Abstract
Introduction
Our aim was to determine the incidence of diverticulitis recurrence after sigmoid colectomy for diverticular disease.
Methods
Consecutive patients who benefited from sigmoid colectomy for diverticular disease from January 2007 to June 2021 were identified based on operative codes. Recurrent episodes were identified based on hospitalization codes and reviewed. Survival analysis was performed and was reported using a Kaplan–Meier curve. Follow-up was censored for last hospital visit and diverticulitis recurrence. The systematic review of the literature was performed according to the PRISMA statement. Medline, Embase, CENTRAL, and Web of Science were searched for studies reporting on the incidence of diverticulitis after sigmoid colectomy. The review was registered into PROSPERO (CRD42021237003, 25/06/2021).
Results
One thousand three-hundred and fifty-six patients benefited from sigmoid colectomy. Four hundred and three were excluded, leaving 953 patients for inclusion. The mean age at time of sigmoid colectomy was 64.0 + / − 14.7 years. Four hundred and fifty-eight patients (48.1%) were males. Six hundred and twenty-two sigmoid colectomies (65.3%) were performed in the elective setting and 331 (34.7%) as emergency surgery. The mean duration of follow-up was 4.8 + / − 4.1 years. During this period, 10 patients (1.1%) developed reccurent diverticulitis. Nine of these episodes were classified as Hinchey 1a, and one as Hinchey 1b. The incidence of diverticulitis recurrence (95% CI) was as follows: at 1 year: 0.37% (0.12–1.13%), at 5 years: 1.07% (0.50–2.28%), at 10 years: 2.14% (1.07–4.25%) and at 15 years: 2.14% (1.07–4.25%). Risk factors for recurrence could not be assessed by logistic regression due to the low number of incidental cases. The systematic review of the literature identified 15 observational studies reporting on the incidence of diverticulitis recurrence after sigmoid colectomy, which ranged from 0 to 15% for a follow-up period ranging between 2 months and over 10 years.
Conclusion
The incidence of diverticulitis recurrence after sigmoid colectomy is of 2.14% at 15 years, and is mostly composed of Hinchey 1a episodes. The incidences reported in the literature are heterogeneous.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colonic diverticulosis defines the presence of diverticula, which are mucosal protrusion through the muscularis propria of the colon. They are preferentially located in the left colon and the sigmoid colon [1]. The prevalence of diverticulosis was estimated to be as high as at 42% in an American population aged 30 to 80 years [1]. Various risk factors have been identified for the development of diverticulosis, including age, ethnicity, overweight, smoking, as well as slowed bowel movement [2]. Colonic diverticulosis remains asymptomatic in a majority of patients. However, approximately 15–20% of patients develop a complication related to diverticulosis, such as acute diverticulitis, lower gastrointestinal bleeding, colonic obstruction or chronic pain [3]. Among these complications, acute diverticulitis is the most common and affect 4–15% of patients suffering from diverticulosis during their lifetime [4]. Diverticulitis leads to significant morbidity and mortality (mortality estimated to be of 2.5 per 100,000, [5]), and represents 2.6 billion dollars per year in the USA [5].
Acute diverticulitis has been stratified by several scoring systems according to its severity [6]. The severity of the episode usually dictates its management, from medical treatment with or without antibiotics [7], to percutaneous computed tomography-guided drainage, laparoscopic lavage or Hartmann intervention [8]. In case of non-surgical management, elective sigmoid colectomy can be later performed for patients with reduced quality of life due to diverticular disease or suffering from a chronic complication of diverticular disease (such as stenosis or fistula). Moreover, emergency surgery is indicated in the event of Hinchey III or Hinchey IV diverticulitis [8]. However, sigmoid colectomy does not necessarily remove the entirety of the colon affected by diverticula. Therefore, recurrence of diverticulitis may occur after sigmoid colectomy.
Considering the importance of estimating the risk of recurrence for optimal decision making and patients’ information, we aimed at determining the incidence of recurrent diverticulitis after sigmoid colectomy.
