Abstract
Introduction
Mechanical failure due to dislocation, fracture and acetabular wear is a major complication associated with the use of spacers in the management of periprosthetic joint infection (PJI). We have developed a novel custom-made spacer in the setting of two-stage septic revision hip arthroplasty and present the preliminary results of our technique.
Materials and methods
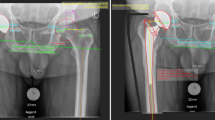
Between May 2015 and November 2017, 30 patients underwent hip revision using the ENDO spacer technique in the setting of a two-stage septic exchange arthroplasty. The technique involves the dual mobility liner and the downsized stainless cemented straight stem in combination with antibiotic-loaded PMMA bone cement. The primary outcome measure was the overall spacer complication rate, particularly spacer dislocation. Furthermore, functional outcome using the Harris Hip Score (HHS) before spacer implantation and prior re-implantation was evaluated.
Results
The mean age of the patients was 69.8 years (range from 45 to 85; SD = 9.9 years). No microorganisms were preoperatively found in 23 (76.7%) cases. Successful re-implantation was performed in all patients after a mean spacer duration time of 53.6 days (range 14–288 days; SD = 48.2). Spacer-related complications occurred in only two patients (6.7%). The HHS significantly improved from 34.0 (range 3–62; SD = 15.1) to 48.1 (range 11–73; SD = 15.7) (p = 0.0008).
Conclusions
The ENDO spacer surgical technique is a feasible option in the treatment of periprosthetic joint infection (PJI), with a low dislocation rate. Furthermore, it allows early mobilization with the possibility of full-weight bearing.





Similar content being viewed by others
References
Fink B, Vogt S, Reinsch M, Buchner H (2011) Sufficient release of antibiotic by a spacer 6 weeks after implantation in two-stage revision of infected hip prostheses. Clin Orthop Relat Res 469(11):3141–3147. https://doi.org/10.1007/s11999-011-1937-4
Masri BA, Duncan CP, Beauchamp CP (1998) Long-term elution of antibiotics from bone-cement: an in vivo study using the prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) system. J Arthroplast 13(3):331–338
Citak M, Argenson JN, Masri B, Kendoff D, Springer B, Alt V, Baldini A, Cui Q, Deirmengian GK, del Sel H, Harrer MF, Israelite C, Jahoda D, Jutte PC, Levicoff E, Meani E, Motta F, Pena OR, Ranawat AS, Safir O, Squire MW, Taunton MJ, Vogely C, Wellman SS (2014) Spacers J Orthop Res 32(Suppl 1):S120–S129. https://doi.org/10.1002/jor.22555
Uchiyama K, Takahira N, Fukushima K, Moriya M, Yamamoto T, Minegishi Y, Sakai R, Itoman M, Takaso M (2013) Two-stage revision total hip arthroplasty for periprosthetic infections using antibiotic-impregnated cement spacers of various types and materials. Sci World J 2013:147248. https://doi.org/10.1155/2013/147248
Barrack RL (2002) Rush pin technique for temporary antibiotic-impregnated cement prosthesis for infected total hip arthroplasty. J Arthroplast 17(5):600–603
Citak M, Masri BA, Springer B, Argenson JN, Kendoff DO (2015) Are preformed articulating spacers superior to surgeon-made articulating spacers in the treatment of PJI in THA? A literature review. Open Orthop J 9:255–261. https://doi.org/10.2174/1874325001509010255
Faschingbauer M, Reichel H, Bieger R, Kappe T (2015) Mechanical complications with one hundred and thirty eight (antibiotic-laden) cement spacers in the treatment of periprosthetic infection after total hip arthroplasty. Int Orthop 39(5):989–994. https://doi.org/10.1007/s00264-014-2636-z
Burastero G, Basso M, Carrega G, Cavagnaro L, Chiarlone F, Salomone C, Papa G, Felli L (2017) Acetabular spacers in 2-stage hip revision: is it worth it? A single-centre retrospective study. Hip Int 27(2):187–192. https://doi.org/10.5301/hipint.5000446
Hoell S, Moeller A, Gosheger G, Hardes J, Dieckmann R, Schulz D (2016) Two-stage revision arthroplasty for periprosthetic joint infections: what is the value of cultures and white cell count in synovial fluid and CRP in serum before second stage reimplantation? Arch Orthop Trauma Surg 136(4):447–452. https://doi.org/10.1007/s00402-015-2404-6
Akgun D, Perka C, Trampuz A, Renz N (2018) Outcome of hip and knee periprosthetic joint infections caused by pathogens resistant to biofilm-active antibiotics: results from a prospective cohort study. Arch Orthop Trauma Surg 138(5):635–642. https://doi.org/10.1007/s00402-018-2886-0
Murgier J, Laffosse JM, Cailliez J, Cavaignac E, Murgier P, Bayle-Iniguez X, Chiron P, Bonnevialle P (2016) Is the prognosis the same for periprosthetic joint infections due to Staphylococcus aureus versus coagulase-negative staphylococci? A retrospective study of 101 patients with 2-year minimum follow-up. Arch Orthop Trauma Surg 136(10):1357–1361. https://doi.org/10.1007/s00402-016-2533-6
