Abstract
Purpose
Fish and shellfish consumption is suggested to be a cancer-protective factor. However, studies investigating this association for gastric cancer, especially considering Helicobacter pylori (H. pylori) and atrophic gastritis (AG), are limited. We investigated gastric cancer risk associated with fish, shellfish, and n-3 polyunsaturated fatty acids (n-3 PUFAs) consumption among Japanese adults.
Methods
90,504 subjects enrolled in the Japan Public Health Center-based Prospective Study (JPHC Study) were followed until December 2013. Dietary intake data were collected using a food frequency questionnaire. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated for gastric cancer risk associated with fish and shellfish consumption and marine n-3 PUFAs (sum of eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA)) using Cox proportional hazards models. Among those with avaliable data, we conducted a subgroup analysis taking H. pylori infection and AG status into consideration.
Results
There were 2,701 gastric cancer cases during an average of 15 years of follow-up. We observed an increased gastric cancer risk for salted fish consumption for men [HR for fifth quintile versus first quintile 1.43 (95% CI 1.18–1.75)] and for women [HR 1.33 (95% CI 1.00–1.77)]. We observed a weak risk reduction trend for women as the intake of marine n-3 PUFAs increased (p-trend:0.07). When we included H. pylori infection and atrophic gastritis status in the analysis, the associations diminished.
Conclusion
Our results suggest that salted fish increases gastric cancer risk for men and women, while marine n-3 PUFAs marginally decreases this risk among women in Japan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fifth-most common and fourth-most lethal cancer worldwide, with over 1 million new cases and 770,000 deaths in 2020 [1]. The highest age-standardised incident rates (ASIRs) for gastric cancer, calculated per 100,000 person-years are observed in eastern Asia (32.5 for men; 13.2 for women), where 60% of all gastric cancers occur [1, 2]. Given this high burden, it is crucial to identify modifiable risk and protective factors for gastric cancer for better targeted and more effective prevention.
While Helicobacter pylori (H. pylori) infection remains the leading cause of gastric cancer, a 2018 report by the World Cancer Research Fund (WCRF) and the American Institute for Cancer Research (AICR) on the relationship between diet and cancer suggested that consumption of certain food, such as foods preserved by salting, processed meat, or consumption of alcoholic drinks may be associated with gastric cancer development [3].
Diet has received attention in the past decades for its potential role in preventing cancer. Seafood is a part of a diet for many: fish, in particular, is a known source of n-3 polyunsaturated fatty acids (PUFAs) and other nutrients such as vitamin D and selenium [3].
Epidemiological studies have found conflicting results on the association between fish consumption and gastric cancer [4,5,6]. Dietary n-3 PUFAs are reported to suppress mutations, inhibit cell growth, enhance cell apoptosis, and ultimately reduce cancer risk [7]. On the other hand, salted fish, fish that is treated with a combination of brining, dry salting, or pickle curing, have been reported to have a dose-dependent relation with gastric cancer risk [8]. Moreover, grilled or charbroiled fish can contain mutagenic and carcinogenic heterocyclic amines and polycyclic aromatic hydrocarbons, which may increase gastric cancer risk [9, 10]. While the WCRF/AICR reported that high-salt foods and salt-preserved foods have a probable association with gastric cancer risk, the same report concluded that there was limited evidence on the association between gastric cancer and consumption of processed, grilled, or charbroiled fish [3]. A 2011 meta-analysis with 15 case–control studies and two cohort studies [11] found no association between fish consumption and gastric cancer risk (relative risk (RR) 0.87, 95% confidence interval (CI) 0.71–1.07). A 2014 meta-analysis [12] with 27 prospective cohort studies found an inverse association between fish consumption and gastrointestinal cancer risk; however, when they analysed seven cohorts with available data on gastric cancer, 20 grams (g) per day increment of fish slightly increased gastric cancer risk (RR 1.03, 95% CI 1.00–1.05).
The gastric cancer risk associated with fish consumption, other than salted fish roe and fish preserved by salt, remains unclear. Furthermore, limited studies have taken H. pylori infection into consideration while assessing the association between fish and shellfish consumption, n-3 PUFAs, and gastric cancer risk.
