Abstract
Purpose
Inhalation of a foreign body is a real emergency in pediatric age and requires prompt diagnosis and treatment to reduce mortality. The objective of this study is to analyze clinical and radiological details, types, and localization of foreign bodies in patients conducted or to our hospital with suspected inhalation.
Methods
We conducted a retrospective analysis of all cases of foreign body inhalation admitted to our Pediatric Emergency Room between January 2009 and June 2022.
Results
171 patients were included in the study. In 83 patients, the FB was detected. The mean age of presentation was 2.3 years (SD: ± 2). Cough (73%) and unilateral reduced breath sound (51%) were the most common clinical symptom and clinical sign. The most frequent localization was the right main bronchus (43%). The foreign bodies retrieved were vegetable (83%), of which peanut was the most common. Chest radiographs were normal in 25%. The mean duration of hospitalization was 5 days (± 2.9). Complications such as pneumothorax were seen in two cases.
Conclusions
Foreign body inhalation represents a true pediatric emergency and still a challenge in clinical practice.
The best way to manage it is an early diagnosis and removal by fully trained staff.

Similar content being viewed by others
References
Brkic F, Umihanic S, Altumbabic H et al (2018) Death as a consequence of foreign body aspiration in children. Med Arch 72(3):220–223. https://doi.org/10.5455/medarh.2018.72.220-223
Cohen S, Avital A, Godfrey S, Gross M, Kerem E, Springer C (2009) Suspected foreign body inhalation in children: what are the indications for bronchoscopy? J Pediatr 155(2):276–280. https://doi.org/10.1016/J.JPEDS.2009.02.040
Adjeso T, Damah MC, Murphy JP, Anyomih TTK (2017) Foreign body aspiration in Northern Ghana: a review of pediatric patients. Int J Otolaryngol 2017:1–4. https://doi.org/10.1155/2017/1478795
Ministero della Salute I. Linee di indirizzo per la prevenzione del soffocamento da cibo in età pediatrica. Published online 2017:1–12.
Gregori D, Scarinzi C, Berchialla P et al (2007) The cost of foreign body injuries in the upper aero-digestive tract: need for a change from a clinical to a public health perspective? Int J Pediatr Otorhinolaryngol 71(9):1391–1398. https://doi.org/10.1016/J.IJPORL.2007.05.013
Snidero S, Soriani N, Baldi I, Zobec F, Berchialla P, Gregori D (2012) Scale-up approach in CATI surveys for estimating the number of foreign body injuries in the aero-digestive tract in children. Int J Environ Res Public Health 9(11):4056–4067. https://doi.org/10.3390/IJERPH9114056
Website SSSGroupSS. (2023) index @ https://www.susysafe.org. Accessed 23 Aug 2023
Perkins GD, Handley AJ, Koster RW et al (2015) European Resuscitation Council Guidelines for Resuscitation 2015:Section 2. Adult basic life support and automated external defibrillation. Resuscitation 95:81–99. https://doi.org/10.1016/J.RESUSCITATION.2015.07.015
Berg RA, Hemphill R, Abella BS et al (2010) Part 5: adult basic life support: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.110.970939
Number of choking deaths by place of occurrence and age, registered in England and Wales, 2014 to 2016 - Office for National Statistics. Accessed 17 Oct 2022. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/adhocs/007747numberofchokingdeathsbyplaceofoccurrenceandageregisteredinenglandandwales2014to2016
