Abstract
Purpose
Medulloblastoma (MB) is the most common malignant pediatric brain tumor. Current treatment allows decent survival rates but often with life-long morbidity. Molecular classification provides a base for novel therapeutic approaches. However, these groups are heterogeneous. MicroRNA-125a has a tumor suppressor function. It is downregulated in several tumors. The expression of microRNA-125a in MB patients remains unclear. Therefore, this study was designed to evaluate the expression of microRNA-125a in molecular groups of pediatric MB patients in Egyptian population and its clinical significance.
Methods
Formalin-fixed, paraffin-embedded tissue blocks from 50 pediatric MB patients were retrospectively collected. Immunohistochemistry for β-catenin, GAB1, YAP1, and p53 was done for molecular classification. MicroRNA-125a expression analysis was done using qRT-PCR. Follow-up data were obtained from patients’ records.
Results
MicroRNA-125a expression was significantly lower in MB patients showing large cell/anaplastic (LC/A) histology and in the non-WNT/non-SHH group. Lower levels of microRNA-125a showed a tendency toward poor survival rates; however, difference was not significant. Infants and larger preoperative tumor size were significantly associated with lower survival rates. On a multivariate analysis, preoperative tumor size was an independent prognostic factor.
Conclusion
MicroRNA-125a expression was significantly lower in categories of pediatric MB patients with worse prognosis namely LC/A histology and the non-WNT/non-SHH group suggesting a pathogenetic role. MicroRNA-125a expression could represent a promising prognostic factor and a potential therapeutic target in the non-WNT/non-SHH group which represents the most common and the most heterogeneous group of pediatric MBs coupled with the highest rates of disseminated disease. Preoperative tumor size represents an independent prognostic factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medulloblastoma (MB) is the most common malignant pediatric brain tumor [1]. Children aged 4 to 9 years old show the highest incidence at 44% [2].
Studies of MB demonstrated that mutations in cell signaling pathways are associated with specific gene expression signatures, which could be detected using relatively simple and widely available techniques [3]. This has led to the introduction of the molecular subtyping in the 2016 World Health Organization (WHO) classification which is still endorsed by the 2021 WHO classification [4, 5].
According to the 2021 WHO classification of central nervous system (CNS) tumors, MBs are classified based on histopathological features and molecular characteristics. According to molecular characteristics, MB is classified into four groups: WNT (wingless-related integration site)-activated MBs, SHH (sonic hedgehog)-activated MBs which are separated into TP53-mutant and TP53-wild-types, and non-WNT/non-SHH MBs, comprising group 3 and group 4 which are listed as provisional variants [5].
The current treatment of MB allows 5-year survival rates ranging between 50 and 90%. This wide range is multifactorial depending on age at diagnosis, the presence of metastasis at diagnosis, histological pattern, and molecular group. Moreover, current therapeutic modalities come at the expense of life-long morbidity [6]. Therefore, the recent WHO classification has provided a base for novel therapeutic approaches that target cell signaling pathways that are activated aberrantly in MB [7]. However, these groups are heterogeneous, and they need more research to improve the molecular understanding and management of MB [8].
MicroRNAs are small noncoding RNAs that regulate gene expression through sequence-specific binding to 3′-untranslated regions of mRNAs, resulting in translational inhibition or mRNA degradation [9]. Some microRNAs show altered expression in many malignancies suggesting a critical role played by them in tumorigenesis [10].
The published literature largely lacks detailed studies of microRNA expression in MBs. A single study, conducted before the release of the 2016 WHO classification, focused on microRNA expression profiling in MB, where specific microRNA signatures distinguished tumors from normal cerebellar tissues [11].
MicroRNA-125a is located at 19q13. It is expressed in differentiated cells and acts as an antiproliferative factor. MicroRNA-125a expression is downregulated in several tumors [12]. MicroRNA-125a gene has two mature microRNAs in its precursor structure: hsa-mir-125a-5p and hsa-mir-125a-3p. MiR-125a-5p has a prognostic role in several tumors, and its mimic alone or in combination with other therapeutic agents could be a novel therapeutic approach against these tumors [13].