Therefore, the aim of this study was to investigate the association between fish and shellfish consumption, and n-3 PUFAs and gastric cancer risk using a Japanese population-based prospective study.
Methods
Study design
The Japan Public Health Center-based Prospective Study (the JPHC Study) is an ongoing cohort study designed to investigate associations between lifestyle habits and non-communicable diseases. The JPHC Study has been described in detail elsewhere [13]. Briefly, the JPHC Study consists of Cohort I, established in 1990, and Cohort II, established in 1993, involving a total of 140,420 individuals (68,722 men, 71,698 women) in 11 public health centres (PHC) nationwide aged 40–69 at the beginning of the baseline survey.
Study population
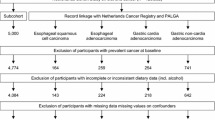
For this study, we included those who responded to a self-administered 5-year follow-up questionnaire between 1995 and 1999, which included comprehensive information on dietary intake and lifestyle-related factors. Figure 1 shows the flow diagram of study participant selection. We excluded participants from Katsushika, Tokyo, due to the lack of cancer incidence information. After excluding those who died or moved out of the study area before the 5-year follow-up survey, non-Japanese nationals, incorrect birthdate, duplicates, cancer diagnosis before the 5-year follow-up survey, non-response, history of any type of cancer, history of gastric surgery, or reported extreme energy intake (men: < 800 or > 4200 kcal; women: < 500 or > 3500 kcal), 90,504 (42,328 men and 48,176 women) participants remained for analysis.
Exposure and covariates
The self-administered questionnaire at the 5-year follow-up collected data on smoking, alcohol consumption, physical activity, anthropometry, and medical history. It also included a comprehensive food frequency questionnaire (FFQ). It covered 138 food and drink items with nine eating frequency categories (never; 1–3 times/month; 1–2 times/week; 3–4 times/week; 5–6 times/week; once/day; 2–3 times/day; 4–6 times/day; ≥ 7 times/day) and three portion sizes (small: 50% smaller than the standard size; medium: standard; large: 50% larger than the standard size). The FFQ also included questions on consumption of 19 seafood items (from here on referred to as fish and shellfish: canned tuna, salmon/trout, bonito/tuna, cod/flatfish, sea bream, horse mackerel/sardines, mackerel pike/mackerel, shirasuboshi (dried young sardines), chikuwa (Japanese fish cake), kamaboko (Japanese cured surimi (minced fish paste)), salted fish, salted fish roe, dried fish, eel, squid, octopus, prawn, short-necked clam, and viviparide). These items were further categorised into: fish (canned tuna, salmon/trout, bonito/tuna, cod/flatfish, sea bream, horse mackerel/sardines, mackerel pike/mackerel, shirasuboshi, salted fish, dried fish, and eel), salted fish (salted pike/mackerel, salted cod/flatfish, salted salmon/trout, salted fish roe, dried fish, and shirasuboshi), and n-3 PUFAs-rich fish (salmon/trout, horse mackerel/sardines, mackerel pike/mackerel, eel, and sea bream, based on the mount of n-3 PUFAs in 100 g (g) edible fish portion). Daily consumption of fish and shellfish, salted fish, and n-3 PUFA-rich fish (measured in g/day) were calculated by multiplying the frequency by relative portion size. For n-3 PUFAs, we focused on eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA), n-3 PUFAs that are often found high in marine food, to look at the association between marine-based n-3 PUFAs and gastric cancer risk [14]. Daily intake of EPA, DPA, and DHA was calculated using Japanese food fatty acid composition tables [15]. The sum of EPA, DPA, and DHA was considered as marine n-3 PUFAs in our study, as about 90% of these n-3 PUFAs consumed among the study participants derived from marine food. All dietary intake variables were log-transformed and adjusted for total energy intake using the residual method and divided into quintiles for both sexes.
FFQ validation for fish,shellfish, and marine n-3 PUFAs were conducted using 14- or 28-day dietary records, which are considered a gold standard. Spearman correlation coefficient for fish and shellfish for Cohort I was men 0.32, women 0.32, and for Cohort II, men 0.27, women 0.23 [16, 17]. Spearman correlation coefficient for marine n-3 PUFAs in Cohort I were EPA: men 0.38, women 0.45; DPA: men 0.32, women 0.39; and DHA: men 0.34, women 0.37 [18]. Reproducibility of the FFQ was evaluated by administering two questionnaires 1 year apart. Spearman correlation coefficient for fish and shellfish for Cohort I was men 0.44, women 0.34, and for Cohort II, men 0.45, women 0.40 [17, 19].
