Abstract
Objectives
Postoperative wound disruption is associated with high morbidity and mortality. We sought to identify the risk factors and outcomes of wound disruption following colorectal resection.
Methods
The American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database was used to examine the clinical data of patients who underwent colorectal resection from 2005 to 2013. Multivariate regression analysis was performed to identify risk factors of wound disruption.
Results
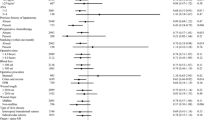
We sampled a total of 164,297 patients who underwent colorectal resection. Of these, 2073 (1.3 %) had wound disruption. Patients with wound disruption had significantly higher mortality (5.1 vs. 1.9 %, AOR: 1.46, P = 0.01). The highest risk of wound disruption was seen in patients with wound infection (4.8 vs. 0.9 %, AOR: 4.11, P < 0.01). A number of factors are associated with wound disruption such as chronic steroid use (AOR: 1.71, P < 0.01), smoking (AOR: 1.60, P < 0.01), obesity (AOR: 1.57, P < 0.01), operation length more than 3 h (AOR: 1.56, P < 0.01), severe Chronic Obstructive Pulmonary Disease (COPD) (AOR: 1.36, P < 0.01), urgent/emergent admission (AOR: 1.31, P = 0.01), and serum Albumin Level <3 g/dL (AOR: 1.27, P < 0.01). Laparoscopic surgery had significantly lower risk of wound disruption compared to open surgery (AOR: 0.61, P < 0.01).
Conclusion
Wound disruption occurs in 1.3 % of colorectal resections, and it correlates with mortality of patients. Wound infection is the strongest predictor of wound disruption. Chronic steroid use, obesity, severe COPD, prolonged operation, non-elective admission, and serum albumin level are strongly associated with wound disruption. Utilization of the laparoscopic approach may decrease the risk of wound disruption when possible.


Similar content being viewed by others
References
Cöl C, Soran A, Cöl M (1998) Can postoperative abdominal wound dehiscence be predicted? Tokai J Exp Clin Med 23:123–127
Khorgami Z, Shoar S, Laghaie B, Aminian A, Hosseini Araghi N, Soroush A (2013) Prophylactic retention sutures in midline laparotomy in high-risk patients for wound dehiscence: a randomized controlled trial. J Surg Res 180:238–243
Hahler B (2006) Surgical wound dehiscence. Medsurg Nurs 15:296–300; quiz 301
Mäkelä JT, Kiviniemi H, Juvonen T, Laitinen S (1995) Factors influencing wound dehiscence after midline laparotomy. Am J Surg 170:387–390
Begum B, Zaman R, Ahmed M, Ali S (2008) Burst abdomen-A preventable morbidity. Mymensingh Med J 17:63–66
Marwah S, Marwah N, Singh M, Kapoor A, Karwasra RK (2005) Addition of rectus sheath relaxation incisions to emergency midline laparotomy for peritonitis to prevent fascial dehiscence. World J Surg 29:235–239
National surgical quality improvement program (2005). American College of Surgeons, Chicago. Cited 17 Jan 2012. www.acsnsqip.org
User guide for the 2011 participant use data file. American College of Surgeons national surgical quality improvement program (2012). http://site.acsnsqip.org/wp-content/uploads/2012/03/2011-User-Guide_Final.pdf. Cited April 2015
Rodríguez-Hermosa JI, Codina-Cazador A, Ruiz B, Roig J, Gironès J, Pujadas M et al (2005) Risk factors for acute abdominal wall dehiscence after laparotomy in adults. Cir Esp 77:280–286
Shanmugam VK, Fernandez S, Evans KK, McNish S, Banerjee A, Couch K et al (2015) Postoperative wound dehiscence: predictors and associations. Wound Repair Regen 23:184–190
van Ramshorst GH, Eker HH, Harlaar JJ, Nijens KJ, Jeekel J, Lange JF (2010) Therapeutic alternatives for burst abdomen. Surg Technol Int 19:111–119
Gürleyik G (2001) Factors affecting disruption of surgical abdominal incisions in early postoperative period. Ulus Travma Derg 7:96–99
Yahchouchy-Chouillard E, Aura T, Picone O, Etienne JC, Fingerhut A (2003) Incisional hernias. I. Related risk factors. Dig Surg 20:3–9