To date, the expression profile of microRNA-125a in MB patients remains unclear. Therefore, this study was designed to evaluate the expression of microRNA-125a in different molecular groups of pediatric MB patients in Egyptian population and its clinical significance.
Methods
The current retrospective study included tumor samples from 50 archived formalin-fixed, paraffin-embedded (FFPE) tissue blocks obtained from MB patients up to the age of 18 years. Samples were obtained from the Pathology Department, Faculty of Medicine, Alexandria University, Egypt, during the period from 2009 to 2018 upon the approval of the ethics committee at the Faculty of Medicine, Alexandria University. None of the patients previously received chemotherapy or radiotherapy.
Patient’s data
Clinical and follow-up data were obtained by reviewing patients’ records at the Clinical Oncology Department, Borg El-Arab Children’s Cancer Hospital, Alexandria University, Egypt. The date of assessment was January 2022.
Patients were classified into standard- and high-risk groups based on age at diagnosis, presence/absence of leptomeningeal dissemination (based on magnetic resonance imaging (MRI) and cerebrospinal fluid (CSF) analysis), extent of residual tumor after resection, and presence/absence of large cell/anaplastic (LC/A) histology. Standard-risk patients are children aged > 3 years without leptomeningeal dissemination, postoperative residual tumor < 1.5cm2, and non-LC/A histology [6].
Infants received HIT-SKK protocol with intensive chemotherapy followed by craniospinal radiotherapy at the age of 3 years [14].
Standard-risk patients were treated with whole CNS radiotherapy 23.4 Gy and boost up to 54 Gy with weekly vincristine. High-risk patients were treated with whole CNS radiotherapy 36 Gy and boost up to 54 Gy. Both standard- and high-risk patients received adjuvant chemotherapy (8 cycles of cisplatin, Endoxan, and vincristine) [15,16,17].
Histopathologic examination
Diagnosis was made conforming to the WHO criteria of 2021 [5].
Immunohistochemistry (IHC)
It was performed on 4-μm FFPE tissue sections using Dako PT Link unit and Dako Autostainer (Link 48, Agilent Technologies Inc., CA, USA).
For molecular classification, IHC for β-catenin antibody, a mouse monoclonal antibody (clone 15B8, 14–2567-82, Thermo Fischer Scientific, CA, USA), GAB1 antibody, a rabbit polyclonal antibody (GTX111253, GeneTex, CA, USA), YAP1 antibody, a mouse monoclonal antibody (G-6, sc-376830, Santa Cruz Biotechnology Inc., CA, USA), and p53 (DO-7, Leica Biosystems Inc., IL, USA) was done [18].
WNT group was identified by positive nuclear staining of β-catenin (≥ 5%) [19] and YAP1 nuclear positivity, while the SHH group was identified by positive cytoplasmic immunostaining of GAB1 (≥ 25%) [18] and YAP1 nuclear positivity. Non-WNT/non-SHH tumors were identified by negative nuclear β-catenin, GAB1, and YAP1 staining [20]. P53 immunostaining was performed in the SHH group where widespread strong nuclear positivity was considered as TP53-mutant, while scattered weak nuclear positivity was considered as TP53-wild-type [5].
For cases of LC/A histology, synaptophysin and integrase interactor 1 (INI 1) IHC were performed to confirm the diagnosis.
Histochemical staining for reticulin
It was performed in cases of histologically detected nodules to differentiate between desmoplastic nodular MB (DNMB) and biphasic pattern of classic MB.
Quantitative reverse transcription-polymerase chain reaction (qRT-PCR)
-
1.
Expression profile analysis of microRNA and quantitative real-time PCR
-
1.1.
RNA extraction from FFPE tissue samples
Samples were deparaffinized using deparaffinization solution (cat. no. 19093) and protease digested; then, total RNA isolation from samples was performed using QIAGEN® RNeasy FFPE Kit (ID: 73,504) according to the manufacturer’s instructions.
