Abstract
Purpose
A significant shift in meal pattern with frequent eating out was closely associated with multiple chronic outcomes, but with limited evidence on hyperuricemia. We aimed to explore the associations between eating out and serum uric acid (SUA) as well as hyperuricemia.
Methods
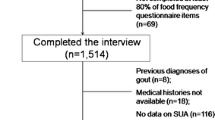
A total of 29,597 participants were recruited from the Henan Rural Cohort Study. A validated food frequency questionnaire (FFQ) was used to collect dietary data, including the frequency of eating out. Linear regression models were used to examine the association of eating-out frequency with SUA and BMI. Logistic regression and restricted cubic spline were performed to assess the association and dose–response relationship between eating-out frequency and hyperuricemia. The mediation effect of BMI between eating out and the risk of hyperuricemia was evaluated.
Results
Eating out was significantly associated with higher SUA levels in the total population and males (P < 0.001). Multivariate-adjusted odds ratios (ORs) with 95% confidence interval (CIs) of hyperuricemia were 1.26 (1.09, 1.46) for the total population and 1.18 (1.00, 1.40) for males (≥ 7 times/week vs 0 time/week). A non-linear positive dose–response relationship between eating-out frequency and hyperuricemia was observed. Furthermore, BMI played a partial mediating role in the relationship between eating out frequency and hyperuricemia, which explained 30.7% in the total population and 44.8% in males.
Conclusion
Our findings indicated that eating out was associated with increased SUA levels and elevated hyperuricemia risk in rural China, especially in males. Moreover, the relationship was partly mediated by BMI.
Clinical trials
ChiCTR-OOC-15006699 (2015-07-06).



Similar content being viewed by others
Availability of data and material
The data are available from the corresponding author on reasonable request. Contact Dr. Chongjian Wang (tjwcj2005@126.com) for additional information regarding data access.
Code availability
Not applicable.
References
Becerra-Tomás N, Mena-Sánchez G, Díaz-López A et al (2020) Cross-sectional association between non-soy legume consumption, serum uric acid and hyperuricemia: the PREDIMED-Plus study. Eur J Nutr 59(5):2195–2206. https://doi.org/10.1007/s00394-019-02070-w
Masseoud D, Rott K, Liu-Bryan R, Agudelo C (2005) Overview of hyperuricaemia and gout. Curr Pharm Des 11(32):4117–4124. https://doi.org/10.2174/138161205774913318
Shiozawa A, Szabo SM, Bolzani A, Cheung A, Choi HK (2017) Serum uric acid and the risk of incident and recurrent gout: a systematic review. J Rheumatol 44(3):388–396. https://doi.org/10.3899/jrheum.160452
Kanbay M, Jensen T, Solak Y, Le M, Roncal-Jimenez C, Rivard C, Lanaspa MA, Nakagawa T, Johnson RJ (2016) Uric acid in metabolic syndrome: from an innocent bystander to a central player. Eur J Intern Med 29:3–8. https://doi.org/10.1016/j.ejim.2015.11.026
Lee SY, Park W, Suh YJ, Lim MJ, Kwon SR, Lee JH, Joo YB, Oh YK, Jung KH (2019) Association of serum uric acid with cardiovascular disease risk scores in Koreans. Int J Environ Res Public Health 16(23):4632. https://doi.org/10.3390/ijerph16234632
Wardhana W, Rudijanto A (2018) Effect of uric acid on blood glucose levels. Acta Med Indones 50(3):253–256
Shah P, Bjornstad P, Johnson RJ (2016) Hyperuricemia as a potential risk factor for type 2 diabetes and diabetic nephropathy. J Bras Nefrol 38(4):386–387. https://doi.org/10.5935/0101-2800.20160061
Cicero AFG, Fogacci F, Desideri G, Grandi E, Rizzoli E, D’Addato S, Borghi C (2019) Arterial stiffness, sugar-sweetened beverages and fruits intake in a rural population sample: data from the Brisighella Heart Study. Nutrients 11(11):2674. https://doi.org/10.3390/nu11112674
