Abstract
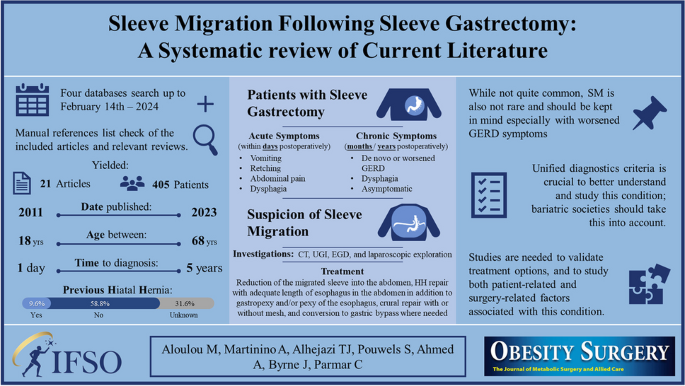
Sleeve gastrectomy (SG) is the most frequently performed bariatric procedure worldwide. The incidence and consequences of sleeve migration (SM) are not clearly understood. There is no clear consensus on appropriate measures to reduce the risk of SM. This study systematically reviewed the literature and identified 405 cases of SM from 21 studies. Age ranged from 18 to 68 years. Thirty-two percent and 11% of patients were females and males respectively, while sex was not reported in 57%. Time to diagnosis ranged from 1 day to 5 years postoperatively. A total of 9.6% and 58.8% of patients had or had no previous hiatal hernia respectively. SM incidence, risk factors, proposed mechanisms, clinical presentation, diagnosis, management, and potential preventive strategies are described in this review.
Graphical Abstract

Similar content being viewed by others
References
IFSO. 8TH global registry report. 2023. https://www.ifso.com/pdf/8th-ifso-registry-report-2023.pdf.
Baumann T, Grueneberger J, Pache G, Kuesters S, Marjanovic G, Kulemann B, et al. Three-dimensional stomach analysis with computed tomography after laparoscopic sleeve gastrectomy: sleeve dilation and thoracic migration. Surg Endosc. 2011;25(7):2323–9.
Karila-Cohen P, Pelletier AL, Saker L, Laouénan C, Bachelet D, Khalil A, et al. Staple line intrathoracic migration after sleeve gastrectomy: correlation between symptoms, CT three-dimensional stomach analysis, and 24-h pH monitoring. Obes Surg. 2022;32(7):1–9.
Sabry K, Elmaleh HM, El-Swaify ST, Refaat MA, Atiya MAN, Alazab E, et al. Surgical management algorithm for intrathoracic sleeve migration: a retrospective series and literature review. J Laparoendosc Adv Surg Tech. 2022;32(10):1078–91.
Saber AA, Shoar S, Khoursheed M. Intra-thoracic sleeve migration (ITSM): an underreported phenomenon after laparoscopic sleeve gastrectomy. Obes Surg. 2017;27(8):1917–23.
Oshiro T, Wakamatsu K, Nabekura T, Moriyama Y, Kitahara N. The potential of a polyglycolic acid sheet for preventing intrathoracic sleeve migration. Minim Invasive Ther Allied Technol. 2023;32(4):199–206.
Fouad MMB, Ibraheim SMN, Ibraheim P, Maurice KK, Saber AT. Assessment of the role of omentopexy in laparoscopic sleeve gastrectomy: a tertiary center experience. J Laparoendosc Adv Surg Tech. 2022;32(9):962–8.
Castagneto-Gissey L, Genco A, Del Corpo G, Badiali D, Pronio AM, Casella G. Sleeve gastrectomy and gastroesophageal reflux: a comprehensive endoscopic and pH-manometric prospective study. Surg Obes Relat Dis. 2020;16(11):1629–37.
Arnoldner MA, Felsenreich DM, Langer FB, Weber M, Mang T, Kulinna-Cosentini C, et al. Pouch volume and pouch migration after Roux-en-Y gastric bypass: a comparison of gastroscopy and 3 D-CT volumetry: is there a “migration crisis”? Surg Obes Relat Dis. 2020;16(12):1902–8.
Meknat A, Fernandez-Ranvier G, Hariri K, Guevara DE, Beitner M, Herron DM. Intrathoracic sleeve migrations after sleeve gastrectomy: a compilation of case reports. J Laparoendosc Adv Surg Tech. 2020;30(9):1013–7.
Amor Ben I, Debs T, Kassir R, Anty R, Amor Ben V, Gugenheim J. De novo hiatal hernia of the gastric tube after sleeve gastrectomy. Int J Surg Case Rep. 2015;15:78–80.
Bhandarkar S, Kalikar V, Nasta A, Goel R, Patankar R. Post-laparoscopic sleeve gastrectomy, intrathoracic sleeve migration and its management: a case series and review of literature. J Minim Access Surg. 2023;19(4):544–7.
Boru CE, Termine P, Antypas P, Iossa A, Ciccioriccio CM, de Angelis F, et al. Concomitant hiatal hernia repair during bariatric surgery: does the reinforcement make the difference? Minerva Chir. 2021;76(1):33–42.
Choi SJ, Kim SM. Intrathoracic migration of gastric sleeve affects weight loss as well as GERD–an analysis of remnant gastric morphology for 100 patients at one year after laparoscopic sleeve gastrectomy. Obes Surg. 2021;31(7):2878–86.