The RNA concentration and purity were measured using NanoDrop 2000/2000c spectrophotometer (Thermo Scientific, USA).
-
1.2.
Real-time qRT-PCR
Complementary DNA (cDNA) was synthesized using TaqMan ®MicroRNA Reverse Transcription Kit with miRNA specific primers (Applied Biosystems, USA).
RT reactions for target (microRNA-125a) and spiked-in control (RNU6B) were performed. In brief, 10 ng of RNA, specific stem-loop primers for each miRNA, 10 × buffer, dNTPs, reverse transcriptase, and RNase inhibitor were loaded in a thermal cycler (Primus 25 advanced, PEQLAB, UK) following the manufacturer’s protocol.
Then real-time PCR was carried out using the miRNA-specific TaqMan probes and TaqMan universal master mix in Applied Biosystems StepOne™ Real-Time PCR System. The expression levels of the miRNA-125a in each sample were normalized to those of RNU6B. The arithmetic formula (2−ΔCT) was used to calculate the median and range for each group as individual data points, and the difference in expression between patient groups was assessed [21].
-
1.1.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS ver. 25 Chicago, IL, USA) [22]. Descriptive statistics were summarized for categorical variables as frequencies and percentages and for continuous variables as mean (M) and median (Mdn). Various tests were used including Mann–Whitney (U), Kruskal–Wallis (H), Pearson’s correlation (r), and Spearman’s rho correlation coefficient (ρ).
Overall survival (OS) was defined as the time from diagnosis until death or last visit. Event-free survival (EFS) was defined as the time from diagnosis until disease recurrence/progression or death. Log rank test was used to compare the patients’ outcome between different groups. Univariate Cox regression was used to evaluate the effect of continuous covariates on patients’ outcome.
For the multivariate analysis, Cox survival regression analysis was used. For each variable, hazard ratio (HR) was calculated, and its 95% confidence interval (CI) was determined. In all statistical tests, level of significance of 0.05 was used, which the results were considered to be statistically significant.
Results
Clinicopathological characteristics
The current study included 50 MB patients: 32 (64%) were males, and 18 (36%) were females. Age of the patients ranged between 2 and 18 years (M = 9.7, ± 5.1 years); 5 (10%) were ≤ 3 years, and 45 (90%) were > 3 years; 22 patients (44%) were standard risk, and 28 patients (56%) were high risk.
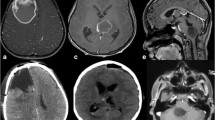
35 cases (70%) showed classic histology, while 13 cases (26%) were DNMB, and only 2 cases (4%) showed LC/A histology. One case (2%) belonged to the WNT group, the SHH-activated and TP53-wild-type group represented 13 cases (26%), and 36 cases (72%) belonged to the non-WNT/non-SHH group (Figs. 1 and 2). Clinicopathological characteristics of patients based on molecular classification are listed in Table 1. Statistical analysis showed that histology and preoperative size of the tumor (cm2) showed significant relation to molecular groups (p = < 0.001 and 0.03, respectively), where all SHH-activated and TP53-wild-type groups were associated with DNMB histology (100%), and the non-WNT/non-SHH group was associated with classic histology in 94.4% of cases. The preoperative size of tumor in the SHH-activated and TP53-wild-type group (Mdn = 22.5) was significantly larger than in the non-WNT/non-SHH group (Mdn = 16).