Laboratory analysis
Information on H. pylori infection and atrophic gastritis was available for 31% of participants who provided blood samples at the baseline survey in Cohort II (8,702 men and 15,672 women). H. pylori was measured using plasma immunoglobin G (IgG) level through an enzyme immunoassay (Eiken Kagaku, Tokyo, Japan). IgG titer ≥ 10 U/mL was considered as H. pylori-positive. Atrophic gastritis was defined using plasma levels of pepsinogen I and II, measured by a latex-agglutination assay (Eiken Kagaku, Tokyo, Japan), with pepsinogen I ≤ 70 ng/mL and pepsinogen I/II ratio ≤ 3.0 considered as positive [20].
Follow-up and identification of gastric cancer case
Person-years of follow-up were calculated from the date of the 5-year follow-up survey to the date of gastric cancer diagnosis, death, move out from the study area, or until 31 December 2013 (except Osaka PHC: 31 December 2012), whichever came first. The residential registry was used to confirm residence and survival status. Gastric cancer incidence was identified by active patient notification from major local hospitals in each PHC area and linkage of the record with population-based cancer registries, and were supplemented by death certificates. Gastric cancer was coded using the International Classification of Diseases (ICD) for Oncology, 3rd edition (C16.0 to 16.9) [21]. Residual cases were tumours that could not be classified due to overlapping lesions (C16.8) or no information (C16.9).
Statistical analysis
We used Cox proportional hazards regression models to estimate hazard ratios (HRs) and their 95% confidence intervals (CIs), running multivariable models using the lowest quintile as a reference. We conducted the analysis separately for men and women since gastric cancer incidence is significantly higher in men [22]. The models were adjusted for potential confounders based on previous studies: metabolic equivalent of tasks (METs, continuous), body mass index (BMI, weight (kg)/height(m)2, continuous), total energy, meat consumption (energy-adjusted, continuous), fruit consumption (energy-adjusted, continuous), vegetable consumption (energy-adjusted, continuous), alcohol consumption (main analysis: men: never/former, < 150, 150–299, 300–449, ≥ 450 g ethanol/week; women: never/former, < 150, 150–299, ≥ 300 g ethanol/week; H. pylori and atrophic gastritis analysis: men: never/former, < 150, 150–299, 300–449, ≥ 450 g ethanol/week; women: never/former, current), smoking (never, former, < 20 cigarettes/day, ≥ 20 cigarettes/day), history of diabetes mellitus, use of anti-cholesterol drugs, history of gastric ulcer, and family history of gastric cancer. We used two definitions of salted food depending on the analysis: salted food excluding salted fish, or salted food and salted fish. When evaluating the association between salted fish and gastric cancer, we used salted food excluding salted fish (energy adjusted, continuous). For the analysis on the association between fish other than salted fish and gastric cancer, we used salted food and salted fish (energy adjusted, continuous) to evaluate the effect of salt. Because the consumption of salted food and salted fish varies heavily by the region of Japan [23], we thought that adjusting the model by PHC may mask the true association between fish consumption and gastric cancer. Therefore, we included PHC as a covariate for all models except for salted fish. We tested for linear trends using the median value of each quintile. For salted fish, fish excluding salted fish, and n-3 PUFAs-rich fish analyses, we adjusted for fish excluding salted fish, salted fish, and lean fish consumption, respectively, in addition to the confounding variables listed above. We performed sensitivity analysis by running the same model excluding gastric cancer cases diagnosed within 3 years of follow-up. For multi-variable analysis, we used multiple imputation to impute missing data on METs (3.6%), alcohol consumption (7.7%), smoking status (4.9%), BMI (2.6%), family history of gastric cancer (12.5%), and vegetable intake (0.1%) using the command “mi estimate”, created based on Rubin rules [24]. We assessed interaction between the exposure variables and BMI (< 25, ≥ 25 kg/m2), smoking (never/former, current), and alcohol consumption (never/former, ever) by comparing the model with or without an interaction term using the likelihood ratio test with or without an interaction term. We also conducted an analysis based on the anatomical region of the tumour (proximal, upper one-third of the stomach, versus distal, lower two-thirds of the stomach), based on The Japanese classification of gastric carcinoma, 3rd edition [25].