Wicke C, Halliday B, Allen D, Roche NS, Scheuenstuhl H, Spencer MM et al (2000) Effects of steroids and retinoids on wound healing. Arch Surg 135:1265–1270
Anstead GM (1998) Steroids, retinoids, and wound healing. Adv Wound Care 11:277–285
Baca B, Ozben V, Boler DE, Onur E, Hamzaoglu I, Karahasanoglu T et al (2010) Effect of corticosteroid dose and duration of administration on colonic anastomosis. Inflamm Bowel Dis 16:2162–2167
Eubanks TR, Greenberg JJ, Dobrin PB, Harford FJ, Gamelli RL (1997) The effects of different corticosteroids on the healing colon anastomosis and cecum in a rat model. Am Surg 63:266–269
Phillips JD, Kim CS, Fonkalsrud EW, Zeng H, Dindar H (1992) Effects of chronic corticosteroids and vitamin A on the healing of intestinal anastomoses. Am J Surg 163:71–77
Lohsiriwat V, Chinswangwatanakul V, Lohsiriwat S, Akaraviputh T, Boonnuch W, Methasade A et al (2007) Hypoalbuminemia is a predictor of delayed postoperative bowel function and poor surgical outcomes in right-sided colon cancer patients. Asia Pac J Clin Nutr 16:213–217
Lohsiriwat V, Lohsiriwat D, Boonnuch W, Chinswangwatanakul V, Akaraviputh T, Lert-Akayamanee N (2008) Pre-operative hypoalbuminemia is a major risk factor for postoperative complications following rectal cancer surgery. World J Gastroenterol 14:1248–1251
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF (1999) Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg 134:36–42
Fuhrman MP, Charney P, Mueller CM (2004) Hepatic proteins and nutrition assessment. J Am Diet Assoc 104:1258–1264
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:448–454
Banh L (2006) Serum proteins as markers of nutrition: what are we treating? Pract Gastroenterol 30:46–64
Pierpont YN, Dinh TP, Salas RE, Johnson EL, Wright TG, Robson MC et al (2014) Obesity and surgical wound healing: a current review. ISRN Obes 2014:638936
Moghadamyeghaneh Z, Masoomi H, Mills SD, Carmichael JC, Pigazzi A, Nguyen NT, et al (2014) Outcomes of conversion of laparoscopic colorectal surgery to open surgery. JSLS 18:e2014.00230. doi:10.4293/JSLS.2014.00230
Wydra D, Emerich J, Sawicki S, Ciach K, Marciniak A (2006) Major complications following exenteration in cases of pelvic malignancy: a 10-year experience. World J Gastroenterol 12:1115–1119
Artioukh DY, Smith RA, Gokul K (2007) Risk factors for impaired healing of the perineal wound after abdominoperineal resection of rectum for carcinoma. Colorectal Dis 9:362–367
Cresti S, Ouaïssi M, Sielezneff I, Chaix JB, Pirro N, Berthet B et al (2008) Advantage of vacuum assisted closure on healing of wound associated with omentoplasty after abdominoperineal excision: a case report. World J Surg Oncol 6:136
Gümüş N (2009) Vacuum-assisted closure of perineal war wound related to rectum. Eplasty 9:e55
Mouës CM, Vos MC, van den Bemd GJ, Stijnen T, Hovius SE (2004) Bacterial load in relation to vacuum-assisted closure wound therapy: a prospective randomized trial. Wound Repair Regen 12:11–17
Cliby WA (2002) Abdominal incision wound breakdown. Clin Obstet Gynecol 45:507–517
Grace RH, Cox SJ (1973) Incidence of incisional hernia following dehiscence of the abdominal wound. Proc R Soc Med 66:1091–1092
White H, Cook J, Ward M (1977) Abdominal wound dehiscence. A 10-year survey from a district general hospital. Ann R Coll Surg Engl 59:337–341
Fleischer GM, Rennert A, Rühmer M (2000) Infected abdominal wall and burst abdomen. Chirurg 71:754–762
Carlson MA (1997) Acute wound failure. Surg Clin North Am 77:607–636
Israelsson LA, Millbourn D (2013) Prevention of incisional hernias: how to close a midline incision. Surg Clin North Am 93:1027–1040
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moghadamyeghaneh, Z., Hanna, M.H., Carmichael, J.C. et al. Wound Disruption Following Colorectal Operations. World J Surg 39, 2999–3007 (2015). https://doi.org/10.1007/s00268-015-3208-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3208-0