Histopathological and immunohistochemical results of MB cases. WNT MB a classic histology (H&E × 400), b β-catenin positive nuclear staining (anti β-catenin X400), c GAB1 negative staining (anti GAB1 X400) d YAP1 positive nuclear staining (anti YAP1 X400); SHH-activated & TP53-wildtype MB e desmoplastic nodular histology (H&E X400) f β-catenin cytoplasmic staining (anti β-catenin X400) g GAB1 positive cytoplasmic staining (anti GAB1 X400) h YAP1 internodular positive nuclear staining and scattered positive intranodular cells (anti YAP1 X400); non-WNT/non-SHH MB i classic histology (H&E X400) j β-catenin cytoplasmic staining (anti β-catenin X400) k GAB1 negative staining (anti GAB1 X400) l YAP1 negative staining (anti YAP1 X400); non-WNT/non-SHH MB m LC/A histology (H&E X400) n β-catenin cytoplasmic staining (anti β-catenin X400) o GAB1 negative staining (anti GAB1 X200) p YAP1 negative staining (anti YAP1 X400)
SHH-activated TP53-wildtype MB a the nodules are reticulin-free zones surrounded by a dense intercellular reticulin fiber network. (Reticulin stain X100) b p53 positive nuclear staining in scattered cells (wild type pattern) (anti p53 X400). Non-WNT/non-SHH MB, LC/A histology c synaptophysin positive cytoplasmic staining (anti synaptophysin X200) d retained INI1 nuclear staining (anti INI1 X400)
One case belonged to WNT molecular group; the patient was 15 years old, and the cross-sectional area of the tumor was 13.5cm2, high risk with postoperative residual > 1.5 cm2, and showed classic histology. For statistical reasons, this case was not included in statistical analysis Fig. 1.
MicroRNA-125a expression in MB patients
2−∆CT ranged between 0.000019 and 324 (Mdn = 8.3).
Relation between microRNA-125a expression and clinicopathological parameters
MicroRNA-125a levels showed significant relation with histological patterns and molecular groups. The levels of microRNA-125a were significantly lowest in cases with LC/A histology (Mdn = 2.2) followed by classic histology (Mdn = 6) followed by DNMB (Mdn = 20) (p = 0.049). The levels of microRNA-125a in the non-WNT/non-SHH group (Mdn = 5.6) were significantly lower than the levels of microRNA-125a in the SHH-activated and TP53-wild-type group (Mdn = 20.3) (p = 0.026) (Table 2, Fig. 3).
There was no statistically significant correlation between levels of microRNA-125a and either preoperative size of the tumor (rs = 0.314 and p = 0.136) or age of the patients (rs = − 0.265 and p = 0.063).
Survival analysis
Median follow-up time was 37 months. The number of deaths in patients included in the study was 23 (46%). The 5-year OS was 60% with a mean of 77 months and a median of 69 months (95% CI, 61.873–92.418). The number of events was 28 (56%). The 5-year EFS was 42% with a mean of 64.5 months and a median of 39 months (95% CI, 48.821–80.318).
Effect of microRNA-125a expression on clinical outcome of MB patients
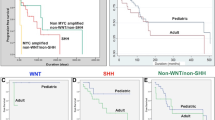
MicroRNA-125a expression was divided into low- and high-expression levels in relation to median. The 5-year OS tends to be lower in the cases with low microRNA-125a than the cases with high microRNA-125a (52% versus 70%). The cases with low microRNA-125a levels showed a tendency for lower EFS (Mdn = 33 months) than the cases with high microRNA-125a levels (Mdn = 42 months). Neither of the differences in OS and EFS were significant (X2 = 0.000 and 0.189, p = 1 and 0.664 respectively) (Table 3, Fig. 4a, b).
Kaplan–Meier survival curves for microRNA-125a expression in pediatric MBs. Patients were sub-divided into high and low microRNA-125a expression groups based on the median expression values. a and b OS and EFS for microRNA-125a in the 50 MB patients under the study, c OS for microRNA-125a expression in non-WNT/non-SHH molecular group, d OS for microRNA-125a expression in SHH-activated & TP53-wildtype molecular group, e OS for microRNA-125a expression in standard-risk group, f OS for microRNA-125a expression in high-risk group
Relations of OS and EFS to different clinicopathological parameters (Table 3)
Kaplan–Meier curves revealed that EFS in patients ≤ 3 years of age (Mdn = 6 months) was significantly lower than patients > 3 years of age (Mdn = 56 months), (X2 = 6.3, p = 0.012). Univariate Cox regression showed that each unit increase in size of the tumor seems to increase the hazard of the event both for OS and EFS; this was significant in EFS (EFS: HR = 1.078, p = 0.031), but it was not significant in OS (OS: HR = 1.062, p = 0.165).