Biring GS, Kostamo T, Garbuz DS, Masri BA, Duncan CP (2009) Two-stage revision arthroplasty of the hip for infection using an interim articulated prostalac hip spacer: a 10- to 15-year follow-up study. J Bone Jt Surg Br 91(11):1431–1437. https://doi.org/10.1302/0301-620X.91B11.22026
Bori G, Garcia-Oltra E, Soriano A, Rios J, Gallart X, Garcia S (2014) Dislocation of preformed antibiotic-loaded cement spacers (Spacer-G): etiological factors and clinical prognosis. J Arthroplast 29(5):883–888. https://doi.org/10.1016/j.arth.2013.10.014
Dairaku K, Takagi M, Kawaji H, Sasaki K, Ishii M, Ogino T (2009) Antibiotics-impregnated cement spacers in the first step of two-stage revision for infected totally replaced hip joints: report of ten trial cases. J Orthop Sci 14(6):704–710. https://doi.org/10.1007/s00776-009-1406-z
Tsung JD, Rohrsheim JA, Whitehouse SL, Wilson MJ, Howell JR (2014) Management of periprosthetic joint infection after total hip arthroplasty using a custom made articulating spacer (CUMARS); the exeter experience. J Arthroplast 29(9):1813–1818. https://doi.org/10.1016/j.arth.2014.04.013
Jung J, Schmid NV, Kelm J, Schmitt E, Anagnostakos K (2009) Complications after spacer implantation in the treatment of hip joint infections. Int J Med Sci 6(5):265–273
Anagnostakos K, Duchow L, Koch K (2016) Two-stage protocol and spacer implantation in the treatment of destructive septic arthritis of the hip joint. Arch Orthop Trauma Surg 136(7):899–906. https://doi.org/10.1007/s00402-016-2455-3
Guyen O, Chen QS, Bejui-Hugues J, Berry DJ, An KN (2007) Unconstrained tripolar hip implants: effect on hip stability. Clin Orthop Relat Res 455:202–208. https://doi.org/10.1097/01.blo.0000238796.59596.1f
Sutter EG, McClellan TR, Attarian DE, Bolognesi MP, Lachiewicz PF, Wellman SS (2017) Outcomes of modular dual mobility acetabular components in revision total hip arthroplasty. J Arthroplast. https://doi.org/10.1016/j.arth.2017.03.035
Berend KR, Turnbull NJ, Howell RE, Morris MJ, Adams JB, Lombardi AV Jr (2015) Molded articulating cement spacers for two-stage treatment of infected THA and TKA. Surg Technol Int 26:343–349
Romano CL, Romano D, Logoluso N, Meani E (2010) Long-stem versus short-stem preformed antibiotic-loaded cement spacers for two-stage revision of infected total hip arthroplasty. Hip Int 20(1):26–33
Shida T, Koseki H, Yoda I, Horiuchi H, Sakoda H, Osaki M (2013) Adherence ability of Staphylococcus epidermidis on prosthetic biomaterials: an in vitro study. Int J Nanomed 8:3955–3961. https://doi.org/10.2147/IJN.S51994
Lass R, Giurea A, Kubista B, Hirschl AM, Graninger W, Presterl E, Windhager R, Holinka J (2014) Bacterial adherence to different components of total hip prosthesis in patients with prosthetic joint infection. Int Orthop 38(8):1597–1602. https://doi.org/10.1007/s00264-014-2358-2
Pitto RP, Sedel L (2016) Periprosthetic joint infection in hip arthroplasty: is there an association between infection and bearing surface type? Clin Orthop Relat Res 474(10):2213–2218. https://doi.org/10.1007/s11999-016-4916-y
Gibon E, Cordova LA, Lu L, Lin TH, Yao Z, Hamadouche M, Goodman SB (2016) The biological response to orthopedic implants for joint replacement. II: polyethylene, ceramics, PMMA, and the foreign body reaction. J Biomed Mater Res B Appl Biomater. https://doi.org/10.1002/jbm.b.33676
Vielgut I, Sadoghi P, Wolf M, Holzer L, Leithner A, Schwantzer G, Poolman R, Frankl B, Glehr M (2015) Two-stage revision of prosthetic hip joint infections using antibiotic-loaded cement spacers: when is the best time to perform the second stage? Int Orthop 39(9):1731–1736. https://doi.org/10.1007/s00264-015-2751-5
Fleck EE, Spangehl MJ, Rapuri VR, Beauchamp CP (2011) An articulating antibiotic spacer controls infection and improves pain and function in a degenerative septic hip. Clin Orthop Relat Res 469(11):3055–3064. https://doi.org/10.1007/s11999-011-1903-1
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest regarding this manuscript. Outside the manuscript, one or more of the authors of this paper have disclosed following disclosures: Waldemar Link, Hamburg, Germany; Zimmer; Ceramtec and Heraeus.
Ethical approval
This study was performed after obtaining approval from the institutional review board. The PV number is “PV5443”.
Rights and permissions
About this article
Cite this article
Lausmann, C., Citak, M., Hessling, U. et al. Preliminary results of a novel spacer technique in the management of septic revision hip arthroplasty. Arch Orthop Trauma Surg 138, 1617–1622 (2018). https://doi.org/10.1007/s00402-018-3038-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3038-2