Dalkılıç MS, Erdem H, Gençtürk M, Yılmaz M, Sisik A. Acute intrathoracic migration with incarceration of laparoscopic sleeve gastrectomy due to incomplete hiatal hernia repair. Cureus. 2022;14(11):11–4.
Genco A, Soricelli E, Casella G, Maselli R, Castagneto-Gissey L, Di Lorenzo N, et al. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg Obes Relat Dis. 2017;13(4):568–74.
Hon HH, Birriel TJ, El CM. Gastric sleeve migration conversion to a Roux-en-Y gastric bypass in combination with wedge fundectomy and paraesophageal hernia repair. Surg Obes Relat Dis. 2018;14(3):426–7.
Mizrahi I, Tabak A, Grinbaum R, Beglaibter N, Eid A, Simanovsky N, et al. The utility of routine postoperative upper gastrointestinal swallow studies following laparoscopic sleeve gastrectomy. Obes Surg. 2014;24(9):1415–9.
Pavelko Y, Bustos R, Gruessner S, Hassan C. Acute hiatal hernia with incarcerated proximal half of recent sleeve gastrectomy: super rare complication. Obes Surg. 2021;31(1):469–71.
Sebastiani S, Nagliati C, Barreca M. Gastric herniation following laparoscopic sleeve gastrectomy: a rare acute complication. Austin J Surg. 2014;1(9):1044.
Termine P, Boru CE, Iossa A, Ciccioriccio MC, Campanelli M, Bianciardi E, et al. Transhiatal migration after laparoscopic sleeve gastrectomy: myth or reality? A multicenter, retrospective study on the incidence and clinical impact. Obes Surg. 2021;31(8):3419–26.
Al-Sanea O, Al-Garzaie A, Dernaika M, Haddad J. Rare complication post sleeve gastrectomy: acute irreducible paraesophageal hernia. Int J Surg Case Rep. 2015;8:88–91.
Alwatari Y, Roriz-Silva R, Bolckmans R, Campos GM. Intrathoracic sleeve gastrectomy migration with gastric volvulus treated with laparoscopic repair and conversion to gastric bypass. J Surg Case Reports. 2020;2020(8):1–4.
Parmar CD, Khalil H, Lakdawala M, Bhan C, Sufi P. Gastro-colic fistula after sleeve gastrectomy leak: our experience with this rare complication. Obes Surg. 2019;29(11):3771–2.
Stier C, Parmar C, Koschker AC, Bokhari M, Stier R, Chiappetta S. Computed tomography-3D-volumetry: a valuable adjunctive diagnostic tool after bariatric surgery. Mini-invasive Surg. 2020;4–18. https://doi.org/10.20517/2574-1225.2019.75.
Parmar CD, Gan J, Stier C, Dong Z, Chiappetta S, El-Kadre L, et al. One Anastomosis/Mini Gastric Bypass (OAGB-MGB) as revisional bariatric surgery after failed primary adjustable gastric band (LAGB) and sleeve gastrectomy (SG): a systematic review of 1075 patients. Int J Surg. 2020;81(July):32–8.
Rheinwalt KP, Schipper S, Plamper A, Alizai PH, Trebicka J, Brol MJ, et al. Roux-en-Y versus one anastomosis gastric bypass as redo-operations following sleeve gastrectomy: a retrospective study. World J Surg. 2022;46(4):855–64.
Nakanishi H, Mosleh KA, Al-Kordi M, Farsi S, Chaudhry S, Marrero K, et al. One anastomosis gastric bypass as revisional surgery following sleeve gastrectomy: a systematic review and meta-analysis. Obes Surg. 2024;34(2):429–41.
Biter LU, ‘tHart JW, Noordman BJ, Smulders JF, Nienhuijs S, Dunkelgrün M, et al. Long-term effect of sleeve gastrectomy vs Roux-en-Y gastric bypass in people living with severe obesity: a phase III multicentre randomised controlled trial (SleeveBypass). Lancet Reg Heal Eur. 2024;38:100836.
Elmaleh HM, Elnabeel Mortada A, Khaled RA. Evaluation of anterior phrenoesophageal ligament preservation during hiatus hernia repair in laparoscopic sleeve gastrectomy as an anti-reflux measure. J Laparoendosc Adv Surg Tech. 2021;31(5):507–14.
Stier C, Chen W, Chong TH, Yang J, Parmar C, Wang C. Step-by-step instructions for the innovative three-port-technique of laparoscopic sleeve gastrectomy: how I do it? 2021;1–13. https://doi.org/10.21203/rs.3.rs-146710/v1.
Skalli EM, Parmar CD. Necrosis of the Nissen-sleeve gastrectomy (N-SG) wrap. Obes Surg. 2020;30(10):4174–5.
Kermansaravi M, Parmar C, Chiappetta S, Shikora S, Aminian A, Abbas SI, et al. Best practice approach for redo-surgeries after sleeve gastrectomy, an expert’s modified Delphi consensus. Surg Endosc. 2023;37(3):1617–28.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Consent to Participate
Informed consent does not apply.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• SM should be a DDx after SG, especially in those with worsened GERD symptoms.
• Long-term follow-up after MBS is crucial to deliver the best possible patient care.
• Further studies are needed to validate the current treatment options for SM.
• Bariatric societies should work on a unified diagnostics criteria for SM.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aloulou, M., Martinino, A., Alhejazi, T.J. et al. Sleeve Migration Following Sleeve Gastrectomy: A Systematic Review of Current Literature. OBES SURG 34, 2237–2247 (2024). https://doi.org/10.1007/s11695-024-07259-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-024-07259-5