Multivariate Cox model
It was then performed to identify the relationship between prognosis and the following covariates: microRNA-125a gene expression, age of the patients, and preoperative tumor size. Although the increased microRNA-125a gene expression and older age of the patients seemed to be protective against the event in both OS and EFS, this relation was not statistically significant (OS: HR = 0.870 and 0.265, p = 0.607 and 0.266 respectively; EFS: HR = 0.943 and 0.492, p = 0.792 and 0.524 respectively). Each unit increase in size of the tumor seemed to increase the hazard of the event both for OS and EFS; this was statistically significant in EFS (EFS: HR = 1.085, p = 0.040) (Table 4).
Evaluation of microRNA-125a gene expression within molecular and risk groups
Low levels of microRNA-125a expression showed a probability of poor outcome within the non-WNT/non-SHH group (50% 5-year OS for cases with low microRNA-125a versus 65% 5-year OS for cases with high microRNA-125a). However, the difference was not statistically significant (X2 = 0.041, p = 0.840). Conversely, within the SHH-activated and TP53-wild-type group, the 5-year OS for cases with low microRNA-125a (67%) was close to those with high microRNA-125a (70%). This result was not statistically significant (X2 = 0.398, p = 0.528) (Fig. 4c, d).
Low levels of microRNA-125a expression were possibly associated with poor outcome within both standard-risk group (58% 5-year OS for cases with low microRNA-125a versus 90% 5-year OS for cases with high microRNA-125a) and high-risk group (45% 5-year OS for cases with low microRNA-125a versus 55% 5-year OS for cases with high microRNA-125a). However, the differences were not statistically significant (X2 = 0.784 and 0.236, p = 0.376 and 0.627 respectively) (Fig. 4e, f).
Discussion
MB is the most common malignant pediatric brain tumor [23]. Advances in molecular profiling identified four molecular groups that guided clinical decision [8]. However, in a recent study, seven molecular subgroups were identified. While WNT remained the same, SHH, group 3, and group 4 were split into further groups, hence reflecting heterogeneity at the molecular level which brings challenge to understanding the biology of MB with impact on treatment options [24]. The current treatment regimens show considerable morbidity. Thus, numerous treatment strategies are designed and tailored in light of our molecular understanding of MBs [25].
In the present work, 5-year OS was 60% which is consistent with those reported in the literature (50–70%) [26]. Age showed a prognostic role where children ≤ 3 years old conferred poor survival, in accordance with findings observed by Zeltzer et al. [27].
It was also found in a uni- and multivariate analysis that preoperative tumor size represents an independent prognostic factor, where the larger the tumor, the poorer the prognosis with significant relation to EFS rates. Our findings are similar to those reported by Evans et al. [28].
MicroRNAs play important roles in regulating gene expression acting as either oncogenes or tumor suppressors under certain conditions [29].
MicroRNA-125a expression is downregulated in several tumors and was found to be a prognostic marker and a potential for therapeutic target in some of these tumors [12, 13].
In a single study, conducted before the release of the 2016 WHO classification, Ferretti et al. found that most microRNAs displayed overall downregulated expression in MB [11].
The current study is the first study to report the expression profile and clinical significance of microRNA-125a in molecular groups of MB and to evaluate its prognostic significance. Fifty MB tumors were collected retrospectively and classified into three molecular groups. The relation between microRNA-125a and different clinicopathological parameters showed statistically significant relation to histology and molecular groups, while there was no significant relation to age or tumor size. MicroRNA-125a was significantly lower in MB cases with LC/A histology followed by classic histology and then DNMB. It was also significantly lower in non-WNT/non-SHH molecular group than SHH-activated and TP53-wild-type. The one WNT MB case could not be included in statistical analysis.
In the present work, it was found that lower levels of microRNA-125a were associated with parameters described in the literature to have worse prognosis namely LC/A histology and non-WNT/non-SHH molecular group suggesting a pathogenetic role for microRNA-125a in these tumors. Huang et al. stated that LC/A histology was one of the most significant factors associated with worse survival rates [30].