Among those with available information on H. pylori and atrophic gastritis, we performed subgroup analyses on the association between fish and shellfish consumption and risk of gastric cancer based on the H. pylori infection and atrophic gastritis status. Given that atrophic gastritis is caused by H. pylori infection-related chronic gastritis [26, 27] and the small number of cases, we divided the subjects into four categories based on their H. pylori infection and atrophic gastritis status: H. pylori antibody and atrophic gastritis negative (H. pylori − /AG −), H. pylori antibody positive (H. pylori +), those with atrophic gastritis (AG +), and H. pylori antibody and/or atrophic gastritis positive (H. pylori + and/or AG +).
All analyses were performed using Stata 16.0 (StataCorp LLC).
Results
During an average of 15 years of follow-up, 2701 gastric cancer cases were diagnosed (1868 men and 833 women). Table 1 shows the baseline characteristics of study subjects by fish and shellfish consumption quintile. Compared to the lowest quintile, the higher quintile subjects were older, more likely to have a history of diabetes mellitus, and consumed less alcohol.
Tables 2 and 3 show gastric cancer risk by consumption of fish and shellfish, fish, fish excluding salted fish, salted fish, n-3 PUFAs-rich fish, and marine n-3 PUFAs for men and women, respectively. There was an increase in gastric cancer risk associated with salted fish consumption for men (HR for fifth quintile versus first quintile 1.43 (95% CI 1.18–1.75); p-trend 0.006) (Table 2). Increased gastric cancer risk was also observed in women who consumed salted fish in high quantities (HR for fifth quintile versus first quintile 1.33 (95% CI 1.00–1.77); p-trend 0.21) (Table 3). We observed a weak decrease in gastric cancer risk trend for marine n-3 PUFAs (HR for fifth quintile versus first quintile 0.79 (95% CI 0.62–1.04); p-trend 0.07) (Table 3). Consumption of fish and shellfish, fish excluding salted fish, or n-3 PUFAs-rich fish was not associated with gastric cancer risk. These findings did not change when we conducted a sensitivity analysis which excluded gastric cancer cases occurring within 3 years of follow-up. We found no interaction between fish and shellfish consumption and any of the exposure variables for both men and women (data not shown).
We further analysed the association between consumption of fish and shellfish, fish, fish excluding salted fish, salted fish, n-3 PUFAs-rich fish, and marine n-3 PUFAs based on anatomical region of the tumour. For proximal gastric cancer (n = 218 men and 68 women), none of the fish and shellfish categories, for both men and women, were associated with cancer risk, except for women in the highest quintile of salted fish consumption (HR for fifth quintile versus first quintile 3.02 (95% CI 1.03–8.81); p-trend < 0.10) (data not shown). For distal gastric cancer (n = 1219 men and 552 women), consumption of salted fish increased the cancer risk for men, as in the findings from the main analysis (HR for fifth quintile versus first quintile 1.68 (95% CI 1.31–2.14); p-trend < 0.001) (data not shown). No clear associations were observed for other fish and shellfish or with marine n-3 PUFAs with distal gastric cancer risk.
Association between fish and shellfish consumption and gastric cancer risk considering H. pylori infection and atrophic gastritis status
17,583 subjects (6192 men and 11,391 women) had information on H. pylori infection status and atrophic gastritis, among whom 482 cases of gastric cancer (288 men and 194 women) were identified during follow-up. The baseline characteristics of subjects in the subgroup analysis were similar to those in the main analysis. Tables 4 and 5 show gastric cancer risk from consumption of fish and shellfish, fish, fish excluding salted fish, salted fish, n-3 PUFAs-rich fish, and marine n-3 PUFAs for men and women, taking H. pylori infection and atrophic gastritis into consideration. There were only 1,511 women who drank alcohol; therefore, we modified the alcohol consumption categories to never/former and current for women’s analysis. We observed similar findings to those of the main analysis; an increased gastric cancer risk trend with salted fish consumption for men in the analysis not taking H. pylori or atrophic gastritis into consideration (HR for fifth quintile versus first quintile 1.62 (95% CI 0.98–2.65); p-trend 0.04) (Table 4). For the analysis by H. pylori and atrophic gastritis status, we could not observe an association for H. pylori − / AG − due to lack of gastric cancer cases (n = 23 men and eight women). For men, the association between salted fish and gastric cancer risk diminished once H. pylori infection and atrophic gastritis status were taken into consideration. For women, similar to the main analysis, none of the fish and shellfish categories considered in our study were associated with gastric cancer risk.
