Abstract
Background
The effects of subcutaneous closed-suction Blake drain for preventing incisional surgical site infections (SSIs) after colorectal surgery have never been evaluated in a randomized controlled trial (RCT). Thus, we performed a RCT to evaluate the clinical benefits of using a subcutaneous closed-suction Blake drain in patients undergoing colorectal surgery.
Method
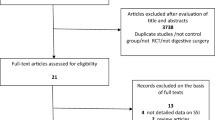
Consecutive patients who underwent colorectal surgery were enrolled in this study. Patients were randomly assigned to the subcutaneous closed-suction drainage arm or the control (no subcutaneous drainage) arm. The primary endpoint was incidence rate of incisional SSIs. And, we performed logistic regression analysis to detect predictive factors for incisional SSIs after colorectal surgery.
Results
From November 2012 to September 2014, a total of 240 patients were enrolled in this study. One-hundred-seventeen patients who were treated by the control arm and 112 patients by the subcutaneous drainage arm were judged to be eligible for analysis. The incidence of incisional SSIs rate was 8.7 % in the overall patients. The incidence of incisional SSIs rate was 12.8 % in the control arm and 4.5 % in the subcutaneous drainage arm. There was significantly reduction of the incidence in the subcutaneous drainage arm than in the control arm (p = 0.025). Logistic regression analysis demonstrated that thickness of subcutaneous fat >3.0 cm, forced expiratory volume in 1 s as percent of forced vital capacity (FEV1.0 %) >70 %, and subcutaneous drain were independent predictors of postoperative incisional SSIs (p = 0.008, p = 0.004, and p = 0.017, respectively).
Conclusion
The results of our RCT suggest that a subcutaneous Blake drain is beneficial for preventing incisional SSIs in patients undergoing colorectal surgery.

Similar content being viewed by others
References
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) hospital infection control practices advisory committee. Am J Infect Control 27(2):97–132
Pinkney TD, Calvert M, Bartlett DC, Gheorghe A, Redman V, Dowswell G, Hawkins W, Mak T, Youssef H, Richardson C, Hornby S, Magill L, Haslop R, Wilson S, Morton D (2013) Impact of wound edge protection devices on surgical site infection after laparotomy: multicentre randomised controlled trial (ROSSINI trial). BMJ 347:f4305. doi:10.1136/bmj.f4305
Mihaljevic AL, Schirren R, Ozer M, Ottl S, Grun S, Michalski CW, Erkan M, Jager C, Reiser-Erkan C, Kehl V, Schuster T, Roder J, Clauer U, Orlitsch C, Hoffmann TF, Lange R, Harzenetter T, Steiner P, Michalski M, Henkel K, Stadler J, Pistorius GA, Jahn A, Obermaier R, Unger R, Strunk R, Willeke F, Vogelsang H, Halve B, Dietl KH, Hilgenstock H, Meyer A, Kramling HJ, Wagner M, Schoenberg MH, Zeller F, Schmidt J, Friess H, Kleeff J (2014) Multicenter double-blinded randomized controlled trial of standard abdominal wound edge protection with surgical dressings versus coverage with a sterile circular polyethylene drape for prevention of surgical site infections: a CHIR-net trial (BaFO; NCT01181206). Ann Surg 260(5):730–737 . doi:10.1097/SLA.0000000000000954discussion 737-739
Panici PB, Zullo MA, Casalino B, Angioli R, Muzii L (2003) Subcutaneous drainage versus no drainage after minilaparotomy in gynecologic benign conditions: a randomized study. Am J Obstet Gynecol 188(1):71–75
Colli A, Camara ML (2011) First experience with a new negative pressure incision management system on surgical incisions after cardiac surgery in high risk patients. J Cardiothorac Surg 6:160. doi:10.1186/1749-8090-6-160