In the current study, SHH-activated and TP53-wild-type MB showed 70% 5-year OS, while non-WNT/non-SHH MB showed 55% 5-year OS, consistent with the findings in literature where SHH-activated and TP53-wild-type MB proved to have a favorable outcome [31], while non‐WNT/non‐SHH tumors have the worst prognosis overall [32].
The lower levels of microRNA-125a in categories with worse prognosis could be explained by the findings in literature suggesting that it has tumor suppressor function through inhibiting proliferation, invasiveness, and metastasis [33]. It was found to be downregulated in different tumors, where its upregulation by targeted therapy induced apoptosis. In neuroblastoma, it was found to interfere with the expression of proproliferative truncated isoform of the neurotrophin receptor tropomyosin–related kinase C (t-trkC), where its underexpression was associated with poor prognosis [34]. In glioblastoma, microRNA-125a is downregulated where it targets podoplanin and inhibits cell migration and invasion [35]. According to Ferretti et al., specific microRNA signatures distinguished tumors from normal cerebellar tissues. Most microRNAs displayed overall downregulated expression in MB, which rescued expression promotes MB cell growth arrest and apoptosis while targeting the proproliferative t-TrkC isoform, suggesting a tumor growth–inhibitory function [11]. Therefore, microRNA-125a could represent a potential target for targeted therapy, a feature observed in clinical trials in different tumors [13, 36, 37].
Non-WNT/non-SHH molecular group which includes group 3 and group 4 remains the genetically most heterogeneous and least understood fraction of MB cases [38]. In contrast to the WNT and SHH groups, no single somatically mutated gene is present in more than 5–10% of either group 3 or group 4, constituting a significant challenge in the development of innovative treatment strategies for these groups [8]. The significantly lower levels of microRNA-125a in the non-WNT/non-SHH group provide a chance for targeted therapy aiming at increasing the levels of microRNA-125a in these patients.
In the current study, the cases with lower levels of microRNA-125a had lower 5-year OS than the cases with higher levels, and possibly, these cases will have poor outcome, but the difference was not statistically significant. This could be explained by the fact that it acts as tumor suppressor gene and is consistent with the reported poor survival rates of reduced levels of microRNA-125a in different tumors [39, 40].
In the present study, whether microRNA-125a expression could be helpful in segregating patients with poor outcome within both risk groups was assessed. Although standard-risk patients with lower expression levels have lower 5-year OS 58% versus 90% for patients with higher expression levels, the difference was not significant. The effect of stratifying patients based on microRNA-125a expression within each molecular group was also examined and showed that patients with lower levels had lower 5-year OS in non-WNT/non-SHH molecular group. This was not the case in SHH molecular group. These differences were not significant. The current study suggests that microRNA-125a might be helpful in predicting patients’ outcome; although the differences in survival rates in the present work were not statistically significant which can be explained by the small sample size, the findings are promising in this context and need to be validated in larger groups.