Discussion
In this study, we aimed to determine the association between fish and shellfish consumption and gastric cancer risk among a Japanese population. We found an increase in gastric cancer risk with salted fish consumption for both men and women. When H. pylori infection and atrophic gastritis status were considered, none of the fish and shellfish consumption categories, for both men and women, were associated with gastric cancer risk.
While limited studies have assessed the association between gastric cancer risk and fish or n-3 PUFAs, our study findings are in line with previous studies [11, 12]. In a Japanese setting, the Japan Collaborative Cohort Study have evaluated associations between 33 food items and gastric cancer risk. While the study found no clear association between fish and gastric cancer, a non-significant increase in risk was observed among women in the third-highest fish consumption category (HR 1.62 (95% CI 0.95 – 2.75)) [28].
Previous JPHC study have also shown an increase in gastric cancer risk with salted fish consumption for men [8]. The current study, with a longer follow-up period and larger sample size, observed an increased gastric cancer risk for both men and women. High salt concentration in the intra-gastric region could destroy the mucosal barrier, causing inflammation and damage. This would in turn lead to symptoms such as diffuse erosion and degeneration of mucosa that could induce proliferous changes and enhance food-derived carcinogenetic effects [29]. Mucosa damage could also enhance H. pylori colonisation though gastric mucosa damage, increasing the risk of gastric cancer [30, 31].
In the main analysis, we also observed a borderline significant decreasing trend in gastric cancer risk for marine n-3 PUFAs for women. One possible mechanism of how marine n-3 PUFAs could reduce gastric cancer risk is through suppression of inflammation. Dietary n-3 PUFAs can be metabolised into prostaglandins, thromboxanes, hydroxyeicosatetraenoic acids and leukotrienes, which possess anti-inflammatory and immune-regulatory characteristics through enzymatic activity [32]. n-3 PUFAs can also be metabolised into resolvins and protectins, which also have anti-inflammatory and immune-regulatory characteristics [33, 34].
The significant associations in our main analysis disappeared in the subgroup analysis which considered H. pylori infection and atrophic gastritis status. This suggests that H. pylori infection is the strongest risk factor for gastric cancer onset.
The major strength of this study is its use of a prospective cohort of a large sample of subjects recruited from the general population. Given the long follow-up period (average 15 years), high follow-up questionnaire response rate, low loss to follow-up, and provision of cancer cases from population-based cancer registries, we believe that gastric cancer cases were sufficiently identified. We used gastric cancer incidence as an end point instead of death to directly measure gastric cancer risk. We conducted a sensitivity analysis which excluded gastric cancer cases diagnosed within 3 years of follow-up, which further validates our findings. Having information on atrophic gastritis and H. pylori infection using a blood test allowed us to adjust for the strongest gastric cancer risk factor.
There were several limitations in our study. Most subjects of the JPHC studies were recruited in non-metropolitan areas, which may have led to a geographically biased result that may not be applicable to the general population. Atrophic gastritis and H. pylori status were only available for a subgroup of subjects, and due to the limited number of cases we were unable to look at the association for those who tested negative to both H. pylori and atrophic gastritis. However, given that H. pylori prevalence among those who were born before 1950 was over 80% in Japan [35], we believe our findings are valid. FFQ validity for fish and marine n-3 PUFAs intake was moderate, which may have introduced measurement error and non-deferential misclassification, biasing the HRs towards the null. We did not have information on how the fish was cooked, and thus were not able to perform the analysis based on the cooking method. Lastly, while we were not able to obtain the date of cancer diagnosis for those who the diagnosis was notified through death certificate notification [DCN, n = 159 (5.9%)] or death certification only [DCO, n = 114 (4.2%)], given the low percentage of DCN and DCO cases, we believe we were able to identify sufficient number of cancer cases that represent the population.