Materials and methods
Original study
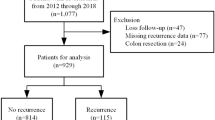
In this monocenter cohort study performed in a tertiary center, consecutive patients who benefited from sigmoid colectomy for diverticular disease from January 2007 to June 2021 were retrospectively identified based on operative codes. Operative reports were reviewed, and patients who benefited of sigmoid colectomy for any other indication than diverticular disease, such as cancer, were excluded. Noteworthy, indications for sigmoid colectomy for diverticular disease in our center include recurrent/chronic diverticulitis impairing quality of life and diverticular stenosis in the elective setting, and Hinchey III and Hinchey IV diverticulitis, Hinchey 1b diverticulitis not responding to non-surgical management, and diverticular bleeding not responding to endoscopic management in the emergency setting. The surgical procedure for sigmoid colectomy was performed by laparoscopy in first intent, and removed the recto-sigmoid junction. If a colorectal anastomosis was performed, the surgical procedure included mobilization of the splenic flexure to provide a tension-free anastomosis. Recurrent episodes were identified based on hospitalization codes (related to diverticulitis) and manually reviewed. A recurrent episode was defined as an episode of acute diverticulitis proven by computed tomography following sigmoid colectomy. Demographic variables at time of surgery and para-clinical variables (blood, computed tomography) at time of recurrence were collected. Survival analysis was performed and was reported using a Kaplan–Meier curve. Follow-up was censored for the last hospital visit and date of diverticulitis recurrence.
Systematic review
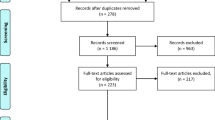
The systematic review of the literature was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [9] (Table S1). Medline, Embase, CENTRAL, and Web of Science were searched from inception to the 28.10.20 for studies reporting on the incidence of recurrent diverticulitis after sigmoid colectomy. The literature search strategy is reported in Table S2. Non-primary research articles (editorials, reviews, secondary analyses), duplicates, non-English literature, and studies that did not report the incidence of postoperative recurrent diverticulitis were excluded. Abstracts were considered. Two independent reviewers (AW, JM) performed the screening of eligible articles and the data extraction, using Covidence (Veritas Health Innovation, Melbourne, Australia). In case of disagreement, consensus was reached with a third reviewer (AB). Characteristics of included studies were extracted from included studies. A qualitative analysis was performed. The review was registered into the international prospective register of systematic reviews PROSPERO [10] (registration number CDR42021237003).
Results
Cohort study
Inclusion process
One thousand three hundred and fifty-six patients underwent sigmoid colectomy over the study period. Among them, 403 patients benefited from sigmoid colectomy for other indications than diverticular disease and were excluded from further analysis, leaving 953 patients for inclusion (Fig. S1).
Demographics of included patients
The mean age at time of sigmoid colectomy was 64.0 + / − 14.7 years. Four hundred and fifty-eight patients (48.1%) were males. Six-hundred and twenty-two sigmoid colectomies (65.3%) were performed in the elective setting and 331 (34.7%) as emergency surgery.
Incidence of diverticulitis recurrence after sigmoid colectomy
The mean duration of follow-up was 4.8 + / − 4.1 years. During this time period, 10 patients (1.1%) developed diverticulitis recurrence. Their mean age was 60.6 + / − 20.2 years. Six patients were females (60%) and four were males (40%). The mean white blood cells count at time of re-admission was of 11.4 + / − 8.5 G/L, and the mean C Reactiv Protein concentration was of 59.4 + / − 44.1 g/L. Five recurrent episodes were localized on the left colon above the anastomosis (colonic conduit), 3 on the right colon and 2 on the transverse colon. Nine of the recurrent episodes were classified by computed tomography as Hinchey 1a, and one was staged as Hinchey 1b (Table 1). All recurrent diverticulitis episodes were managed with antibiotics. Therefore, according to survival analysis, the incidence of recurrent diverticulitis (95% CI) was as follows: at 1 year: 0.37% (0.12–1.13%), at 5 years: 1.07% (0.50–2.28%), at 10 years: 2.14% (1.07–4.25%) and at 15 years: 2.14% (1.07–4.25%) (Fig. S2).
