt S, Camathias C (2016) Risk of noncontact anterior cruciate ligament injuries is not associated with slope and concavity of the tibial plateau in recreational alpine skiers: a magnetic resonance imaging-based case-control study of 121 patients. Am J Sports Med 44(6):1508–1514. https://doi.org/10.1177/0363546516632332
Sonnery-Cottet B, Archbold P, Cucurulo T, Fayard J, Bortolletto J, Thaunat M, Prost T, Chambat P (2011) The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. J Bone Joint Surg British 93(11):1475–1478
Hoteya K, Kato Y, Motojima S, Ingham SJ, Horaguchi T, Saito A, Tokuhashi Y (2011) Association between intercondylar notch narrowing and bilateral anterior cruciate ligament injuries in athletes. Arch Orthop Trauma Surg 131(3):371–376. https://doi.org/10.1007/s00402-010-1254-5
Domzalski M, Grzelak P, Gabos P (2010) Risk factors for anterior cruciate ligament injury in skeletally immature patients: analysis of intercondylar notch width using magnetic resonance imaging. Int Orthop 34(5):703–707. https://doi.org/10.1007/s00264-010-0987-7
Zeng C, Gao SG, Wei J, Yang TB, Cheng L, Luo W, Tu M, Xie Q, Hu Z, Liu PF, Li H, Yang T, Zhou B, Lei GH (2013) The influence of the intercondylar notch dimensions on injury of the anterior cruciate ligament: a meta-analysis. Knee Surg, Sports Traumatol Arthrosc 21(4):804–815. https://doi.org/10.1007/s00167-012-2166-4
Comerford EJ, Tarlton JF, Avery NC, Bailey AJ, Innes JF (2006) Distal femoral intercondylar notch dimensions and their relationship to composition and metabolism of the canine anterior cruciate ligament. Osteoarthritis Cartilage 14(3):273–278. https://doi.org/10.1016/j.joca.2005.09.001
Dienst M, Schneider G, Altmeyer K, Voelkering K, Georg T, Kramann B, Kohn D (2007) Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. Arch Orthop Trauma Surg 127(4):253–260. https://doi.org/10.1007/s00402-006-0177-7
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shen, X., Xiao, J., Yang, Y. et al. Multivariable analysis of anatomic risk factors for anterior cruciate ligament injury in active individuals. Arch Orthop Trauma Surg 139, 1277–1285 (2019). https://doi.org/10.1007/s00402-019-03210-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03210-x