Despite the limitations, we believe we have provided new insights into the association between fish and shellfish consumption and gastric cancer risk. There may be other mechanisms through which fish consumption may be protective of gastric cancer. More studies are needed to understand the true association between fish, shellfish, and gastric cancer risk, especially in Asian countries, where seafood consumption is high.
Data availability
For information on data availability, please refer to this link: https://epi.ncc.go.jp/en/jphc/805/8155.html.
Abbreviations
- 95% CI:
-
95% Confidence intervals
- AG:
-
Atrophic gastritis
- DHA:
-
Docosahexaenoic acid
- DPA:
-
Docosapentaenoic acid
- EPA:
-
Eicosapentaenoic acid
- HR:
-
Hazard ratio
- H. pylori :
-
Helicobacter pylori
- The JPHC Study:
-
The Japan Public Health Center-based Prospective Study
- PHC:
-
Public health center
- PUFAs:
-
Polyunsaturated fatty acids
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Morgan E, Arnold M, Camargo MC, Gini A, Kunzmann AT, Matsuda T, Meheus F, Verhoeven RHA, Vignat J, Laversanne M, Ferlay J, Soerjomataram I (2022) The current and future incidence and mortality of gastric cancer in 185 countries, 2020: a population-based modelling study. eClinicalMedicine. https://doi.org/10.1016/j.eclinm.2022.101404
World Cancer Research Fund/American Institute for Cancer Research (2018) Continuous Update Project Expert Report 2018. Diet, nutrition, physical activity and stomach cancer
Chen H, Ward MH, Graubard BI, Heineman EF, Markin RM, Potischman NA, Russell RM, Weisenburger DD, Tucker KL (2002) Dietary patterns and adenocarcinoma of the esophagus and distal stomach. Am J Clin Nutr 75(1):137–144. https://doi.org/10.1093/ajcn/75.1.137
Pourfarzi F, Whelan A, Kaldor J, Malekzadeh R (2009) The role of diet and other environmental factors in the causation of gastric cancer in Iran–a population based study. Int J Cancer 125(8):1953–1960. https://doi.org/10.1002/ijc.24499
Hu J, La Vecchia C, DesMeules M, Negri E, Mery L (2008) Meat and fish consumption and cancer in Canada. Nutr Cancer 60(3):313–324. https://doi.org/10.1080/01635580701759724
Fernandez E, Chatenoud L, La Vecchia C, Negri E, Franceschi S (1999) Fish consumption and cancer risk. Am J Clin Nutr 70(1):85–90. https://doi.org/10.1093/ajcn/70.1.85
Tsugane S, Sasazuki S, Kobayashi M, Sasaki S (2004) Salt and salted food intake and subsequent risk of gastric cancer among middle-aged Japanese men and women. Br J Cancer 90(1):128–134. https://doi.org/10.1038/sj.bjc.6601511
Skog KI, Johansson MA, Jägerstad MI (1998) Carcinogenic heterocyclic amines in model systems and cooked foods: a review on formation, occurrence and intake. Food Chem Toxicol 36(9–10):879–896. https://doi.org/10.1016/s0278-6915(98)00061-1
Sugimura T, Nagao M, Wakabayashi K (1994) Heterocyclic amines in cooked foods: candidates for causation of common cancers. J Natl Cancer Inst 86(1):2–4. https://doi.org/10.1093/jnci/86.1.2
Wu S, Liang J, Zhang L, Zhu X, Liu X, Miao D (2011) Fish consumption and the risk of gastric cancer: systematic review and meta-analysis. BMC Cancer 11:26–26. https://doi.org/10.1186/1471-2407-11-26
Yu X-F, Zou J, Dong J (2014) Fish consumption and risk of gastrointestinal cancers: a meta-analysis of cohort studies. World J Gastroenterol 20(41):15398–15412. https://doi.org/10.3748/wjg.v20.i41.15398
Tsugane S, Sawada N (2014) The JPHC study: design and some findings on the typical Japanese diet. Jpn J Clin Oncol 44(9):777–782. https://doi.org/10.1093/jjco/hyu096
