Abstract
Folate-mediated one-carbon metabolism (FOCM) plays an important role in colorectal carcinogenesis. Previous studies have assessed the role of folate-mediated one-carbon metabolism (FOCM)-related gene-diet interaction in the aetiology of colorectal cancer (CRC), however, the results remained inconclusive. Thus, this study aimed to investigate dietary factors and genetic variants related to FOCM, as well as potential nutrient-gene and nutrient-lifestyle interactions, on CRC risk. This observational study included 229 patients diagnosed with CRC and 229 age- and sex-matched subjects as controls from a population-based bowel cancer screening program. Conditional logistic regression was used to calculate odds ratios (ORs) and 95% confidence intervals (95%CI) for CRC risk. A Bonferroni-corrected threshold of α = 0.005 was considered significant, and P values less than 0.05 were considered to be suggestive of an association. After Bonferroni correction, a high dietary intake of betaine was associated with a decreased risk of CRC in the adjusted model (OR, 95% CI: 0.21, 0.10–0.40, P < 0.001). Two SNPs, rs1476413 and rs17824591, exhibited significant gene-diet interactions with total choline ad vitamin B12 intakes, respectively, in adjusted models (total choline, tertile 3 vs. 1, OR, 95% CI: 0.25, 0.11–0.66, Pinteraction = 0.012; vitamin B12, tertile 2 vs. tertile 1, OR, 95% CI: 2.48, 1.04-5.00, Pinteraction = 0.003). These findings suggest that betaine intake and interactions between some dietary factors and variants in MTHFR and MTHFD1 genes have an influence on CRC risk in the population studied. If these results are confirmed, specific nutritional intervention strategies could be designed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Novelty and Impact – What´s new?
Previous studies have assessed the role of folate-mediated one-carbon metabolism (FOCM)-related gene-diet interaction in the aetiology of colorectal cancer (CRC), however, the results remained inconclusive. Here, the authors investigate this type of interaction. The findings highlight the importance of interactions between total choline and vitamin B12 intakes, and variants in MTHFR and MTHFD1 genes on CRC risk. If these results are confirmed, they may provide valuable risk stratification guidance for diet recommendations.
Introduction
Colorectal cancer (CRC) is the third most frequent cancer and the second highest mortality in cancer patients worldwide [1]. In Spain, CRC is currently the most frequently diagnosed tumour, with 41,661 new cases (25,415 in men and 16,246 in women) detected in 20222. This incidence is comparable to that found in high-risk zones of Occidental Europe, North America, Australia, and Japan [3].
Although screening for early detection of CRC is effective in decreasing trends in mortality rates, understanding the factors involved in daily life are CRC-diagnosed also important for a proactive approach to prevent this type of cancer [4]. The primary prevention for CRC is mostly associated with diet, lifestyle factors, and metabolic diseases. Regarding dietary factors, one-carbon metabolism (1CM)-related nutrients (such as folate, other B vitamins, methionine (Met), choline, and betaine) have been considered anticarcinogenic and chemotherapeutic agents in the 1 C metabolic network [5], whereas alcohol antagonizes 1CM, and its high consumption has been related to higher CRC risk [6]. In addition, the observed inverse association between folate status and CRC risk was further modified by genetic polymorphisms of the enzymes involved in folate metabolism, most notably methylene tetrahydrofolate reductase (MTHFR) [5].
However, not only the influence of polymorphisms but also the influences of 1CM-related nutrients on genetic polymorphisms in relation to interaction CRC risk remain largely unexplored. Most studies on this type of gene-diet interaction have focused on folate, B vitamin, and methionine intake [7]. To date, there are no studies in which the intake of choline and/or betaine has been evaluated. To better elucidate the role of genetic factors and environmental conditions, especially diet, on CRC risk, this study had a triple aim: (i) to investigate dietary factors (dietary methyl donors and dietary components that potentially modulate the bioavailability of methyl groups) and genetic variants in methyl metabolizing enzymes; (ii) to determine the potential nutrient-gene interactions; and (iii) to analyse the potential nutrient-lifestyle interactions, that is, interactions between the consumption of the dietary factors mentioned on the first objective and other lifestyle factors.
These aims refer to the CRC risk, in a sample of cases and controls, matched on age and sex, from the population-based bowel cancer screening program (BCSP) of the Osakidetza/Basque Health Service. In particular, the dietary factors investigated were: intakes of folate, vitamins B2, B6, and B12, Met, choline, betaine, and ethanol; the genetic variants: DNA methyltransferases (DNMT3B and DNMT1), MTHFR, methylene tetrahydrofolate dehydrogenase 1 (MTHFD1), and Met synthase reductase; and the other lifestyle factors: physical exercise (PE), smoking, and alcohol consumption.
Methods
Study participants
Overall, this epidemiologic study is an observational analytic case-control study designed to address possible gene-diet interactions in relation to CRC. Participants in this study were recruited from among patients attending any of the three hospitals of the Osakidetza/Basque Health Service (Basurto, Galdakao, and Donostia) members of the Basque Country’s BCSP. To be eligible for this BCSP, the patients had to be aged between 50 and 69, asymptomatic for colorectal symptoms, and registered with the Osakidetza/Basque Health Service.
These inclusion criteria were applied to both case and control groups; that is, controls fulfilled the same eligibility criteria defined for the cases, except for the disease (outcome). The age- and sex-matched controls were patients with positive results (abnormal) for an immunochemical faecal occult blood test and negative colonoscopy results (normal). Recruitment and data collection through questionnaires were conducted between 2014 and 2016. The start date of the study was 2014 because the BCSP in the Basque Country reached the whole target population (approximately 586,700 people) at the beginning of this year.
The characteristics of the sampling and the cases (pathological staging, location of cancer, tumour grade, and treatments) have been described before [8]. Briefly, 72% were diagnosed with early-stage (I/II) CRC and 76% had a distal location of cancer. The total sample consisted of 308 cases who were diagnosed with CRC and 308 age- and sex-matched controls. However, in the present study, data from 229 CRC patients and 229 controls were analysed, since this is the sample from which biological samples and associated data were obtained. All participants had data on the main dietary factors (folate, vitamin B2, B6, B12, Met, choline, and betaine) and genetic variants that were included in the present study.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving patients were approved by the Clinical Research Ethics Committee of the Basque Country (protocol code PI2011006, data of approval 03/23/2012; and PI2014042, data of approval 05/28/2014). Written informed consent was obtained from all the study participants.