Conclusion
MicroRNA-125a expression was significantly lower in categories of pediatric MB patients with worse prognosis namely LC/A histology and non-WNT/non-SHH molecular group suggesting a pathogenetic role. MicroRNA-125a expression could represent a promising prognostic factor and a potential therapeutic target in non-WNT/non-SHH molecular group which represents the most common and the most heterogeneous group of pediatric MBs coupled with the highest rates of disseminated disease. Preoperative tumor size represents an independent prognostic factor.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS (2018) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro Oncol 20(suppl_4):iv1-iv86. https://doi.org/10.1093/neuonc/noy131
Smoll NR, Drummond KJ (2012) The incidence of medulloblastomas and primitive neurectodermal tumours in adults and children. J Clin Neurosci 19(11):1541–1544. https://doi.org/10.1016/j.jocn.2012.04.009
Thompson MC, Fuller C, Hogg TL et al (2006) Genomics identifies medulloblastoma subgroups that are enriched for specific genetic alterations. J Clin Oncol 24(12):1924–1931. https://doi.org/10.1200/jco.2005.04.4974
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6):803–820. https://doi.org/10.1007/s00401-016-1545-1
Louis DN, Perry A, Wesseling P et al (2021) The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol 23(8):1231–1251. https://doi.org/10.1093/neuonc/noab106
Martin AM, Raabe E, Eberhart C, Cohen KJ (2014) Management of pediatric and adult patients with medulloblastoma. Curr Treat Options Oncol 15(4):581–594. https://doi.org/10.1007/s11864-014-0306-4
Szalontay L, Khakoo Y (2020) Medulloblastoma: an old diagnosis with new promises. Curr Oncol Rep 22(9):90. https://doi.org/10.1007/s11912-020-00953-4
Northcott PA, Buchhalter I, Morrissy AS et al (2017) The whole-genome landscape of medulloblastoma subtypes. Nature 547(7663):311–317. https://doi.org/10.1038/nature22973
Hammond SM (2006) MicroRNAs as oncogenes. Curr Opin Genet Dev 16(1):4–9. https://doi.org/10.1016/j.gde.2005.12.005
Calin GA, Croce CM (2006) MicroRNA signatures in human cancers. Nat Rev Cancer 6(11):857–866. https://doi.org/10.1038/nrc1997
Ferretti E, De Smaele E, Po A et al (2009) MicroRNA profiling in human medulloblastoma. Int J Cancer 124(3):568–577. https://doi.org/10.1002/ijc.23948
Potenza N, Panella M, Castiello F, Mosca N, Amendola E, Russo A (2017) Molecular mechanisms governing microRNA-125a expression in human hepatocellular carcinoma cells. Sci Rep 7(1):10712. https://doi.org/10.1038/s41598-017-11418-3
Nishida N, Mimori K, Fabbri M et al (2011) MicroRNA-125a-5p is an independent prognostic factor in gastric cancer and inhibits the proliferation of human gastric cancer cells in combination with trastuzumab. Clin Cancer Res 17(9):2725–2733. https://doi.org/10.1158/1078-0432.Ccr-10-2132
Kuehl J, Beck J, Bode U (1995) Delayed radiation therapy after postoperative chemotherapy in children less than 3 years of age with medulloblastoma. Results of the trial HiT-SKK’87, and preliminary results of the pilot trial HiT-SKK’92. Med Pediatr Oncol 25(Suppl):250
Packer RJ, Goldwein J, Nicholson HS et al (1999) Treatment of children with medulloblastomas with reduced-dose craniospinal radiation therapy and adjuvant chemotherapy: a Children’s Cancer Group study. J Clin Oncol 17(7):2127–2136. https://doi.org/10.1200/jco.1999.17.7.2127
Packer RJ, Gajjar A, Vezina G et al (2006) Phase III study of craniospinal radiation therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. J Clin Oncol 24(25):4202–4208. https://doi.org/10.1200/jco.2006.06.4980
Taylor RE, Bailey CC, Robinson K et al (2003) Results of a randomized study of preradiation chemotherapy versus radiotherapy alone for nonmetastatic medulloblastoma: The International Society of Paediatric Oncology/United Kingdom Children’s Cancer Study Group PNET-3 Study. J Clin Oncol 21(8):1581–1591. https://doi.org/10.1200/jco.2003.05.116