Systematic review of the literature
Inclusion process
Two hundred ninety-three publications were identified from database screening. Twenty duplicates were removed. Of the 273 publications remaining, 254 were excluded after title and abstract screening and five after full text screening, leaving 14 studies for inclusion (Fig. 1).
Characteristics of included studies
Included studies totalized 4489 patients who underwent sigmoid colectomy for diverticulitis. The number of patients per study ranged between 8 [11] and 12,073 [12]. Studies were published between 2003 and 2019: two in 2003 [13, 14], one in 2004 [15], one in 2005 [16], one in 2008 [17], one in 2009 [18], one in 2011 [19], one in 2012 [20], one in 2014 [21], one in 2015 [22], one in 2016 [11], one in 2018 [23], and two in 2019 [12, 24]. Five studies were produced in the USA [12-14, 18, 24], two in France [14, 21], two in Germany [15, 19], two in Italy [20, 22], one in the UK [23], one in the Netherlands [17], one in Belgium [16], and one in Saudi Arabia [11]. The studies included 1 randomized clinical trial [23], 8 retrospective studies [12, 13, 18, 20, 22, 2416-], 4 prospective studies [11, 15, 19, 20], and 2 case-control studies [14, 21]. Ten studies included complicated episodes of diverticulitis (11, 20, 2415-22-] and ten studies included uncomplicated episodes of diverticulitis [12-14, 22, 2417-]. Six studies refer to elective settings [12, 13, 16, 17, 22, 24] versus three emergency settings [17, 19, 20]. Two studies [13, 14] partly include patients from a similar cohort. Detailed characteristics of included studies are reported in Table 2.
Incidence of diverticulitis recurrence reported by included studies
Incidence rates varied between 0 and 15% [12] for follow-up times ranging from 2 months [15] to 12 years [20]. The highest incidence was 15% over a 5-year follow-up [12]. Of 4489 pooled patients who underwent surgery and 415 had at least one episode of postoperative diverticulitis (9.2%). Recurrence was either based on clinical presentation [12], computed tomography, endoscopy, or a combination of the above [13, 14, 18, 19, 24]. The delay period required to distinguish recurrence from the previous episode varies between authors: 30 days after full recovery [19] versus 6 weeks [12].
Discussion
According to our cohort, the incidence of diverticulitis recurrence after sigmoid colectomy for diverticular disease is of 2.14% at 15 years. These recurrences are mostly composed of uncomplicated Hinchey 1a episodes (modified classification).
