Abstract
Purpose
Recurrent severe hypoglycemic attacks often persist even after performing pancreatectomy for medically unresponsive congenital hyperinsulinism (CHI). In this study, we present our experience with redo pancreatectomy for CHI.
Methods
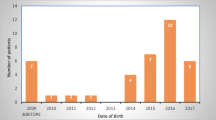
We reviewed all children who underwent pancreatectomy for CHI between January 2005 and April 2021 in our center. A comparison was made between patients whose hypoglycemia was controlled after primary pancreatectomy and patients who required reoperation.
Results
A total of 58 patients underwent pancreatectomy for CHI. Refractory hypoglycemia after pancreatectomy occurred in 10 patients (17%), who subsequently underwent redo pancreatectomy. All patients who required redo pancreatectomy had positive family history of CHI (p = 0.0031). Median extent of initial pancreatectomy was lesser in the redo group with borderline level of statistical significance (95% vs. 98%, p = 0.0561). Aggressive pancreatectomy at the initial surgery significantly (p = 0.0279) decreased the risk for the need to redo pancreatectomy; OR 0.793 (95% CI 0.645–0.975). Incidence of diabetes was significantly higher in the redo group (40% vs. 9%, p = 0.033).
Conclusion
Pancreatectomy with 98% extent of resection for diffuse CHI, especially with positive family history of CHI, is warranted to decrease the chance of reoperation for persistent severe hypoglycemia.
Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Al-Shanafey S, Habib Z, AlNassar S (2009) Laparoscopic pancreatectomy for persistent hyperinsulinemic hypoglycemia of infancy. J Pediatr Surg 44:134–138. https://doi.org/10.1016/j.jpedsurg.2008.10.120. (Discussion 138)
Menni F, de Lonlay P, Sevin C et al (2001) Neurologic outcomes of 90 neonates and infants with persistent hyperinsulinemic hypoglycemia. Pediatrics 107:476–479. https://doi.org/10.1542/peds.107.3.476
Carcassonne M, DeLarue A, LeTourneau JN (1983) Surgical treatment of organic pancreatic hypoglycemia in the pediatric age. J Pediatr Surg 18:75–79. https://doi.org/10.1016/s0022-3468(83)80277-2
Worth C, Yau D, Salomon Estebanez M et al (2020) Complexities in the medical management of hypoglycaemia due to congenital hyperinsulinism. Clin Endocrinol 92:387–395. https://doi.org/10.1111/cen.14152
Goel P, Choudhury SR (2012) Persistent hyperinsulinemic hypoglycemia of infancy: an overview of current concepts. J Indian Assoc Pediatr Surg 17:99–103. https://doi.org/10.4103/0971-9261.98119
Gross RE (1953) The surgery of infancy and childhood. WB Saunders, Philadelphia, p 574
Redkar R, Karkera PJ, Krishnan J et al (2015) Subtotal pancreatectomy for congenital hyperinsulinism: our experience and review of literature. Indian J Surg 77:778–782. https://doi.org/10.1007/s12262-013-0999-9
Schönau E, Deeg KH, Huemmer HP et al (1991) Pancreatic growth and function following surgical treatment of nesidioblastosis in infancy. Eur J Pediatr 150:550–553. https://doi.org/10.1007/BF02072204
Meissner T, Wendel U, Burgard P et al (2003) Long-term follow-up of 114 patients with congenital hyperinsulinism. Eur J Endocrinol 149:43–51. https://doi.org/10.1530/eje.0.1490043
Schiller M, Krausz M, Meyer S et al (1980) Neonatal hyperinsulinism—surgical and pathologic considerations. J Pediatr Surg 15:16–20. https://doi.org/10.1016/S0022-3468(80)80395-2
Ackermann AM, Palladino AA (2015) Managing congenital hyperinsulinism: improving outcomes with a multidisciplinary approach. RRED 5:103–117. https://doi.org/10.2147/RRED.S56608