Liu R, Han C, Wu D, Xia X, Gu J, Guan H, Shan Z, Teng W (2015) Prevalence of hyperuricemia and gout in mainland China from 2000 to 2014: a systematic review and meta-analysis. Biomed Res Int 2015:762820. https://doi.org/10.1155/2015/762820
Lu J, Sun W, Cui L, Li X, He Y, Liu Z, Li H, Han L, Ji A, Wang C, Zhang H, Ji X, Ren W, Wang X, Li C (2020) A cross-sectional study on uric acid levels among Chinese adolescents. Pediatr Nephrol 35(3):441–446. https://doi.org/10.1007/s00467-019-04357-w
Healey LA, Skeith MD, Decker JL, Bayani-Sioson PS (1967) Hyperuricemia in Filipinos: interaction of heredity and environment. Am J Hum Genet 19(2):81–85
Zeng J, Zhang J, Li Z, Li T, Li G (2020) Prediction model of artificial neural network for the risk of hyperuricemia incorporating dietary risk factors in a Chinese adult study. Food Nutr Res. https://doi.org/10.29219/fnr.v64.3712
Gao Y, Cui LF, Sun YY, Yang WH, Wang JR, Wu SL, Gao X (2020) Adherence to the dietary approaches to stop hypertension (DASH) diet and hyperuricemia: a cross-sectional Study. Arthritis Care Res (Hoboken). https://doi.org/10.1002/acr.24150
Kaneko K, Aoyagi Y, Fukuuchi T, Inazawa K, Yamaoka N (2014) Total purine and purine base content of common foodstuffs for facilitating nutritional therapy for gout and hyperuricemia. Biol Pharm Bull 37(5):709–721. https://doi.org/10.1248/bpb.b13-00967
Han QX, Zhang D, Zhao YL, Liu L, Li J, Zhang F, Luan FX, Liu DW, Liu ZS, Cai GY, Chen XM, Zhu HY (2019) Risk factors for hyperuricemia in Chinese centenarians and near-centenarians. Clin Interv Aging 14:2239–2247. https://doi.org/10.2147/cia.S223048
Mottaleb KA, Rahut DB, Mishra AK (2017) Consumption of food away from home in Bangladesh: do rich households spend more? Appetite 119:54–63. https://doi.org/10.1016/j.appet.2017.03.030
Anderson B, Rafferty AP, Lyon-Callo S, Fussman C, Imes G (2011) Fast-food consumption and obesity among Michigan adults. Prev Chronic Dis 8(4):A71
Adams J, Goffe L, Brown T, Lake AA, Summerbell C, White M, Wrieden W, Adamson AJ (2015) Frequency and socio-demographic correlates of eating meals out and take-away meals at home: cross-sectional analysis of the UK national diet and nutrition survey, waves 1–4 (2008-12). Int J Behav Nutr Phys Act 12:51. https://doi.org/10.1186/s12966-015-0210-8
Xue H, Wu Y, Wang X, Wang Y (2016) Time trends in fast food consumption and its association with obesity among children in China. PLoS ONE 11(3):e0151141. https://doi.org/10.1371/journal.pone.0151141
Ayala GX, Rogers M, Arredondo EM, Campbell NR, Baquero B, Duerksen SC, Elder JP (2008) Away-from-home food intake and risk for obesity: examining the influence of context. Obesity (Silver Spring) 16(5):1002–1008. https://doi.org/10.1038/oby.2008.34
Wang B, Liu L, Qiao D, Xue Y, Liu X, Zhang D, Liu C, Mao Z, Yu S, Shen F, Zhang Y, Wang C, Li W, Li X (2020) The association between frequency of away-from home meals and type 2 diabetes mellitus in rural Chinese adults: the Henan Rural Cohort Study. Eur J Nutr. https://doi.org/10.1007/s00394-020-02212-5
Oh C, Kim HS, No JK (2015) Impact of dining out on nutritional intake and metabolic syndrome risk factors: data from the 2011 Korean National Health and Nutrition Examination Survey. Br J Nutr 113(3):473–478. https://doi.org/10.1017/s0007114514003870
Deng B, Luo T, Huang Y, Shen T, Ma J (2012) Prevalence and determinants of hyperlipidemia in moderate altitude areas of the Yunnan-Kweichow plateau in Southwestern China. High Alt Med Biol 13(1):13–21. https://doi.org/10.1089/ham.2011.1037