Dietary assessment
Diets were assessed using a short food frequency questionnaire (FFQ) that was a modified version of the Rodríguez et al. questionnaire [9]. This adaptation was validated with multiple 24-h recalls in the Basque general population [10] and CRC-diagnosed patients in a pilot of the present study [11]. It consisted of 67 items and requires the subjects to recall the number of times each food item was consumed either per week or per month. Moreover, the respondents could also record the consumption of other foods that were not included on the food list, as well as the use of dietetic products and nutritional supplements (generic and brand-name, dose, and frequency).
Once the completed FFQ was received, it was reviewed by a dietitian. Consumption frequencies were standardised to “per day” and multiplied by standard serving sizes (grams) [12]. For items that included several foods, each food’s contribution was estimated with weighting coefficients that were obtained from the usual consumption data [13]. All food items that were consumed were entered into DIAL 2.12 (2011 ALCE INGENIERIA), a type of dietary assessment software, to estimate energy intake (kcal/day), dietary fibre, and 1CM-related vitamins (B2, B6, folate, and B12). The intakes of other 1CM-related compounds, in particular, Met, total choline, and betaine were estimated using the United States Department of Agriculture (USDA) Food Data central database [14] and from the publication of Zeisel et al. [15].
Assessment of covariates
Potential confounders of CRC risk were selected based on published evidence from European Prospective Investigation into Cancer and Nutrition (EPIC), the International Agency for Research on Cancer (IARC), and the World Cancer Research Fund (WCRF), which included: overweight or obesity based on self-reported body mass index (BMI), age, sex, PE (expressed as daily minutes of cycling/sports), smoking (never vs. past/currently, and intensity of smoking measured by the number of cigarettes smoked per day), and alcohol consumption (reported as grams of ethanol per day). In addition, the use of drugs related to decreasing CRC risk (antiplatelet, including non-steroidal anti-inflammatory drugs, and anticoagulants) [16] was recorded. These questions were taken from the Spanish Health Questionnaire [17]. BMI, estimated from self-reported height and weight, was classified according to the WHO criteria for those under 65 years of age [18] and according to the criteria proposed by Silva Rodrigues et al. for those 65 and older [19]. The characteristics of the sample is shown in the Supplementary Material (Table S1).
On the other hand, the FFQ used to assess dietary intake included specific questions about the frequency of intake of the following five major types of alcoholic beverages: beer, wine, cider, aperitif with alcohol, and liquor. These consumption frequencies were standardised to “per day” and multiplied by standard serving sizes (ml) [20]. The alcohol consumption data were expressed as grams of ethanol/day that were estimated with the software DIAL 2.12 (2011 ALCE INGENIERIA) and standard drink units [21]. We used the standard drink unit defined for Spain (one standard drink unit is the equivalent of 10 g of ethanol). With this information, the participants were categorised into those who did and did not meet the recommendations [20]. Those participants who did not meet the recommendations were categorised as “high-risk consumption.”
The differences in general characteristics (age, BMI, PE, smoking, and alcohol consumption, among others) between cases and controls were previously described [22]. Briefly, significant differences between cases and controls were found for smoking and weight status, with a higher percentage of cases with past or current smoking status and with overweight/obesity compared to controls (P < 0.01). However, no significant differences were found in alcohol consumption between cases and controls (P > 0.05).
Additionally, in both cases and controls, socioeconomic level, and health status (specifically health resource consumption) data were assessed with two indices that were obtained from the clinical databases developed by the Health Department of the Basque Government, namely the socioeconomic deprivation index (DI) and predictive risk modelling (PRM), respectively. The first one was estimated using the MEDEA project criteria, as has been described elsewhere, [23] and was divided into quintiles, with the first being the least disadvantaged and the fifth being the most disadvantaged. The PRM is an index that is based on Adjusted Clinical Groups [24] and Clinical Risk Groups [25]. This index combines information about diagnoses, prescriptions, previous costs, and the use of specific procedures. It can predict the use of health resources, and it was stratified into four levels: the first included participants with a risk of high health resource consumption, and the fourth included those with low health resource consumption. The differences in these two indices (DI and PRM) between cases and controls were previously described [22].
Biological samples and genotyping
In this study, healthy tissues or saliva samples of cases and controls were collected and genotyped. Samples were provided by the Basque Biobank for Research-OEHUN (www.biobancovasco.org) and were processed following standard operating procedures with appropriate approval of the Ethical and Scientific Committees. DNA was extracted using AllPrep DNA / RNA kit (Qiagen) for paraffin-embedded tissue samples and AutoGenFlex Tissue DNA Extraction kit (Autogen) for mouthwash saliva samples and then was quantified with NanoDrop™ Spectrophotometer (ThermoFisher). Double-stranded DNA was quantified by fluorometry using the Quant-iT™ PicoGreen1 dsDNA Assay Kit (Invitrogen, CA) on a DTX 880 Multimode Detector (Beckman Coulter) to normalize DNA concentration.
After an updated summary of the published genetic variants in methyl metabolizing enzymes related to CRC risk, a total of ten single nucleotide polymorphisms (SNPs) were identified, in particular: DNMT3B (rs2424913, rs406193), [26] DNMT1 (rs2228612), [27] MTHFR (rs1476413, rs1801131, rs1801133), [28, 29] MTHFD1 (rs8003379, rs17824591) and Met synthase reductase (rs1801394, rs10380) [29]. These SNPs were organised in the context of the gene(s) at or near the locus and chromosome locus. The allelic discrimination was assessed using the MassARRAY1 System (Agena Bioscience) on CeGen-PRB2-ISCII (Nodo USC) following the procedure provided by the manufacturer. Quality control samples were included in the genotyping assays.
Statistical analysis
The sample size was estimated to be 286 in each group (cases and controls) to detect an odds ratio (OR) of 2.0 with 80% power at a two-sided level of significance of 5%, under an exposure prevalence of 10%, using the Epidat 3.0 program [30].