The incidence of recurrence found in our population was rather low, especially when compared to the literature. For instance, one small cohort study estimated this incidence to be of 8.7% after 12 years [17]. However, this cohort was of a smaller sample size (183 patients), and diagnosis of recurrence was performed using a combination of clinical, laboratory criteria associated with compatible imaging, constituted of CT but also barium enema or colonoscopy. Therefore, the wider criteria used for diagnosing recurrence may explain the difference with our findings. Similarly, two other studies based on smaller cohorts and whose diagnostic imaging was either CT or barium enema recorded a higher incidence, respectively 5% after 6.5 years in a cohort of 236 patients [13] and 14% after 5 years in a cohort of 158 patients [14]. A larger cohort study, including 12,073 patients, of which 2241 were treated surgically, estimated the incidence of recurrence to be of 15% after 5 years for the surgical group [12]. The population included patients who received medical or surgical management (as inpatients or outpatients) for a second, third, fourth, or fifth episode of uncomplicated diverticulitis. Recurrence of diverticulitis was defined as any consultation for treatment of diverticulitis occurring more than 6 weeks after the episode; the exact diagnostic method is not mentioned. The heterogeneity in the definitions of recurrence may explain the higher incidence of recurrence than in our study. It has indeed been shown that adding an imaging method such as ultrasound or CT to the diagnosis increased the negative predictive value of diverticulitis from 0.98 to 0.99 and the positive predictive value from 0.65 to 0.95 [25]. One study showed an incidence of recurrence of 4.2% at 55 months confirmed clinically and by CT-scan [24]. However, the data were collected using emails or telephone questionnaires, which again raises the question of the exact definition of recurrence. In addition, the type of setting seems to influence the reported incidence of recurrence as shown in two studies where surgery occurred in an emergency setting for acute diverticulitis. Indeed, in these studies, the incidence of recurrence was 3.5% for a follow-up of 2.6 years [19] and 5.8% for a follow-up of 10.6 years [20]. Similarly, the surgical approach appears to influence the risk of recurrence as reported in a case–control study (2.7% recurrence in the laparoscopy group versus 9.6% for open colon resection) [21]. However, the follow-up was significantly longer in the open colon resection group (63 months) than in the laparoscopy group (46 months), which makes it difficult to draw final conclusions. The absence of diverticulitis recurrence in some studies may be explained by either the size of the cohort or the length of the follow-up [11, 15, 16, 22]. Moreover, an information bias is also possible. One randomized clinical trial recorded an incidence of recurrence of 8% [23]. However, the cohort only included patients with complicated diverticulitis. These higher incidences highlight the role of the indication as risk factor of recurrence. Nonetheless, the current literature does not support that a complicated presentation increases the risk of recurrence of diverticulitis. On the contrary, uncomplicated recurrent diverticulitis has been suggested as a likely risk factor for recurrence (the link is not established by multiple logistic regression analysis) [24]. The length of colon resection is also a postulated risk factor for recurrence. Several studies have examined this question, without finding a unanimous answer. Two case–control studies [13, 21] maintain that the level of anastomosis influences the risk of recurrence of diverticulitis after sigmoidectomy and one study [20] contradicts this hypothesis. Additionally, age and persistent postoperative pain are two risk factors of recurrence mentioned in the literature [17].
In comparison, a systematic review describes the following risk factors for recurrence of diverticulitis after non-surgical treatment. Firstly, non-modifiable factors such as young age and female gender are considered risk factors for recurrence. Secondly, it has been shown that a primary episode of acute diverticulitis with abscess formation is associated with an increased risk of recurrence, compared to uncomplicated diverticulitis. Furthermore, the size of the inflamed segment as well as the number and colonic extension of the diverticula increases the risk of recurrence. The number of previous recurrence episodes and the interval with a previous episode also plays a role. Indeed, the risk is higher in the first year after remission [26].
By comparing the risk factors for recurrence in patients treated non-surgically versus surgically, it appears that thorough selection of patients for surgical management may decrease the incidence of recurrence. Indeed, prioritizing complicated manifestations for surgery should theoretically decrease the number of recurrences of diverticulitis after sigmoidectomy. Furthermore, as the size of the inflamed segment determines the risk of recurrence in the non-surgically treated group and the level of anastomosis in the surgical group is still debated, it will be interesting to follow the literature in the future to draw conclusions.
The strengths of our study are a cohort including all stages of diverticulitis and easy access to patient follow-up data. Indeed, our center is the only public tertiary center in the region; all patients with public insurance who were operated in our center are therefore re-hospitalized in our center in case of recurrence, and the computerized system allowed us to extract follow-up data over a long period. Moreover, the review includes searches were conducted on several databases with a wide range of literature. However, it remains possible that a few patients may be treated as outpatients by their general practitioners, and may not be identified by our search in case of a recurrence. The additional limitations of our study are the absence of quality-of-life measurement after sigmoid colectomy, the fact that a few patients may have undergone sigmoid colectomy for other diverticular disease-related diagnoses, such as bleeding diverticula, and the retrospective design of the study, which limited data collection. Moreover, considering the small number of incident cases, we could not identify predictors of recurrence by logistic regression. Nevertheless, our systematic review managed to identify the following risk factors, which were consistent with a systematic review of the risk of recurrence of diverticulitis after surgery [27]: age, persistent postoperative pain (which may be a postoperative complication and not a recurrent episode), uncomplicated recurrent diverticulitis as an operative indication, preoperative diagnosis of irritable bowel syndrome, pathology result incompatible with acute diverticulitis and patient’s comorbidities. In addition, the small sample size of these studies does not allow adequate identification of risk factors by regression, and the retrospective design of these studies does not allow adequate follow-up of patients to identify possible recurrences.