Zheng X, Chen J, Xie T, Xia Z, Loo WTY, Lao L, You J, Yang J, Tsui K, Mo F, Gao F (2017) Relationship between Chinese medicine dietary patterns and the incidence of breast cancer in Chinese women in Hong Kong: a retrospective cross-sectional survey. Chin Med 12:17. https://doi.org/10.1186/s13020-017-0138-9
Liu Z, Su X, Xiao M, Zhou P, Guo J, Huang Y, Zhan Y (2019) Association between eating away from home and hyperuricemia: a population-based nationwide cross-sectional study in China. Biomed Res Int 2019:2792681. https://doi.org/10.1155/2019/2792681
Dong X, Zhang H, Wang F, Liu X, Yang K, Tu R, Wei M, Wang L, Mao Z, Zhang G, Wang C (2020) Epidemiology and prevalence of hyperuricemia among men and women in Chinese rural population: the Henan Rural Cohort Study. Mod Rheumatol 30(5):910–920. https://doi.org/10.1080/14397595.2019.1660048
Zeng Q, Zeng Y (2018) Eating out and getting fat? A comparative study between urban and rural China. Appetite 120:409–415. https://doi.org/10.1016/j.appet.2017.09.027
Liu X, Mao Z, Li Y, Wu W, Zhang X, Huo W, Yu S, Shen L, Li L, Tu R, Wu H, Li H, He M, Liu L, Wei S, Li W, Wu T, Wang C (2019) Cohort profile: the Henan Rural Cohort: a prospective study of chronic non-communicable diseases. Int J Epidemiol 48(6):1756–1756j. https://doi.org/10.1093/ije/dyz039
Xue Y, Yang K, Wang B, Liu C, Mao Z, Yu S, Li X, Wang Y, Sun H, Wang C, Li W (2020) Reproducibility and validity of an FFQ in the Henan Rural Cohort Study. Public Health Nutr 23(1):34–40. https://doi.org/10.1017/s1368980019002416
Yang X (2004) China food composition table 2004. Peking University Medical Press, Beijing
Dong X, Li Y, Yang K, Zhang L, Xue Y, Yu S, Liu X, Tu R, Qiao D, Luo Z, Liu X, Wang Y, Li W, Wang C (2021) Associations of spicy food flavor and intake frequency with blood lipid levels and risk of abnormal serum lipid levels in Chinese rural population: a cross-sectional study. Public Health Nutr 1–36. https://doi.org/10.1017/s1368980021001853
Xue Y, Liu C, Wang B, Mao Z, Yu S, Wang Y, Zhang D, Wang C, Li W, Li X (2021) The association between dietary patterns with type 2 diabetes mellitus and pre-diabetes in the Henan rural cohort study. Public Health Nutr 1–10. https://doi.org/10.1017/s1368980021000227
Fan M, Lyu J, He P (2014) Chinese guidelines for data processing and analysis concerning the International physical activity questionnaire. Chinese J Epidemiol 35(8):961–964
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53(6):982–992. https://doi.org/10.1053/j.ajkd.2008.12.034
Dong X, Li Y, Yang K, Zhang L, Xue Y, Yu S, Liu X, Tu R, Qiao D, Luo Z, Liu X, Wang Y, Li W, Zheng Z, Wang C (2020) Mediation effect of body mass index on the association between spicy food intake and hyperuricemia in rural Chinese adults: the Henan rural cohort study. BMC Public Health 20(1):1629. https://doi.org/10.1186/s12889-020-09736-9
Liu X, Jiang J, Liu X, Luo Z, Wang Y, Dong X, Wei D, Li R, Wang Y, Huo W, Yu S, Li L, Jin S, Wang C, Mao Z (2019) Association of serum testosterone with different classes of glucose metabolism and the mediation effect of obesity: the Henan Rural Cohort Study. Diabetes Metab Res Rev 35(5):e3133. https://doi.org/10.1002/dmrr.3133
Kim HJ, Oh SY, Choi DW, Park EC (2019) The association between eating-out rate and BMI in Korea. Int J Environ Res Public Health 16(17):3186. https://doi.org/10.3390/ijerph16173186
Ali N, Perveen R, Rahman S, Mahmood S, Rahman S, Islam S, Haque T, Sumon AH, Kathak RR, Molla NH, Islam F, Mohanto NC, Nurunnabi SM, Ahmed S, Rahman M (2018) Prevalence of hyperuricemia and the relationship between serum uric acid and obesity: a study on Bangladeshi adults. PLoS ONE 13(11):e0206850. https://doi.org/10.1371/journal.pone.0206850