Data were analysed using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp., Armonk, NY, USA) and STATA 16.0 (StataCorp LP, Texas, USA). Categorical variables are shown as a percentage, and continuous variables are as the means and standard deviation. Normality was checked using the Kolmogorov–Smirnov–Lilliefors test and since all continuous variables followed a non-normal distribution, the Wilcoxon rank-sum test was used for two related means comparison. The Chi-square test was used to evaluate differences between categorical variables. When expected frequencies were lesser than five, Fisher´s exact test was used. Tests for associations and deviation from Hardy-Weinberg equilibrium were performed separately in cases and controls.
Conditional logistic regression was used to calculate ORs and 95% confidence intervals (95%CI) for CRC risk according to (i) tertiles (T) of dietary compound intake, (ii) dominant and recessive models of SNPs, (iii) nutrient-gene interactions, and (iii) nutrient-lifestyle interactions. The logistic regression models were applied to the total sample and the subgroup of cases with distal location (n = 178) and their respective controls (Tables S2, S7, and S8). When the sample size was small (≤ 10 per group), the conditional exact logistic regression model was applied. The logistic regression model could not be applied to the subgroup of cases with proximal location due to the (too small) sample size. The intake of dietary compounds was categorised into Ts based on the distribution in the control group, taking into account sex differences when they were significant. Specifically, different cutoff points were applied to estimate Ts in men and women when significant sex differences were identified, that is, in the case of folate and Met intake. The lowest T was used as the reference group. The most frequent genotype (homozygous) was considered the reference group to calculate ORs in a dominant model, and the most frequent genotype (homozygous) and the heterozygous genotype containing the risk allele were considered the reference group in the recessive model. The nutrient-gene interaction analyses were carried out using a dominant model for genotypes.
The analyses of logistic regression were done for the unadjusted (model I) and adjusted models (models II and III). Models II and III were adjusted for known risk factors for CRC: [31, 32] age, sex, BMI, PE level, smoking status, the intensity of smoking (in current and past smokers), socio-economic level (DI) and health status (PRM), energy intake, dietary fibre, ethanol intake, and antiplatelet and anticoagulants use. The reference categories were those that, according to the literature, have a lower CRC risk. For the BMI variable, normal weight was considered as the reference category, and underweight was included as a separate category. We included participants with missing data for the covariates as a separate category.
Quantitative covariates such as intensity of smoking (cigarettes/day) were dichotomised by mean or median, according to the normality test. We used the cut-off of Romaguera et al. [33] to create two PE levels expressed in min/day of cycling/sports: sedentary-light (< 15 min/day) and moderate-vigorous (≥ 15 min/day). Age was dichotomised using the same age ranges that were used in the sample selection process (50–59 years old vs. 60–69 years old). Qualitative ones, such as DI and PRM were dichotomised considering the distribution of frequencies to obtain similar sample sizes for each category (DI, quintile 1–3 vs. quintile 4–5; PRM, level 3–4 vs. level 1–2). Energy, dietary fibre, and ethanol intake were included as quantitative variables in the adjusted models.
In model II, dietary compound intake or SNPs were included separately, whereas model III was only used in the analysis of dietary compound intake and, in this case, all the compounds were included at the same time. In addition, to study the possible association between the intake of betaine and total choline, and the CRC risk, model II (adjusted model) of the regression analysis was also applied, including folate as covariate (these data are shown in text form in the Results section). The significance level was corrected using a Bonferroni correction by dividing the standard P value (two-tailed) (α = 0.05) by the total number of SNPs analysed (n = 10), assuming alpha was equal to 0.005 (α = 0.05/10).
Results
Colorectal cancer risk according to nutrient intake
The intakes of folate, vitamins B2 and B6, Met, choline, and betaine were significantly higher in controls than those in cases (P < 0.001), whereas the consumption of vitamin B12 and alcohol was higher in cases than controls (P < 0.001) (Table 1). The ORs for CRC risk by the intake of nutrients are presented in Table 2. The adjusted ORs for CRC risk decreased with higher intakes of choline and betaine (P < 0.005). Although in the case of choline, the association was only significant in the unadjusted model. These results were confirmed in the subgroup of cases with distal tumour location (Table S2). In the total sample, after further adjustment for folate, moderate intake of betaine remained associated with a reduced risk of CRC (Model II including folate as a covariate, ORT2 vs. T1 = 0.36, 95% CI: 0.20–0.65, P = 0.001; ORT3 vs. T1 = 0.20, 95% CI: 0.09–0.40, P < 0.01).
Colorectal cancer risk according to polymorphism genotypes
The distribution of genotypes at SNPs selected in the CRC group and in the control group that deviated from the Hardy-Weinberg equilibrium is shown in the Supplementary Material (Table S3). The SNP that was not following the Hardy-Weinberg equilibrium in controls was rs1801394 (P < 0.05), however, this SNP showed no significance when the conservative Bonferroni method is used. None of the genotype frequencies for the SNPs analysed reached statistically significant differences between cases and controls, after the Bonferroni correction.
Supplementary Table S4 presents the associations between genotype variants and CRC risk. No significant association was found between the genotype for any SNP analysed and CRC risk, except a decreased risk of CRC among those with rs2424913-TT variant (ORTT vs. CC = 0.56, 95% CI: 0.33–0.96, P < 0.05), even though this association was not significant after the Bonferroni correction.
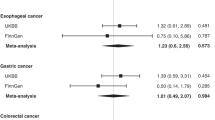
Colorectal cancer risk according to nutrient-gene interactions
Associations between SNP genotypes and CRC risk, stratified by dietary factors in unadjusted and adjusted models are shown in Supplementary Tables S5 and S6, respectively. A summary of all observed associations between folate metabolism-related nutrients and SNPs on CRC risk is provided in Table 3. In the unadjusted model, the rs1476413-CC genotype was associated with a decreased risk of CRC among individuals with high total choline intake (OR T3 vs. T1 = 0.29, 95% CI: 0.15–0.55) (Pinteraction = 0.002). This result was also confirmed in the adjusted model, although in this case, P-value did not remain significant after applying the Bonferroni correction (Pinteraction = 0.012). Moreover, in the adjusted model, the rs17824591-GG genotype was associated with an increased risk of CRC among individuals with moderate vitamin B12 intake (OR T2 vs. T1 = 2.48, 95% CI: 1.04-5.00) (Pinteraction = 0.003). Although, in the unadjusted model, these results were not confirmed in the subgroup of cases with distal tumour location (Table S7); in the adjusted model, the rs1476413-CC genotype was associated with a decreased risk of CRC among subjects with high betaine intake (OR T3 vs. T1 = 0.22, 95% CI: 0.09–0.49) (Pinteraction = 0.004) (Table S8).