Cutrone C, Pedruzzi B, Tava G et al (2011) The complimentary role of diagnostic and therapeutic endoscopy in foreign body aspiration in children. Int J Pediatr Otorhinolaryngol 75(12):1481–1485. https://doi.org/10.1016/j.ijporl.2011.08.014
Pinzoni F, Boniotti C, Molinaro SM, Baraldi A, Berlucchi M (2007) Inhaled foreign bodies in pediatric patients: review of personal experience. Int J Pediatr Otorhinolaryngol 71(12):1897–1903. https://doi.org/10.1016/J.IJPORL.2007.09.002
Lee JJW, Philteos J, Levin M, Namavarian A, Propst EJ, Wolter NE (2021) Clinical prediction models for suspected pediatric foreign body aspiration: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg 147(9):1. https://doi.org/10.1001/JAMAOTO.2021.1548
Gonçalves JR, Feijó S, Monteiro P, Maulide I, de Almeida AB (2007) Tracheobronchial foreign bodies in children: fifteen years of experience in a respiratory endoscopy unit. Journal of Bronchology 14(2):79–82. https://doi.org/10.1097/LBR.0B013E3180463284
Dongol K, Neupane Y, Dutta H, Gyawali BR, Kharel B (2021) Prevalence of foreign body aspiration in children in a tertiary care hospital. JNMA J Nepal Med Assoc 59(234):111–115. https://doi.org/10.31729/JNMA.5393
Na’ara S, Vainer I, Amit M, Gordin A (2020) Foreign body aspiration in infants and older children: a comparative study. Ear Nose Throat J 99(1):47–51. https://doi.org/10.1177/0145561319839900
Reid A, Hinton-Bayre A, Vijayasekaran S, Herbert H (2020) Ten years of paediatric airway foreign bodies in Western Australia. Int J Pediatr Otorhinolaryngol. https://doi.org/10.1016/j.ijporl.2019.109760
Kiyan G, Gocmen B, Tugtepe H, Karakoc F, Dagli E, Dagli TE (2009) Foreign body aspiration in children: the value of diagnostic criteria. Int J Pediatr Otorhinolaryngol 73(7):963–967. https://doi.org/10.1016/j.ijporl.2009.03.021
Ciftci AO, Bingöl-Koloǧlu M, Şenocak ME, Tanyel FC, Büyükpamukçu N (2003) Bronchoscopy for evaluation of foreign body aspiration in children. J Pediatr Surg 38(8):1170–1176. https://doi.org/10.1016/S0022-3468(03)00263-X
The Royal Children’s Hospital Melbourne (2023). https://www.rch.org.au/clinicalguide/guideline_index/Foreign_bodies_inhaled/. Accessed 12 Sept 2023
Fidkowski CW, Zheng H, Firth PG (2010) The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg 111(4):1016–1025. https://doi.org/10.1213/ANE.0b013e3181ef3e9c
Antón-Pacheco JL, Cano I, Comas J et al (2006) Management of congenital tracheal stenosis in infancy. Eur J Cardiothorac Surg 29(6):991–996. https://doi.org/10.1016/j.ejcts.2005.12.061
Med AS. Foreign body removal. Accessed 21 Feb 21 2023. www.saudiannals.net
Sjogren PP, Mills TJ, Pollak AD, Muntz HR, Meier JD, Grimmer JF (2018) Predictors of complicated airway foreign body extraction. Laryngoscope 128(2):490–495. https://doi.org/10.1002/lary.26814
Skoulakis CE, Doxas PG, Papadakis CE, et al (2000) Bronchoscopy for foreign body removal in children. A review and analysis of 210 cases 53 www.elsevier.com/locate/ijporl. Accessed 19 July 2023
Author information
Authors and Affiliations
Contributions
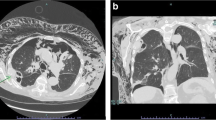
M.To, M.Tr.,M.Tr, and D.M. wrote the main manucript text. A.D, L.S have collected and analyzed data. S.S. and A.S. prepared Table 1 and Table 2 C.C. and prepared Figure 1 All authors reviewed the manucript
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Torsello, M., Sicuranza, L., Meucci, D. et al. Foreign body aspiration in children: our pediatric tertiary care experience. Pediatr Surg Int 40, 93 (2024). https://doi.org/10.1007/s00383-024-05679-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-024-05679-z