Conclusion
The risk of recurrence of diverticulitis after sigmoid colectomy is low and recurrent episodes are mostly uncomplicated. Sigmoid colectomy is therefore a good treatment option for diverticulitis. However, the indication must be weighed against the risk factors for recurrence, which should influence the proposed management.
Data availability
Data are available upon reasonable request.
References
Peery AF, Keku TO, Martin CF, Eluri S, Runge T, Galanko JA et al (2016) Distribution and characteristics of colonic diverticula in a United States screening population. Clin Gastroenterol Hepatol 14(7):980-985.e1
Strate LL, Morris AM (2019) Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology 156(5):1282-1298.e1
Tursi A, Papa A, Danese S (2015) Review article: the pathophysiology and medical management of diverticulosis and diverticular disease of the colon. Aliment Pharmacol Ther 42(6):664–684
Imaeda H, Hibi T (2018) The burden of diverticular disease and its complications: west versus east. Inflamm Intest Dis 3(2):61–68
Sandler RS, Everhart JE, Donowitz M, Adams E, Cronin K, Goodman C et al (2002) The burden of selected digestive diseases in the United States. Gastroenterology 122(5):1500–1511
Klarenbeek B, de Korte N, Peet D, Cuesta M (2011) Review of current classifications for diverticular disease and a translation into clinical practice. Int J Colorectal Dis 17(27):207–214
van Dijk ST, Chabok A, Dijkgraaf MG, Boermeester MA, Smedh K (2020) Observational versus antibiotic treatment for uncomplicated diverticulitis: an individual-patient data meta-analysis. Br J Surg 107(8):1062–1069
Francis NK, Sylla P, Abou-Khalil M, Arolfo S, Berler D, Curtis NJ et al (2019) EAES and SAGES 2018 consensus conference on acute diverticulitis management: evidence-based recommendations for clinical practice. Surg Endosc 33(9):2726–2741
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29(372):n71
Prospero [Internet]. Available from: https://www.crd.york.ac.uk/prospero/
Ghasoup A, Al Qurashi T, Widinly M, Sadieh O, Laparoscopic sigmoidectomy for complicated diverticular disease - SAGES Abstract Archives [Internet]. SAGES. [cited 2022 Feb 13]. Available from: https://www.sages.org/meetings/annual-meeting/abstracts-archive/laparoscopic-sigmoidectomy-for-complicated-diverticular-disease/
Thornblade LW, Simianu VV, Davidson GH, Flum DR (2021) Elective surgery for diverticulitis and the risk of recurrence and ostomy. Ann Surg 273(6):1157–1164
Thaler K, Baig MK, Berho M, Weiss EG, Nogueras JJ, Arnaud JP et al (2003) Determinants of recurrence after sigmoid resection for uncomplicated diverticulitis. Dis Colon Rectum 46(3):385–388
Thaler K, Weiss EG, Nogueras JJ, Arnaud JP, Wexner SD, Bergamaschi R (2003) Recurrence rates at minimum 5-year follow-up: laparoscopic versus open sigmoid resection for uncomplicated diverticulitis. Surg Laparosc Endosc Percutan Tech 13(5):325–327
Schwandner O, Farke S, Fischer F, Eckmann C, Schiedeck THK, Bruch HP (2004) Laparoscopic colectomy for recurrent and complicated diverticulitis: a prospective study of 396 patients. Langenbecks Arch Surg 389(2):97–103