Additionally, even if the remaining combination of SNPs and nutrient intakes did not show any significant interaction for CRC risk, the following variants were associated with a decreased risk of CRC among individuals with moderate-high betaine and/or total choline intake, in both the unadjusted and adjusted models (Tables S5 and S6): DNMT3B (rs2424913, rs406193), DNMT1 (rs2228612), MTHFR (rs1801131, rs1801133), MTHFD1 (rs8003379, rs17824591), and Met synthase reductase (rs1801394, rs10380). These results were confirmed in the subgroup of cases with distal tumour location (Table S7 and S8).
Colorectal cancer risk according to nutrient-lifestyle interactions
On the other hand, the combined effects of nutrient intake and lifestyle factors (PE, smoking, and alcohol consumption) on CRC risk were also examined. Individuals who reported both a low and a moderate-high level of PE (OR T3 vs. T1 = 0.27, 95% CI: 0.13–0.66; OR T3 vs. T1 = 0.12, 95% CI: 0.07–0.44, respectively) and a low or no alcohol consumption (OR T3 vs. T1 = 0.34, 95% CI: 0.23–0.61) and had high betaine intake showed a low CRC risk, even if no significant interactions were found (Table 4).
Discussion
The present study aimed to determine the association between dietary factors and genetic variants related to the FOCM and CRC risk, as well as possible nutrient-gene interactions. Moreover, the combined effects of nutrient intake and lifestyle factors (PE, smoking, and alcohol consumption) on CRC risk were also examined. Our results suggest that betaine intake and interactions between some dietary factors and variants in MTHFR and MTHFD1 genes have an influence on CRC risk in the population studied. The results were confirmed in the subgroup with distal tumour location. On the other hand, no significant interactions were observed between nutrient intake and lifestyle factors on CRC risk.
As we mentioned in the introduction section, to date, few epidemiologic studies have examined the association between betaine and cancer risk, and those who have studied this possible relationship have obtained inconsistent results. Several researchers found an inverse association between betaine intake and breast cancer risk [34]. However, other studies found no evidence that higher intakes of this nutrient reduced the risk of breast cancer [35]. Some studies have reported that a higher intake of betaine was associated with a reduced risk of lung cancer [36], whereas no association was found for epithelial ovarian cancer [37]. It has been suggested that the underlying mechanisms by which a high intake of betaine would reduce the risk of some cancers would be similar to those of folate. Betaine can donate the methyl group to homocysteine as does folate, although the donation of the methyl group by betaine is limited to the liver and the kidney [34]. A high intake of betaine could help prevent the adverse effect resulting from hypomethylation of DNA or restore DNA repair mechanism, and therefore, would lead to reduced cancer risk [36].
Inconsistent results were also observed on the relationship between betaine intake and CRC risk. The Health Professionals Follow-up Study conducted in the United States [38] and an investigation carried out in a Chinese population [39] have examined this possible association and in both studies, no association was found. This result has been attributed, in part, to the fact that the levels of this nutrient would not be critical in folate-nourished populations, because folate and choline metabolic pathways are highly interrelated, and betaine is derived from choline and increase in response to a higher choline intake [40].
Our study, like another case-control study, where plasma betaine was analysed, [41] confirmed the inverse association between betaine intake and CRC risk, even among subjects with an average total folate intake below population recommendations and below the intakes recorded in other studies, such as the Health Professionals Follow-up Study mentioned above, [38] with a total folate intake from diet and supplements of 479–858 µg/day in the total sample. In the present study, the average folate intake was 270.9 µg/day among controls and therefore the intake level of folate was not very high.
Nevertheless, the few published on the association between betaine intake and CRC risk are confusing. Neither the Health Professionals Follow-up Study [38] nor the one carried out by Lu et al. [39] found significant associations for betaine intakes. These discrepancies could be due to differences in the characteristics of participants, the intake and status of other nutrients involved in FOCM, and the design type. In summary, in the Health Professionals Follow-up Study, [38] the participants were US male health professionals aged 40 to 75 years, and in Lu et al.´s study, [39], Chinese males and females aged 30 to 75 years. The folate intake in the total sample of Lee et al.´ study [38] was of 479–858 µg/day, whereas, in the control sample of Lu et al.´s study [39] was 240.3 µg/d. Lee et al.´ study [38] is a prospective cohort study, whereas, Lu et al.´s study [39] is a case-control study.
Regarding the possible associations between genetic variants related to the FOCM and CRC risk, in the current study, a genotype in DNMT3B (rs2424913) was related to CRC risk, even though this relationship was not significant after the Bonferroni correction. Other authors did not find a close correlation between this genetic variant and the development of CRC among the Chinese population [42]. As regards potential nutrient-gene interactions on CRC risk, rs1476413, and rs17824591 exhibited significant nutrient-gene interactions with total choline and vitamin B12 intakes, respectively. These findings suggest that these variants in MTHFR and MTHFD1 genes interact with dietary factors to modify the risk for CRC. It should be noted that the mechanism by which choline intake/status affects DNA integrity is not entirely clear but may be through effects on mitochondrial membrane integrity and oxidative stress [43]. Regarding vitamin B12, the underlying mechanism by which a high intake of this vitamin would reduce CRC risk could be related to tumour methylation, as other authors have pointed out in colon cancer [44].
In another case-control study, however, no interactions were found between the MTHFR rs1476413 SNP and dietary factors (including folate and Met) on CRC risk, although other MTHFR and MTHFD1 SNPs exhibited gene-diet interactions with Met intake [28]. The lack of data on the possible interaction between the aforementioned SNPs, and their interaction with betaine, makes it difficult to compare our results to other studies.