Nguyen QV, Malau-Aduli BS, Cavalieri J, Malau-Aduli AEO, Nichols PD (2019) Enhancing omega-3 long-chain polyunsaturated fatty acid content of dairy-derived foods for human consumption. Nutrients. https://doi.org/10.3390/nu11040743
Science and Technology Agency (1990) Fatty acids, cholesterol, vitamin E composition tables of Japanese foods (Japanese). Ishiyaku Shuppan, Tokyo, Japan
Sasaki S, Kobayashi M, Tsugane S (2003) Validity of a self-administered food frequency questionnaire used in the 5-year follow-up survey of the JPHC study cohort I: comparison with dietary records for food groups. J Epidemiol 13(1sup):57–63. https://doi.org/10.2188/jea.13.1sup_57
Ishihara J, Sobue T, Yamamoto S, Yoshimi I, Sasaki S, Kobayashi M, Takahashi T, Iitoi Y, Akabane M, Tsugane S (2003) Validity and reproducibility of a self-administered food frequency questionnaire in the JPHC Study Cohort II: study design, participant profile and results in comparison with Cohort I. J Epidemiol 13(1 Suppl):S134-147. https://doi.org/10.2188/jea.13.1sup_134
Kobayashi M, Sasaki S, Kawabata T, Hasegawa K, Tsugane S (2003) Validity of a self-administered food frequency questionnaire used in the 5-year follow-up survey of the JPHC study cohort I to assess fatty acid intake: comparison with dietary records and serum phospholipid level. J Epidemiol 13(1sup):64–81. https://doi.org/10.2188/jea.13.1sup_64
Sasaki S, Ishihara J, Tsugane S (2003) Reproducibility of a self-administered food frequency questionnaire used in the 5-year follow-up survey of the JPHC study cohort I to assess food and nutrient intake. J Epidemiol 13(1sup):115–124. https://doi.org/10.2188/jea.13.1sup_115
Miki K (2006) Gastric cancer screening using the serum pepsinogen test method. Gastric cancer : official journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 9(4):245–253. https://doi.org/10.1007/s10120-006-0397-0
World Health Organization (2013) International classification of diseases for oncology (ICD-O). 3rd ed., 1 revision. World Health Organization, Geneva
Lou L, Wang L, Zhang Y, Chen G, Lin L, Jin X, Huang Y, Chen J (2020) Sex difference in incidence of gastric cancer: an international comparative study based on the Global Burden of Disease Study 2017. BMJ Open 10(1):e033323. https://doi.org/10.1136/bmjopen-2019-033323
Tsugane S, Sasaki S, Kobayashi M, Tsubono Y, Sobue T (2001) Dietary habits among the JPHC study participants at baseline survey. Japan Public Health Center-based Prospective Study on Cancer and Cardiovascular Diseases. J Epidemiol 11(6 Suppl):S30-43. https://doi.org/10.2188/jea.11.6sup_30
StataCorp (2021) Data multiple-imputation reference manual: release 17. Stata Press, College Station
(2011)J apanese classification of gastric carcinoma: 3rd English edition. Gastric cancer 14 (2):101–112. doi: https://doi.org/10.1007/s10120-011-0041-5
Kuipers EJ, Uyterlinde AM, Peña AS, Roosendaal R, Pals G, Nelis GF, Festen HP, Meuwissen SG (1995) Long-term sequelae of Helicobacter pylori gastritis. Lancet 345(8964):1525–1528. https://doi.org/10.1016/s0140-6736(95)91084-0
Karnes WE Jr, Samloff IM, Siurala M, Kekki M, Sipponen P, Kim SW, Walsh JH (1991) Positive serum antibody and negative tissue staining for Helicobacter pylori in subjects with atrophic body gastritis. Gastroenterology 101(1):167–174. https://doi.org/10.1016/0016-5085(91)90474-y
Tokui N, Yoshimura T, Fujino Y, Mizoue T, Hoshiyama Y, Yatsuya H, Sakata K, Kondo T, Kikuchi S, Toyoshima H, Hayakawa N, Kubo T, Tamakoshi A (2005) Dietary habits and stomach cancer risk in the JACC Study. J Epidemiol 15 Suppl 2(II):S98-108. https://doi.org/10.2188/jea.15.s98