Lord K, Radcliffe J, Gallagher PR et al (2015) High risk of diabetes and neurobehavioral deficits in individuals with surgically treated hyperinsulinism. J Clin Endocrinol Metab 100:4133–4139. https://doi.org/10.1210/jc.2015-2539
Reyes GA, Fowler CL, Pokorny WJ (1993) Pancreatic anatomy in children: emphasis on its importance to pancreatectomy. J Pediatr Surg 28:712–715. https://doi.org/10.1016/0022-3468(93)90039-N
Stanley CA (2016) Perspective on the genetics and diagnosis of congenital hyperinsulinism disorders. J Clin Endocrinol Metab 101:815–826. https://doi.org/10.1210/jc.2015-3651
Mohamed Z, Arya VB, Hussain K (2012) Hyperinsulinaemic hypoglycaemia:genetic mechanisms, diagnosis and management. J Clin Res Pediatr Endocrinol 4:169–181. https://doi.org/10.4274/jcrpe.821
Demirbilek H, Hussain K (2017) Congenital hyperinsulinism: diagnosis and treatment update. J Clin Res Pediatr Endocrinol 9:69–87. https://doi.org/10.4274/jcrpe.2017.S007
Al-Agha AE, Ahmad IA (2013) Characterization of the ABCC8 gene mutation and phenotype in patients with congenital hyperinsulinism in western Saudi Arabia. Saudi Med J 34:1002–1006
Pierro A, Nah SA (2011) Surgical management of congenital hyperinsulinism of infancy. Semin Pediatr Surg 20:50–53. https://doi.org/10.1053/j.sempedsurg.2010.10.009
Hussain K (2008) Diagnosis and management of hyperinsulinaemic hypoglycaemia of infancy. Horm Res 69:2–13. https://doi.org/10.1159/000111789
Adzick NS, De Leon DD, States LJ et al (2019) Surgical treatment of congenital hyperinsulinism: Results from 500 pancreatectomies in neonates and children. J Pediatr Surg 54:27–32. https://doi.org/10.1016/j.jpedsurg.2018.10.030
Danowitz M, De Leon DD (2022) The role of GLP-1 signaling in hypoglycemia due to hyperinsulinism. Front Endocrinol 13:863184. https://doi.org/10.3389/fendo.2022.863184
Palladino AA, Sayed S, Levitt Katz LE et al (2009) Increased glucagon-like peptide-1 secretion and postprandial hypoglycemia in children after Nissen fundoplication. J Clin Endocrinol Metab 94:39–44. https://doi.org/10.1210/jc.2008-1263
Patti ME, McMahon G, Mun EC et al (2005) Severe hypoglycaemia post-gastric bypass requiring partial pancreatectomy: evidence for inappropriate insulin secretion and pancreatic islet hyperplasia. Diabetologia 48:2236–2240. https://doi.org/10.1007/s00125-005-1933-x
Bizzarri C, Cervoni M, Crea F et al (2011) Dumping syndrome: an unusual cause of severe hyperinsulinemic hypoglycemia in neurologically impaired children with gastrostomy. Minerva Pediatr 63:67–71
Acknowledgements
We would like to thank Qutaiba N. M. Shah Mardan, MBBS, MRCS(Eng) for proof reading and language assistance.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Ali Al-Ameer] and [Afrah Alsomali]. The first draft of the manuscript was written by [Ali Al-Ameer]. The final draft was reviewed and adjusted by [Zakaria Habib]. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
Ethical approval was waived by the local Research Ethics Committee of King Faisal Specialist Hospital and Research Center in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Informed consent
A waiver of informed consent was granted by the institutional review board for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al-Ameer, A., Alsomali, A. & Habib, Z. Incidence, predictors and outcomes of redo pancreatectomy in infants with congenital hyperinsulinism: a 16-year tertiary center experience. Pediatr Surg Int 39, 183 (2023). https://doi.org/10.1007/s00383-023-05470-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05470-6