Most studies assessing MTHFR and CRC risk have focused on the rs1801133 SNP. The variant allele in this SNP causes an increase in thermolability of the MTHFR enzyme [45] which is associated with decreased plasma folate and increased plasma homocysteine [46]. The potential influence of MTHFR activity on DNA methylation and the availability of uridylates and thymidylates for DNA synthesis and repair makes MTHFR an attractive candidate for a cancer-predisposing gene. Even if other studies found an association between this SNP and the CRC risk and interaction with Met, [42] in the present study no significant association was found between these factors. Furthermore, few studies have assessed polymorphisms in MTHFD1 in relation to risk for CRC [7, 42]. Nevertheless, those SNPs (rs2295638, rs2236225) in which they found interaction with nutrients, specifically with Met [7, 42, 47] were not any of those analysed in the present study.
In any case, even if in the present study no more nutrient-gene interactions were detected, individuals with moderate-high betaine and/or total choline intakes showed a decreased risk, for all genotypes analysed, both in the total sample and in the subgroup with distal tumour location. Finally, concerning interactions between nutrient intakes and lifestyle factors, although no interactions were found, individuals who reported low or no alcohol consumption, and had moderate-high levels of PE and high betaine intake showed the lowest risk of CRC. Even though no data have been found in the literature on these interactions, our findings agree with previous studies about the interaction effects of folate status and lifestyle factors on CRC risk [48].
The main strength of this study compared to other previous published [49] is that colonoscopy was used as a diagnosis criterion to identify both cases and controls to avoid false positives and negatives. To our knowledge, to date, only one other study of the association between diet and CRC risk has been published, in which it was confirmed that controls were free of the disease through colonoscopy [50]. Another strength is the fact that information is provided based on a standardised protocol including not only dietary factors but also other possible determinants of CRC such as health determinants and weight status among others. However, some limitations should be mentioned. First, recall bias is also of concern in case-control studies. Second, the small sample size makes it difficult to detect possible associations and nutrient-gene and nutrient-lifestyle interactions and disease risk, since some genotypes and categories according to lifestyle factors showed low frequencies in our population.
Another disadvantage of the small sample size is that they can produce false-positive results; to avoid it, the Bonferroni correction was used. Third, self-reported data could be subject to measurement errors and the problem of food omissions due to memory failure and under-reporting of unhealthy habits among disease subjects. However, previous validation studies indicate that the self-reported dietary information is reported with sufficient accuracy for use in epidemiology analysis [51]. Fourth, although the FFQ used to collect information on dietary intake in the present study has been validated among people who lived in the same region, this validation did not include specific nutrients such as betaine or total choline, but it included the main food sources of these methyl-donors. So, the possible measurement errors are most likely non-differential and thus do not explain the inverse associations observed in our study.
Fifth, even though data on lifestyles (including diet) were recorded retrospectively—that is, the questions referred to behaviours before participating in the BCSP—it should be also noted that dietary changes are usually modest after participating in the BCSP due to a lack of information and personalised advice [52]. In addition, adults generally maintain relatively stable eating habits for a long time [53]. Therefore, the results of this study are unlikely to be greatly affected by potential changes in eating. Sixth, although we have adjusted for several confounding factors, some residual confounding may result from the misclassification of those variables and confounding by unmeasured variables. Finally, to avoid selection bias of controls, we obtained controls from the same BCSP and in the same period as cases. It should also worth noting that we have compared our results with those of the Health Professionals Follow-up Study, [38] that only includes male participants.
In conclusion, the present study suggests that high betaine intake is associated with decreased risk of CRC among the population studied. Moreover, our results support the existing hypothesis of genetic-nutrient interactions in colorectal carcinogenesis. Total choline and vitamin B12 intake, and the SNPs rs1476413 and rs17824591 may be related, respectively, to CRC risk in this population. High total choline intake together with the MTHFR rs1476413-CC genotype reduces CRC risk, whereas moderate vitamin B12 intake together with the MTHFD1 rs17824591-GG genotype increases CRC risk.
Further studies are necessary to confirm these associations and understand in depth their role in colorectal carcinogenesis, including participants under 50 years old. Understanding the interaction between nutrition and genetic variation can be useful to distinguish between individuals who will and who will not benefit from diet intervention strategies.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- 1CM:
-
One-carbon metabolism
- BCSP:
-
Population-based bowel cancer screening program
- CI:
-
Confidence interval
- CRC:
-
Colorectal cancer
- DI:
-
Deprivation index
- DNMT:
-
DNA methyltransferases
- FFQ:
-
Food frequency questionnaire
- FOCM:
-