Baier PK, Gluck NC, Baumgartner U, Adam U, Fischer A, Hopt UT (2010) Subcutaneous Redon drains do not reduce the incidence of surgical site infections after laparotomy. A randomized controlled trial on 200 patients. Int J Color Dis 25(5):639–643. doi:10.1007/s00384-010-0884-y
Kaya E, Paksoy E, Ozturk E, Sigirli D, Bilgel H (2010) Subcutaneous closed-suction drainage does not affect surgical site infection rate following elective abdominal operations: a prospective randomized clinical trial. Acta Chir Belg 110(4):457–462
Mori T, Kimura T, Kitajima M (2010) Skill accreditation system for laparoscopic gastroenterologic surgeons in Japan. Minimally invasive therapy & allied technologies : MITAT : official journal of the Society for Minimally Invasive Therapy 19(1):18–23. doi:10.3109/13645700903492969
Al-Inany H, Youssef G, Abd ElMaguid A, Abdel Hamid M, Naguib A (2002) Value of subcutaneous drainage system in obese females undergoing cesarean section using Pfannenstiel incision. Gynecol Obstet Investig 53(2):75–78
Magann EF, Chauhan SP, Rodts-Palenik S, Bufkin L, Martin JN Jr, Morrison JC (2002) Subcutaneous stitch closure versus subcutaneous drain to prevent wound disruption after cesarean delivery: a randomized clinical trial. Am J Obstet Gynecol 186(6):1119–1123
Chowdri NA, Qadri SA, Parray FQ, Gagloo MA (2007) Role of subcutaneous drains in obese patients undergoing elective cholecystectomy: a cohort study. Int J Surg 5(6):404–407. doi:10.1016/j.ijsu.2007.05.011
Hellums EK, Lin MG, Ramsey PS (2007) Prophylactic subcutaneous drainage for prevention of wound complications after cesarean delivery—a metaanalysis. Am J Obstet Gynecol 197(3):229–235. doi:10.1016/j.ajog.2007.05.023
Fujii T, Tabe Y, Yajima R, Yamaguchi S, Tsutsumi S, Asao T, Kuwano H (2011) Effects of subcutaneous drain for the prevention of incisional SSI in high-risk patients undergoing colorectal surgery. Int J Color Dis 26(9):1151–1155. doi:10.1007/s00384-011-1228-2
Tsujita E, Yamashita Y, Takeishi K, Matsuyama A, Tsutsui S, Matsuda H, Taketomi A, Shirabe K, Ishida T, Maehara Y (2012) Subcuticular absorbable suture with subcutaneous drainage system prevents incisional SSI after hepatectomy for hepatocellular carcinoma. World J Surg 36(7):1651–1656. doi:10.1007/s00268-012-1524-1
Pan HD, Wang L, Peng YF, Li M, Yao YF, Zhao J, Zhan TC, Du CZ, Gu J (2015) Subcutaneous vacuum drains reduce surgical site infection after primary closure of defunctioning ileostomy. Int J Color Dis 30(7):977–982. doi:10.1007/s00384-015-2168-z
Braakenburg A, Obdeijn MC, Feitz R, van Rooij IA, van Griethuysen AJ, Klinkenbijl JH (2006) The clinical efficacy and cost effectiveness of the vacuum-assisted closure technique in the management of acute and chronic wounds: a randomized controlled trial. Plast Reconstr Surg 118(2):390–397 . doi:10.1097/01.prs.0000227675.63744.afDiscussion 398-400
Borgquist O, Ingemansson R, Malmsjo M (2010) Wound edge microvascular blood flow during negative-pressure wound therapy: examining the effects of pressures from −10 to −175 mmHg. Plast Reconstr Surg 125(2):502–509. doi:10.1097/PRS.0b013e3181c82e1f
Nakayama H, Takayama T, Okubo T, Higaki T, Midorikawa Y, Moriguchi M, Aramaki O, Yamazaki S (2014) Subcutaneous drainage to prevent wound infection in liver resection: a randomized controlled trial. J Hepato-biliary-pancreat Sci 21(7):509–517. doi:10.1002/jhbp.93
