Abstract
Purpose
The purpose of our study was to perform a comparative analysis of the examination and treatment outcomes of children with cylindrical and button batteries (BB) ingestion depending on their size and anatomical locations.
Methods
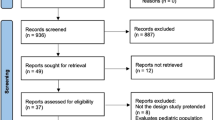
This study was a retrospective analysis of 124 children aged from 1 month to 18 years who ingested batteries and were treated in a tertiary care center from January 1, 2014 to March 31, 2019. The data studied included age, sex, presenting symptoms at the time of evaluation, type and size of battery and modality of management.
Results
Twenty-three (18.5%) patients ingested cylindrical batteries (CBs), and 101 (81.5%) ingested BBs. The duration of hospital stay was significantly longer (p = 0.004) in the group of children who ingested BBs larger than 20 mm. Endoscopic removal was performed in 75 (60.5%) children, 46 (37.1%) were followed up and three (2.4%) underwent open surgeries. Children with CBs ingestion, in 55% of cases, had gastric mucosal injuries. Children with BBs impacted in the esophagus in 96% cases had visible severe mucosal damage, whereas patients with gastric BB ingestion 19.5% had superficial gastric mucosal damage.
Conclusion
Performing timely endoscopic retrieval in children who are admitted early to the hospital will reduce the risk of damage to the gastrointestinal mucosa, especially in the stomach. Unlike BBs, CBs, despite their large size, have advantageous shapes, uneventfully pass the esophagus and are more often retained in the stomach; thus, mucosal injuries are more often observed in the stomach. Consequently, endoscopic extraction is the treatment of choice for children with BB ingestion.
Similar content being viewed by others
References
Centers for Disease Control and Prevention (CDC) (2012) Injuries from batteries among children aged < 13 years United States, 1995–2010. MMWR Morb Mortal Wkly Rep 61:661–700
Litovitz T, Whitaker N, Clark L et al (2010) Emerging battery-ingestion hazard: clinical implication. Pediatrics 125(6):1168–1177
Sharpe SJ, Rochette LM, Smith GA (2012) Pediatric battery-related emergency department visits in the United States, 1990–2009. Pediatrics 129:1111–1119
Lee JH (2018) Foreign body ingestion in children. Clin Endosc 51(2):129–136. https://doi.org/10.5946/ce.2018.039
Bekhof J, Norbruis O, Scheenstra R et al (2004) Babies and batteries. Lancet 364(8):708–709
Fuentes S, Cano I, Benavent MI, Gómez A (2014) Severe esophageal injuries caused by accidental button battery ingestion in children. J Emerg Trauma Shock 7(4):316–321. https://doi.org/10.4103/0974-2700.142773
Haddad N, Wilson JD, Fard D, Levi JR (2020) Pediatric button battery ingestion: publication trends in the literature. Am J Otolaryngol. https://doi.org/10.1016/j.amjoto.2020.102401
Leinwand K, Brumbaugh DE, Kramer RE (2016) Button battery ingestion in children: a paradigm for management of severe pediatric foreign body ingestions. Gastrointest Endosc Clin N Am 26(1):99–118. https://doi.org/10.1016/j.giec.2015.08.003
Marom T, Goldfarb A, Russo E et al (2010) Battery ingestion in children. Intern J Ped Otorhinolaryngol 74:849–854
Lerner DG, Brumbaugh D, Lightdale JR, Jatana KR, Jacobs IN, Mamula P (2020) Mitigating risks of swallowed button batteries: new strategies before and after removal. J Pediatr Gastroenterol Nutr 70(5):542–546. https://doi.org/10.1097/MPG.0000000000002649 (PMID: 32022776)
Pugmire BS, Lim R, Avery LL (2015) Review of ingested and aspirated foreign bodies in children and their clinical significance for radiologists. Radiographics 35(5):1528–1538. https://doi.org/10.1148/rg.2015140287
Honda S, Shinkai M, Usui Y et al (2010) Severe gastric damage caused by button battery ingestion in a 3 month-old infant. J Pediatr Surg 45:e23–e26
Kramer RE, Lerner DG, Lin T, Manfredi M, Shah M, Stephen TC (2015) Management of ingested foreign bodies in children JPGN. J Pediatr Gasteroenterol. https://doi.org/10.1097/MPG.0000000000000729
Thomson M, Tringali A, Dumonceau JM, Tavares M, Tabbers MM, Furlano R, Spaander M, Hassan C, Tzvinikos C, Ijsselstijn H, Viala J, Dall’Oglio L, Benninga M, Orel R, Vandenplas Y, Keil R, Romano C, Brownstone E, Hlava Š, Gerner P, Dolak W, Landi R, Huber WD, Everett S, Vecsei A, Aabakken L, Amil-Dias J, Zambelli A (2017) Paediatric gastrointestinal endoscopy: European Society for Paediatric Gastroenterology Hepatology and Nutrition and European Society of Gastrointestinal Endoscopy Guidelines. J Pediatr Gastroenterol Nutr 64(1):133–153. https://doi.org/10.1097/MPG.0000000000001408.PMID:27622898
Khaled et al (2020) Gastric injury secondary to button battery ingestions; a retrospective multicenter review. Gastrointest Endosc 92:276–283
National Capital Poison Control Center. National capital poison center button battery ingestion triage and treatment guideline. Available at: https://www.poison.org/battery/guideline. Accessed on March 24, 2021
Rios G, Rodriguez L, Lucero Y et al (2020) Endoscopic findings associated with button battery ingestion in children: do we need to change the protocol for managing gastric location? Pediatr Emerg Care. https://doi.org/10.1097/PEC.0000000000001415
Mubarak A, Benninga MA, Broekaert I, Dolinsek J, Homan M, Mas E, Miele E, Pienar C, Thapar N, Thomson M, Tzivinikos C, de Ridder L (2021) Diagnosis, management, and prevention of button battery ingestion in childhood: A European Society for Paediatric Gastroenterology Hepatology and Nutrition Position Paper. J Pediatr Gastroenterol Nutr 73(1):129–136. https://doi.org/10.1097/MPG.0000000000003048 (PMID: 33555169)
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akilov, K.A., Asadullaev, D.R., Yuldashev, R.Z. et al. Cylindrical and button battery ingestion in children: a single-center experience. Pediatr Surg Int 37, 1461–1466 (2021). https://doi.org/10.1007/s00383-021-04953-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04953-8