Folate-mediated one-carbon metabolism
- Met:
-
Methionine
- MTHFD1:
-
Methylene tetrahydrofolate dehydrogenase 1
- MTHFR:
-
Methylene tetrahydrofolate reductase
- OR:
-
Odds ratio
- PE:
-
Physical exercise
- PRM:
-
Predictive risk modelling
- SD:
-
Standard deviation
- SNP:
-
Single nucleotide polymorphism
- T:
-
Tertile
References
Morgan E, Arnold M, Gini A, Lorenzoni V, Cabasag CJ, Laversanne M, Vignat J, Ferlay J, Murphy N, Bray F (2023) Global burden of colorectal cancer in 2020 and 2040: incidence and mortality estimates from GLOBOCAN. Gut 72(2):338–344. https://doi.org/10.1136/gutjnl-2022-327736
Cancer Observatory of the Spanish Association against Cancer (2022) Accessed December 28, 2023. https://observatorio.contraelcancer.es/
World Health Organization. Cancer Today. Global Cancer Observatory [GCO] (2020) Accessed December 28, 2023. http://gco.iarc.fr/today
Keum N, Giovannucci E (2019) Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol 16(12):713–732. https://doi.org/10.1038/s41575-019-0189-8
Choi SW, Mason JB (2002) Folate status: effects on pathways of colorectal carcinogenesis. J Nutr 132(8 Suppl). https://doi.org/10.1093/jn/132.8.2413s. :2413S-2418S
Fedirko V, Tramacere I, Bagnardi V, Rota M, Scotti L, Islami F, Negri E, Straif K, Romieu I, La Vecchia C, Boffetta P, Jenab M (2011) Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol 22(9):1958–1972. https://doi.org/10.1093/annonc/mdq653
Liu AY, Scherer D, Poole E, Potter JD, Curtin K, Makar K, Slattery ML, Caan BJ, Ulrich CM (2013) Gene-diet-interactions in folate-mediated one-carbon metabolism modify colon cancer risk. Mol Nutr Food Res 57(4):721–734. https://doi.org/10.1002/mnfr.201200180
Alegria-Lertxundi I, Aguirre C, Bujanda L, Fernández FJ, Polo F, Ordovás JM, Etxezarraga MC, Zabalza I, Larzabal M, Portillo I, M de Pancorbo M, Palencia-Madrid L, Garcia-Etxebarria K, Rocandio AM, Arroyo-Izaga M (2020) Gene-diet interactions in colorectal cancer: survey design, instruments, participants and descriptive data of a case-control study in the Basque Country. Nutrients 12(8):2362. https://doi.org/10.3390/nu12082362
Rodríguez IT, Ballart JF, Pastor GC, Jordà EB, Val VA (2008) Validación De Un Cuestionario De frecuencia de consumo alimentario corto: reproducibilidad y validez [Validation of a short questionnaire on frequency of dietary intake: reproducibility and validity]. Nutr Hosp 23(3):242–252 PMID: 18560701
Telleria-Aramburu N, Alegria-Lertxundi I, Arroyo-Izaga M (2021) Adaptation, validation and reproducibility of a short FFQ to assess food group intake in the population resident in the basque country (Spain). Public Health Nutr 24(3):436–448. https://doi.org/10.1017/s1368980020001822
Alegria-Lertxundi I, Alvarez M, Rocandio AM, de Pancorbo MM, Arroyo-Izaga M (2016) Nutritional adequacy and diet quality in colorectal cancer patients postsurgery: a pilot study. Nutr Cancer 68(4):577–588. https://doi.org/10.1080/01635581.2016.1158299
Carbajal A, Sánchez-Muniz FJ, Secretariat of Publications and Audiovisual Media (2003) Guía de prácticas en Nutrición y Dietética [Guide to Practices in Nutrition and Dietetics]. University of León, ; :1–3. Accessed December 10, 2020. https://www.ucm.es/data/cont/docs/458-2019-01-04-Guia-Practicas-2019-web.pdf
Department of Agriculture, Fisheries and Food, Basque Government. Estudio cuantitativo del consumo de alimentos en la CAPV [Quantitative study of food consumption in the autonomous community of the Basque Country]. Basque Government: Central Publication Service (2008) Accessed December 9, 2020. https://www.euskadi.eus/contenidos/informacion/coleccion_elika/es_dapa/adjuntos/Guia_Elika_8.pdf
U.S. Department of Agriculture, Agricultural Research Service. USDA’s FoodData Central (2017) Accessed August 9, 2018. https://fdc.nal.usda.gov/
Zeisel SH, Mar MH, Howe JC, Holden JM (2003) Concentrations of choline-containing compounds and betaine in common foods. J Nutr 133(5):1302–1307. https://doi.org/10.1093/jn/133.5.1302
Iles-Shih L, Collins JF, Holub JL, Lieberman DA (2010) Prevalence of significant neoplasia in FOBT-positive patients on warfarin compared with those not on warfarin. Am J Gastroenterol 105(9):2030–2035. https://doi.org/10.1038/ajg.2010.264
Ministry of Health, Social Services and Equality, Government of Spain / National Statistics Institute. Encuesta Nacional de Salud. España 2011/12 [National Health Survey, Spain 2011/12]. Accessed December 20 (2019) http://www.msssi.gob.es/estadEstudios/estadisticas/sisInfSanSNS/nivelSalud.htm
World Health Organization. Obesity: preventing and managing the global epidemic: report of a WHO consultation, 2000. Accessed December 5 (2019) https://apps.who.int/iris/handle/10665/42330
Silva Rodrigues RA, Martinez Espinosa M, Duarte Melo C, Rodrigues Perracini M, Rezende Fett WC, Fett CA (2014) New values anthropometry for classification of nutritional status in the elderly. J Nutr Health Aging 18(7):655–661. https://doi.org/10.1007/s12603-014-0451-2
Serra-Majem L, Aranceta J, SENC Working Group on Nutritional Objectives for the Spanish Population (2001) Spanish Society of Community Nutrition. Nutritional objectives for the Spanish population. Consensus from the Spanish Society of Community Nutrition. Public Health Nutr 4(6A):1409–1413. https://doi.org/10.1079/phn2001229
Ministry of Health and Consumption, Government of Spain. Informes de la Comisión Clínica 2017: Alcohol [Clinical Commission Reports: Alcohol]. Accessed December 10 (2019) http://www.pnsd.msc.es/Categoria2/publica/pdf/InformeAlcohol.pdf
Alegria-Lertxundi I, Aguirre C, Bujanda L, Fernández FJ, Polo F, Ordovás JM, Etxezarraga MC, Zabalza I, Larzabal M, Portillo I, de Pancorbo MM, Palencia-Madrid L, Rocandio AM, Arroyo-Izaga M (2019) Single nucleotide polymorphisms associated with susceptibility for development of colorectal cancer: case-control study in a basque population. PLoS ONE 14(12):e0225779. https://doi.org/10.1371/journal.pone.0225779