Guthrie JF, Lin BH, Frazao E (2002) Role of food prepared away from home in the American diet, 1977–78 versus 1994–96: changes and consequences. J Nutr Educ Behav 34(3):140–150. https://doi.org/10.1016/s1499-4046(06)60083-3
An R (2016) Fast-food and full-service restaurant consumption and daily energy and nutrient intakes in US adults. Eur J Clin Nutr 70(1):97–103. https://doi.org/10.1038/ejcn.2015.104
Choi MK, Lee YK, Heo YR, Hyun T, Lyu ES, Park H, Ro HK, Bae YJ (2019) Association between the frequency of dining out and the risk of obesity, diabetes mellitus, and dyslipidemia among Korean adults. Ecol Food Nutr 58(6):560–574. https://doi.org/10.1080/03670244.2019.1644327
Forman JP, Scheven L, de Jong PE, Bakker SJ, Curhan GC, Gansevoort RT (2012) Association between sodium intake and change in uric acid, urine albumin excretion, and the risk of developing hypertension. Circulation 125(25):3108–3116. https://doi.org/10.1161/circulationaha.112.096115
Li R, Yu K, Li C (2018) Dietary factors and risk of gout and hyperuricemia: a meta-analysis and systematic review. Asia Pac J Clin Nutr 27(6):1344–1356. https://doi.org/10.6133/apjcn.201811_27(6).0022
Bae J, Shin DH, Chun BY, Choi BY, Kim MK, Shin MH, Lee YH, Park PS, Kim SK (2014) The effect of vitamin C intake on the risk of hyperuricemia and serum uric acid level in Korean Multi-Rural Communities Cohort. Joint Bone Spine 81(6):513–519. https://doi.org/10.1016/j.jbspin.2014.05.007
Rai SK, Fung TT, Lu N, Keller SF, Curhan GC, Choi HK (2017) The dietary approaches to stop hypertension (DASH) diet, Western diet, and risk of gout in men: prospective cohort study. BMJ 357:j1794. https://doi.org/10.1136/bmj.j1794
Vangay P, Johnson AJ, Ward TL, Al-Ghalith GA, Shields-Cutler RR, Hillmann BM, Lucas SK, Beura LK, Thompson EA, Till LM, Batres R, Paw B, Pergament SL, Saenyakul P, Xiong M, Kim AD, Kim G, Masopust D, Martens EC, Angkurawaranon C, McGready R, Kashyap PC, Culhane-Pera KA, Knights D (2018) US immigration westernizes the human gut microbiome. Cell 175(4):962-972.e910. https://doi.org/10.1016/j.cell.2018.10.029
Cohen DA, Story M (2014) Mitigating the health risks of dining out: the need for standardized portion sizes in restaurants. Am J Public Health 104(4):586–590. https://doi.org/10.2105/ajph.2013.301692
Steenhuis IH, Vermeer WM (2009) Portion size: review and framework for interventions. Int J Behav Nutr Phys Act 6:58. https://doi.org/10.1186/1479-5868-6-58
Jee YH, Jung KJ, Park YB, Spiller W, Jee SH (2019) Causal effect of alcohol consumption on hyperuricemia using a Mendelian randomization design. Int J Rheum Dis 22(10):1912–1919. https://doi.org/10.1111/1756-185x.13668
Siqueira JH, Mill JG, Velasquez-Melendez G, Moreira AD, Barreto SM, Benseñor IM, Molina M (2018) Sugar-sweetened soft drinks and fructose consumption are associated with hyperuricemia: cross-sectional analysis from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Nutrients 10(8):981. https://doi.org/10.3390/nu10080981
Bae J, Chun BY, Park PS, Choi BY, Kim MK, Shin MH, Lee YH, Shin DH, Kim SK (2014) Higher consumption of sugar-sweetened soft drinks increases the risk of hyperuricemia in Korean population: the Korean Multi-Rural Communities Cohort Study. Semin Arthritis Rheum 43(5):654–661. https://doi.org/10.1016/j.semarthrit.2013.10.008
Wang DD, Sievenpiper JL, de Souza RJ, Chiavaroli L, Ha V, Cozma AI, Mirrahimi A, Yu ME, Carleton AJ, Di Buono M, Jenkins AL, Leiter LA, Wolever TM, Beyene J, Kendall CW, Jenkins DJ (2012) The effects of fructose intake on serum uric acid vary among controlled dietary trials. J Nutr 142(5):916–923. https://doi.org/10.3945/jn.111.151951