Laurent SR, Detroz B, Detry O, Degauque C, Honoré P, Meurisse M (2005) Laparoscopic sigmoidectomy for fistulized diverticulitis. Dis Colon Rectum 48(1):148–152
Andeweg C, Peters J, Bleichrodt R, van Goor H (2008) Incidence and risk factors of recurrence after surgery for pathology-proven diverticular disease. World J Surg 32(7):1501–1506
Lipof T, Zanno A, Spilka J, Bartus C, Johnson K, Sardella W et al (2009) Long-term outcomes after laparoscopic colectomy in the treatment of sigmoid diverticulitis, Dis Col Rectum 52(4):764–861
Holmer C, Lehmann KS, Engelmann S, Gröne J, Buhr HJ, Ritz JP (2011) Long-term outcome after conservative and surgical treatment of acute sigmoid diverticulitis. Langenbecks Arch Surg 396(6):825–832
Binda GA, Mataloni F, Bruzzone M, Carabotti M, Cirocchi R, Nascimbeni R et al (2018) Trends in hospital admission for acute diverticulitis in Italy from 2008 to 2015. Tech Coloproctol 22(8):597–604
Bergamaschi R, Arnaud JP (1998) Anastomosis level and specimen length in surgery for uncomplicated diverticulitis of the sigmoid. Surg Endosc 12(9):1149–1151
Roscio F, Grillone G, Frattini P, De Luca A, Girardi V, Scandroglio I (2015) Effectiveness of elective laparoscopic treatment for colonic diverticulitis. JSLS 19(2):e2014.00120
You K, Bendl R, Taut C, Sullivan R, Gachabayov M, Bergamaschi R et al (2018) Randomized clinical trial of elective resection versus observation in diverticulitis with extraluminal air or abscess initially managed conservatively. Br J Surg 105(8):971–979
Choi KK, Martinolich J, Canete JJ, Valerian BT, Chismark DA, Ata A et al (2020) Elective laparoscopic sigmoid colectomy for diverticulitis—an updated look at recurrence after surgery. J Gastrointest Surg 24(2):388–395
Toorenvliet BR, Bakker RFR, Breslau PJ, Merkus JWS, Hamming JF (2010) Colonic diverticulitis: a prospective analysis of diagnostic accuracy and clinical decision-making. Colorectal Dis 12(3):179–186
Hupfeld L, Burcharth J, Pommergaard HC, Rosenberg J (2017) Risk factors for recurrence after acute colonic diverticulitis: a systematic review. Int J Colorectal Dis 32(5):611–622
Longchamp G, Abbassi Z, Meyer J, Toso C, Buchs NC, Ris F (2021) Surgical resection does not avoid the risk of diverticulitis recurrence—a systematic review of risk factors. Int J Colorectal Dis 36(2):227–237
Funding
Open access funding provided by University of Geneva
Author information
Authors and Affiliations
Contributions
Alexia Waser and Jeremy Meyer conceived the study. Alexia Waser collected the data. Alexia Waser, Alexandre Balaphas, Isabelle Uhe, Christian Toso, Nicolas Buchs, Frédéric Ris, and Jeremy Meyer analyzed and interpreted the data. Alexia Waser, Alexandre Balaphas, and Jeremy Meyer drafted the manuscript. Alexia Waser, Alexandre Balaphas, Isabelle Uhe, Christian Toso, Nicolas Buchs, Frédéric Ris, and Jeremy Meyer wrote the manuscript and performed critical revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Waser, A., Balaphas, A., Uhe, I. et al. Incidence of diverticulitis recurrence after sigmoid colectomy: a retrospective cohort study from a tertiary center and systematic review. Int J Colorectal Dis 38, 157 (2023). https://doi.org/10.1007/s00384-023-04454-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04454-1