Orueta JF, Nuño-Solinis R, Mateos M, Vergara I, Grandes G, Esnaola S (2013) Predictive risk modelling in the Spanish population: a cross-sectional study. BMC Health Serv Res 13:269. https://doi.org/10.1186/1472-6963-13-269
School of Public Health, Johns Hopkins University. The Johns Hopkins University ACG Case-Mix System. Accessed August 10 (2012) http://www.acg.jhsph.org/index.php?option=com_content&view=article&id=46&Itemid=61
Verisk Analytics, Inc. DxCG® Introduces Disease Management Calculator. Accessed August 10 (2012) https://www.verisk.com/archived/dxcg-introduces-disease-management-calculator/
de Vogel S, Wouters KA, Gottschalk RW, van Schooten FJ, de Goeij AF, de Bruïne AP, Goldbohm RA, van den Brandt PA, van Engeland M, Weijenberg MP (2011) Dietary methyl donors, methyl metabolizing enzymes, and epigenetic regulators: diet-gene interactions and promoter CpG island hypermethylation in colorectal cancer. Cancer Causes Control 22(1):1–12. https://doi.org/10.1007/s10552-010-9659-6
Li H, Liu JW, Sun LP, Yuan Y (2017) A Meta-analysis of the association between DNMT1 polymorphisms and cancer risk. Biomed Res Int 2017:3971259. https://doi.org/10.1155/2017/3971259
Ashmore JH, Lesko SM, Muscat JE, Gallagher CJ, Berg AS, Miller PE, Hartman TJ, Lazarus P (2013) Association of dietary and supplemental folate intake and polymorphisms in three FOCM pathway genes with colorectal cancer in a population-based case-control study. Genes Chromosomes Cancer 52(10):945–953. https://doi.org/10.1002/gcc.22089
Pardini B, Kumar R, Naccarati A, Prasad RB, Forsti A, Polakova V, Vodickova L, Novotny J, Hemminki K, Vodicka P (2011) MTHFR and MTRR genotype and haplotype analysis and colorectal cancer susceptibility in a case-control study from the Czech Republic. Mutat Res 721(1):74–80. https://doi.org/10.1016/j.mrgentox.2010.12.008
Service of Epidemiology (2004) Dirección Xeral de Saúde Pública, Consellería de Sanidade, Xunta de Galicia, Spain; Unit of Health Analysis and Information Systems, Pan-American Health Organization (PAHO), Washington, DC. Epidat 3.0 program. Santiago de Compostela, A Coruña, Spain
Torres Stone RA, Waring ME, Cutrona SL, Kiefe CI, Allison J, Doubeni CA (2017) The association of dietary quality with colorectal cancer among normal weight, overweight and obese men and women: a prospective longitudinal study in the USA. BMJ Open 7(6):e015619. https://doi.org/10.1136/bmjopen-2016-015619
Doubeni CA, Laiyemo AO, Major JM, Schootman M, Lian M, Park Y, Graubard BI, Hollenbeck AR, Sinha R (2012) Socioeconomic status and the risk of colorectal cancer: an analysis of more than a half million adults in the National Institutes of Health-AARP Diet and Health Study. Cancer 118(14):3636–3644. https://doi.org/10.1002/cncr.26677
Romaguera D, Vergnaud AC, Peeters PH, van Gils CH, Chan DS, Ferrari P, Romieu I, Jenab M, Slimani N, Clavel-Chapelon F, Fagherazzi G, Perquier F, Kaaks R, Teucher B, Boeing H, von Rüsten A, Tjønneland A, Olsen A, Dahm CC, Overvad K, Quirós JR, Gonzalez CA, Sánchez MJ, Navarro C, Barricarte A, Dorronsoro M, Khaw KT, Wareham NJ, Crowe FL, Key TJ, Trichopoulou A, Lagiou P, Bamia C, Masala G, Vineis P, Tumino R, Sieri S, Panico S, May AM, Bueno-de-Mesquita HB, Büchner FL, Wirfält E, Manjer J, Johansson I, Hallmans G, Skeie G, Benjaminsen Borch K, Parr CL, Riboli E, Norat T (2012) Is concordance with World Cancer Research Fund/American Institute for Cancer Research guidelines for cancer prevention related to subsequent risk of cancer? Results from the EPIC study. Am J Clin Nutr 96(1):150–163. https://doi.org/10.3945/ajcn.111.031674
Zhang CX, Pan MX, Li B, Wang L, Mo XF, Chen YM, Lin FY, Ho SC (2013) Choline and betaine intake is inversely associated with breast cancer risk: a two-stage case-control study in China. Cancer Sci 104(2):250–258. https://doi.org/10.1111/cas.12064
Cho E, Holmes MD, Hankinson SE, Willett WC (2010) Choline and betaine intake and risk of breast cancer among post-menopausal women. Br J Cancer 102(3):489–494. https://doi.org/10.1038/sj.bjc.6605510
Ying J, Rahbar MH, Hallman DM, Hernandez LM, Spitz MR, Forman MR, Gorlova OY (2013) Associations between dietary intake of choline and betaine and lung cancer risk. PLoS ONE 8(2):e54561. https://doi.org/10.1371/journal.pone.0054561
Kotsopoulos J, Hankinson SE, Tworoger SS (2010) Dietary betaine and choline intake are not associated with risk of epithelial ovarian cancer. Eur J Clin Nutr 64(1):111–114. https://doi.org/10.1038/ejcn.2009.109
Lee JE, Giovannucci E, Fuchs CS, Willett WC, Zeisel SH, Cho E (2010) Choline and betaine intake and the risk of colorectal cancer in men. Cancer Epidemiol Biomarkers Prev 19(3):884–887. https://doi.org/10.1158/1055-9965.EPI-09-1295
Lu MS, Fang YJ, Pan ZZ, Zhong X, Zheng MC, Chen YM, Zhang CX (2015) Choline and betaine intake and colorectal cancer risk in Chinese population: a case-control study. PLoS ONE 10(3):e0118661. https://doi.org/10.1371/journal.pone.0118661
Yan J, Jiang X, West AA, Perry CA, Malysheva OV, Devapatla S, Pressman E, Vermeylen F, Stabler SP, Allen RH, Caudill MA (2012) Maternal choline intake modulates maternal and fetal biomarkers of choline metabolism in humans. Am J Clin Nutr 95(5):1060–1071. https://doi.org/10.3945/ajcn.111.022772
Myte R, Gylling B, Schneede J, Ueland PM, Häggström J, Hultdin J, Hallmans G, Johansson I, Palmqvist R, Van Guelpen B (2016) Components of one-carbon Metabolism Other than Folate and Colorectal Cancer Risk. Epidemiology 27(6):787–796. https://doi.org/10.1097/EDE.0000000000000529
Bao Q, He BS, Chen LP, Gu L, Nie ZL, Wang SK (2012) Correlation between polymorphism in the promoter of DNA methyltransferase-3B and the risk of colorectal cancer. Zhonghua Yu Fang Yi Xue Za Zhi 46(1):53–57 PMID: 22490141