Cicero AFG, Fogacci F, Grandi E, Rizzoli E, Bove M, D’Addato S, Borghi C (2020) Prevalent seasoning and cooking fats, arterial stiffness and blood lipid pattern in a rural population sample: data from the Brisighella Heart Study. Nutrients 12(10):3063. https://doi.org/10.3390/nu12103063
Shao JH, Shen HB, Mo BQ, Xu YC (2004) A community-based case-control study on risk factors of hyperuricemia among residents in the community. Chinese J Epidemiol 25(8):688–690
Kolz M, Johnson T, Sanna S et al (2009) Meta-analysis of 28,141 individuals identifies common variants within five new loci that influence uric acid concentrations. PLoS Genet 5(6):e1000504. https://doi.org/10.1371/journal.pgen.1000504
Nishida Y, Akaoka I, Nishizawa T (1975) Effect of sex hormones on uric acid metabolism in rats. Experientia 31(10):1134–1135. https://doi.org/10.1007/bf02326752
Adamopoulos D, Vlassopoulos C, Seitanides B, Contoyiannis P, Vassilopoulos P (1977) The relationship of sex steroids to uric acid levels in plasma and urine. Acta Endocrinol (Copenh) 85(1):198–208. https://doi.org/10.1530/acta.0.0850198
Leri M, Scuto M, Ontario ML, Calabrese V, Calabrese EJ, Bucciantini M, Stefani M (2020) Healthy effects of plant polyphenols: molecular mechanisms. Int J Mol Sci 21(4):1250. https://doi.org/10.3390/ijms21041250
Dong X, Liu X, Zhang L, Li R, Tu R, Hou J, Mao Z, Huo W, Guo Y, Li S, Chen G, Wang C (2021) Residential greenness associated with lower serum uric acid levels and hyperuricemia prevalence in a large Chinese rural population. Sci Total Environ 770:145300. https://doi.org/10.1016/j.scitotenv.2021.145300
Tang YX, Bloom MS, Qian ZM, Liu E, Jansson DR, Vaughn MG, Lin HL, Xiao LW, Duan CW, Yang L, Xu XY, Li YR, Zhu L, Dong GH, Liu YM (2021) Association between ambient air pollution and hyperuricemia in traffic police officers in China: a cohort study. Int J Environ Health Res 31(1):54–62. https://doi.org/10.1080/09603123.2019.1628926
Acknowledgements
Thanks to all participants, researchers, and hospital staff devoted to the Henan Rural Cohort Study for their enthusiastic collaboration. The authors are grateful to all coordinators and reviewers for technical assistance and helpful suggestions in the preparation of this manuscript.
Funding
This research was supported by the Foundation of National Key Program of Research and Development of China (Grant No: 2016YFC0900803), National Natural Science Foundation of China (Grant No: 81573243, 81602925), Henan Provincial Science Fund for Distinguished Young Scholars (Grant No: 164100510021), Science and Technology Innovation Talents Support Plan of Henan Province Colleges and Universities (Grant No: 14HASTIT035), Discipline Key Research and Development Program of Zhengzhou University (Grant No: XKZDQY202008, XKZDQY202002). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
YQL and CJW conceived and designed the study. XKD, WL, YX, XTL, XL, HJ, WQH, LLL and ZXM coordinated data collection. NNC and XKD conducted the analyses and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest.
Ethics approval
The study was conducted by the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the Zhengzhou University Medical Life Science Committee (Ethic approval code: [2015] MEC (S128)).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cui, N., Dong, X., Liao, W. et al. Association of eating out frequency and other factors with serum uric acid levels and hyperuricemia in Chinese population. Eur J Nutr 61, 243–254 (2022). https://doi.org/10.1007/s00394-021-02634-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02634-9