Kato S, Tsukamoto T, Mizoshita T, Tanaka H, Kumagai T, Ota H, Katsuyama T, Asaka M, Tatematsu M (2006) High salt diets dose-dependently promote gastric chemical carcinogenesis in Helicobacter pylori-infected Mongolian gerbils associated with a shift in mucin production from glandular to surface mucous cells. Int J Cancer 119(7):1558–1566. https://doi.org/10.1002/ijc.21810
Toyoda T, Tsukamoto T, Yamamoto M, Ban H, Saito N, Takasu S, Shi L, Saito A, Ito S, Yamamura Y, Nishikawa A, Ogawa K, Tanaka T, Tatematsu M (2013) Gene expression analysis of a Helicobacter pylori-infected and high-salt diet-treated mouse gastric tumor model: identification of CD177 as a novel prognostic factor in patients with gastric cancer. BMC Gastroenterol 13:122. https://doi.org/10.1186/1471-230x-13-122
Gaddy JA, Radin JN, Loh JT, Zhang F, Washington MK, Peek RM Jr, Algood HM, Cover TL (2013) High dietary salt intake exacerbates Helicobacter pylori-induced gastric carcinogenesis. Infect Immun 81(6):2258–2267. https://doi.org/10.1128/iai.01271-12
Calder PC, Yaqoob P, Thies F, Wallace FA, Miles EA (2002) Fatty acids and lymphocyte functions. Br J Nutr 87(Suppl 1):S31-48. https://doi.org/10.1079/bjn2001455
Wall R, Ross RP, Fitzgerald GF, Stanton C (2010) Fatty acids from fish: the anti-inflammatory potential of long-chain omega-3 fatty acids. Nutr Rev 68(5):280–289. https://doi.org/10.1111/j.1753-4887.2010.00287.x
Serhan CN, Gotlinger K, Hong S, Lu Y, Siegelman J, Baer T, Yang R, Colgan SP, Petasis NA (2006) Anti-inflammatory actions of neuroprotectin D1/protectin D1 and its natural stereoisomers: assignments of dihydroxy-containing docosatrienes. J Immunol 176(3):1848–1859. https://doi.org/10.4049/jimmunol.176.3.1848
Asaka M, Kimura T, Kudo M, Takeda H, Mitani S, Miyazaki T, Miki K, Graham DY (1992) Relationship of Helicobacter pylori to serum pepsinogens in an asymptomatic Japanese population. Gastroenterology 102(3):760–766. https://doi.org/10.1016/0016-5085(92)90156-S
Acknowledgements
We would like to thank Aomori, Iwate, Ibaraki, Niigata, Osaka, Kochi, Nagasaki, and Okinawa Cancer Registries for providing their incidence data.
Funding
This study was supported by the National Cancer Center Research and Development Fund (23-A-31[toku], 26-A-2 and 29-A-4, 2020-J-4 since 2011) and a Grant-in-Aid for Cancer Research from the Ministry of Health, Labour and Welfare of Japan (1989 to 2010).
Author information
Authors and Affiliations
Consortia
Contributions
MH, CW, MI*, and NS designed the study. MH and CW analysed the data. MH generated tables and drafted the manuscript. NS and UM helped with the nutritional aspects of the study. CW, UM, TY, MIw, MI*, ST, and NS contributed to the interpretation of the results. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical standards
All JPHC Study participants were informed of the objectives of the study. Those who completed the survey questionnaire were regarded as consenting to participate in the study. The study protocol was approved by the Institutional Review Board of the National Cancer Centre, Tokyo, Japan (approval number: 2001–021).
Additional information
The JPHC Study Group members are listed here: https://epi.ncc.go.jp/en/jphc/781/8896.html (Oct 2022).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hirabayashi, M., Wilunda, C., Murai, U. et al. Association between fish and shellfish consumption, n-3 polyunsaturated fatty acids, and gastric cancer risk: the Japan Public Health Center-based Prospective Study. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03343-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03343-9