da Costa KA, Niculescu MD, Craciunescu CN, Fischer LM, Zeisel SH (2006) Choline deficiency increases lymphocyte apoptosis and DNA damage in humans. Am J Clin Nutr 84:88–94. https://doi.org/10.1093/ajcn/84.1.88
Mokarram P, Naghibalhossaini F, Firoozi MS, Hosseini SV, Izadpanah A, Salahi H, Malek-Hosseini SA, Talei A, Mojallal M (2008) Methylenetetrahydrofolate reductase C677T genotype affects promoter methylation of tumor-specific genes in sporadic colorectal cancer through an interaction with folate/vitamin B12 status. World J Gastroenterol 14(23):3662–3671. https://doi.org/10.3748/wjg.14.3662
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJ, den Heijer M, Kluijtmans LA, van den Heuvel LP, Rozen R (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 10(1):111–113. https://doi.org/10.1038/ng0595-111
Ma J, Stampfer MJ, Hennekens CH, Frosst P, Selhub J, Horsford J, Malinow MR, Willett WC, Rozen R (1996) Methylenetetrahydrofolate reductase polymorphism, plasma folate, homocysteine, and risk of myocardial infarction in US physicians. Circulation 94(10):2410–2416. https://doi.org/10.1161/01.cir.94.10.2410
Razzak AA, Oxentenko AS, Vierkant RA, Tillmans LS, Wang AH, Weisenberger DJ, Laird PW, Lynch CF, Anderson KE, French AJ, Haile RW, Harnack LJ, Potter JD, Slager SL, Smyrk TC, Thibodeau SN, Cerhan JR, Limburg PJ (2012) Associations between intake of folate and related micronutrients with molecularly defined colorectal cancer risks in the Iowa women’s Health Study. Nutr Cancer 64(7):899–910. https://doi.org/10.1080/01635581.2012.714833
Panprathip P, Petmitr S, Tungtrongchitr R, Kaewkungwal J, Kwanbunjan K (2019) Low folate status, and MTHFR 677C > T and MTR 2756A > G polymorphisms associated with colorectal cancer risk in Thais: a case-control study. Nutr Res 72:80–91. https://doi.org/10.1016/j.nutres.2019.10.008
Castelló A, Amiano P, Fernández de Larrea N, Martín V, Alonso MH, Castaño-Vinyals G, Pérez-Gómez B, Olmedo-Requena R, Guevara M, Fernandez-Tardon G, Dierssen-Sotos T, Llorens-Ivorra C, Huerta JM, Capelo R, Fernández-Villa T, Díez-Villanueva A, Urtiaga C, Castilla J, Jiménez-Moleón JJ, Moreno V, Dávila-Batista V, Kogevinas M, Aragonés N, Pollán M (2019) MCC-Spain researchers. Low adherence to the western and high adherence to the Mediterranean dietary patterns could prevent colorectal cancer. Eur J Nutr 58(4):1495–1505. https://doi.org/10.1007/s00394-018-1674-5
Feldblyum IV, Alyeva MK, Markovich NI (2016) The association between diet and the probability of colorectal cancer among the population of Perm Krai: epidemiological study. Vopr Pitan 85(5):60–67 PMID: 29381303
Vereecken CA, Covents M, Sichert-Hellert W, Alvira JM, Le Donne C, De Henauw S, De Vriendt T, Phillipp MK, Béghin L, Manios Y, Hallström L, Poortvliet E, Matthys C, Plada M, Nagy E, Moreno LA, HELENA Study Group (2008) Development and evaluation of a self-administered computerized 24-h dietary recall method for adolescents in Europe. Int J Obes (Lond) 32(Suppl 5):S26–34. https://doi.org/10.1038/ijo.2008.180
Anderson AS, Steele R, Coyle J (2013) Lifestyle issues for colorectal cancer survivors–perceived needs, beliefs and opportunities. Support Care Cancer 21(1):35–42. https://doi.org/10.1007/s00520-012-1487-7
Berstad P, Løberg M, Larsen IK, Kalager M, Holme Ø, Botteri E, Bretthauer M, Hoff G (2015) Long-term lifestyle changes after colorectal cancer screening: randomised controlled trial. Gut 64(8):1268–1276. https://doi.org/10.1136/gutjnl-2014-307376
Acknowledgements
The author would like to thank the patients who enrolled in this study for their participation, and the DNA Bank unit of the General Genomics and Proteomics Service at the UPV/EHU and the Basque Biobank for Research-OEHUN for its collaboration. The genotyping service was carried out at CEGEN-PRB2-ISCIII; it is supported by grant PT13/0001, ISCIII-SGEFI / FEDER.
Funding
This research was funded by the Basque Government: Department of Health and Consumer Affairs (2011111153), the Saiotek program (S-PE12UN058), and Education Department (BIOMICs Research Group, MICROFLUIDICs & BIOMICs Cluster of the University of the Basque Country UPV/EHU, No. IT1633-22). I.A.-L. was founded by a pre-doctoral grant from the Basque Government (PRE_2014_1_161, PRE_2015_2_0084, EP_2016_1_0098, EP_2016_1_0098, and PRE_2017_2_0006). Open Access funding provided by the University of the Basque Country UPV/EHU. The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
Marta Arroyo-Izaga: conceptualisation, data curation, formal analysis, software, resources, project administration, writing-original draft, validation, visualisation, writing review & editing, funding acquisition, and supervision. Iker Alegria-Lertxundi: conceptualisation, data curation, formal analysis, software, writing-original draft, and writing review & editing. Sara Corchero-Palacios: formal analysis, and writing-original draft. Marian M. de Pancorbo: conceptualisation, validation, visualisation, writing review & editing, funding acquisition, and supervision. The work reported in the paper has been performed by the authors unless clearly specified in the text.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics Statement
The study was approved by the Clinical Research Ethics Committee of the Basque Country (protocol code PI2011006, data of approval 03/23/2012; and PI2014042, data of approval 05/28/2014). All participants gave written informed consent before enrolment in the study, which was conducted in accordance with the principles of the Declaration of Helsinki.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Corchero-Palacios, S., Alegria-Lertxundi, I., de Pancorbo, M.M. et al. Interactions between folate metabolism-related nutrients and polymorphisms on colorectal cancer risk: a case-control study in the Basque country. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03371-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03371-5