Atkins BZ, Wooten MK, Kistler J, Hurley K, Hughes GC, Wolfe WG (2009) Does negative pressure wound therapy have a role in preventing poststernotomy wound complications? Surg Innov 16(2):140–146. doi:10.1177/1553350609334821
Stannard JP, Atkins BZ, O’Malley D, Singh H, Bernstein B, Fahey M, Masden D, Attinger CE (2009) Use of negative pressure therapy on closed surgical incisions: a case series. Ostomy/Wound Manag 55(8):58–66
Chadi SA, Kidane B, Britto K, Brackstone M, Ott MC (2014) Incisional negative pressure wound therapy decreases the frequency of postoperative perineal surgical site infections: a cohort study. Dis Colon rectum 57(8):999–1006. doi:10.1097/DCR.0000000000000161
Ramsey PS, White AM, Guinn DA, Lu GC, Ramin SM, Davies JK, Neely CL, Newby C, Fonseca L, Case AS, Kaslow RA, Kirby RS, Rouse DJ, Hauth JC (2005) Subcutaneous tissue reapproximation, alone or in combination with drain, in obese women undergoing cesarean delivery. Obstet Gynecol 105(5 Pt 1):967–973. doi:10.1097/01.AOG.0000158866.68311.d1
Imada S, Noura S, Ohue M, Shingai T, Sueda T, Kishi K, Yamada T, Ohigashi H, Yano M, Ishikawa O (2013) Efficacy of subcutaneous penrose drains for surgical site infections in colorectal surgery. World J Gastrointest Surg 5(4):110–114. doi:10.4240/wjgs.v5.i4.110
Bamgbade OA, Rutter TW, Nafiu OO, Dorje P (2007) Postoperative complications in obese and nonobese patients. World J Surg 31(3):556–560 . doi:10.1007/s00268-006-0305-0discussion 561
Fujii T, Tsutsumi S, Matsumoto A, Fukasawa T, Tabe Y, Yajima R, Asao T, Kuwano H (2010) Thickness of subcutaneous fat as a strong risk factor for wound infections in elective colorectal surgery: impact of prediction using preoperative CT. Dig Surg 27(4):331–335. doi:10.1159/000297521
Lee JS, Terjimanian MN, Tishberg LM, Alawieh AZ, Harbaugh CM, Sheetz KH, Holcombe SA, Wang SC, Sonnenday CJ, Englesbe MJ (2011) Surgical site infection and analytic morphometric assessment of body composition in patients undergoing midline laparotomy. J Am Coll Surg 213(2):236–244. doi:10.1016/j.jamcollsurg.2011.04.008
Segal CG, Waller DK, Tilley B, Piller L, Bilimoria K (2014) An evaluation of differences in risk factors for individual types of surgical site infections after colon surgery. Surgery 156(5):1253–1260. doi:10.1016/j.surg.2014.05.010
Moghadamyeghaneh Z, Hanna MH, Carmichael JC, Mills S, Pigazzi A, Nguyen NT, Stamos MJ (2015) Wound disruption following colorectal operations. World J Surg 39(12):2999–3007. doi:10.1007/s00268-015-3208-0
Thomsen T, Tonnesen H, Moller AM (2009) Effect of preoperative smoking cessation interventions on postoperative complications and smoking cessation. The British journal of surgery 96(5):451–461. doi:10.1002/bjs.6591
Hawn MT, Houston TK, Campagna EJ, Graham LA, Singh J, Bishop M, Henderson WG (2011) The attributable risk of smoking on surgical complications. Ann Surg 254(6):914–920. doi:10.1097/SLA.0b013e31822d7f81
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jun Watanabe, Mitsuyoshi Ota, Yusuke Suwa, Atsushi Ishibe, Kazuteru Watanabe, Hidenobu Masui, Kaoru Nagahori, and Itaru Endo have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Watanabe, J., Ota, M., Kawamoto, M. et al. A randomized controlled trial of subcutaneous closed-suction Blake drains for the prevention of incisional surgical site infection after colorectal surgery. Int J Colorectal Dis 32, 391–398 (2017). https://doi.org/10.1007/s00384-016-2687-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-016-2687-2