Ellison DW, Dalton J, Kocak M et al (2011) Medulloblastoma: clinicopathological correlates of SHH, WNT, and non-SHH/WNT molecular subgroups. Acta Neuropathol 121(3):381–396. https://doi.org/10.1007/s00401-011-0800-8
Goschzik T, Zur Mühlen A, Kristiansen G et al (2015) Molecular stratification of medulloblastoma: comparison of histological and genetic methods to detect Wnt activated tumours. Neuropathol Appl Neurobiol 41(2):135–144. https://doi.org/10.1111/nan.12161
Kaur K, Kakkar A, Kumar A et al (2016) Integrating molecular subclassification of medulloblastomas into routine clinical practice: a simplified approach. Brain Pathol 26(3):334–343. https://doi.org/10.1111/bpa.12293
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 3(6):1101–1108. https://doi.org/10.1038/nprot.2008.73
Masuadi E, Mohamud M, Almutairi M, Alsunaidi A, Alswayed AK, Aldhafeeri OF (2021) Trends in the usage of statistical software and their associated study designs in health sciences research: a bibliometric analysis. Cureus 13(1):e12639–e12639. https://doi.org/10.7759/cureus.12639
Ramaswamy V, Remke M, Bouffet E et al (2016) Risk stratification of childhood medulloblastoma in the molecular era: the current consensus. Acta Neuropathol 131(6):821–831. https://doi.org/10.1007/s00401-016-1569-6
Schwalbe EC, Lindsey JC, Nakjang S et al (2017) Novel molecular subgroups for clinical classification and outcome prediction in childhood medulloblastoma: a cohort study. Lancet Oncol 18(7):958–971. https://doi.org/10.1016/s1470-2045(17)30243-7
Thomas A, Noël G (2019) Medulloblastoma: optimizing care with a multidisciplinary approach. J Multidiscip Healthc 12:335–347. https://doi.org/10.2147/jmdh.S167808
Sedano P, Segundo CG, De Ingunza L et al (2021) Real-world data for pediatric medulloblastoma: can we improve outcomes? Eur J Pediatr 180(1):127–136. https://doi.org/10.1007/s00431-020-03722-4
Zeltzer PM, Boyett JM, Finlay JL et al (1999) Metastasis stage, adjuvant treatment, and residual tumor are prognostic factors for medulloblastoma in children: conclusions from the Children’s Cancer Group 921 randomized phase III study. J Clin Oncol 17(3):832–845. https://doi.org/10.1200/jco.1999.17.3.832
Evans AE, Jenkin RD, Sposto R et al (1990) The treatment of medulloblastoma. Results of a prospective randomized trial of radiation therapy with and without CCNU, vincristine, and prednisone. J Neurosurg 72(4):572–82. https://doi.org/10.3171/jns.1990.72.4.0572
Peng Y, Croce CM (2016) The role of MicroRNAs in human cancer. Signal Transduct Target Ther 1:15004. https://doi.org/10.1038/sigtrans.2015.4
Huang PI, Lin SC, Lee YY et al (2017) Large cell/anaplastic medulloblastoma is associated with poor prognosis-a retrospective analysis at a single institute. Childs Nerv Syst 33(8):1285–1294. https://doi.org/10.1007/s00381-017-3435-9
Robinson GW, Rudneva VA, Buchhalter I et al (2018) Risk-adapted therapy for young children with medulloblastoma (SJYC07): therapeutic and molecular outcomes from a multicentre, phase 2 trial. Lancet Oncol 19(6):768–784. https://doi.org/10.1016/s1470-2045(18)30204-3
Cho YJ, Tsherniak A, Tamayo P et al (2011) Integrative genomic analysis of medulloblastoma identifies a molecular subgroup that drives poor clinical outcome. J Clin Oncol 29(11):1424–1430. https://doi.org/10.1200/jco.2010.28.5148
Potenza N, Russo A (2013) Biogenesis, evolution and functional targets of microRNA-125a. Mol Genet Genomics 288(9):381–389. https://doi.org/10.1007/s00438-013-0757-5
Laneve P, Di Marcotullio L, Gioia U et al (2007) The interplay between microRNAs and the neurotrophin receptor tropomyosin-related kinase C controls proliferation of human neuroblastoma cells. Proc Natl Acad Sci U S A 104(19):7957–7962. https://doi.org/10.1073/pnas.0700071104
Cortez MA, Nicoloso MS, Shimizu M et al (2010) miR-29b and miR-125a regulate podoplanin and suppress invasion in glioblastoma. Genes Chromosomes Cancer 49(11):981–990. https://doi.org/10.1002/gcc.20808
Hsieh TH, Hsu CY, Tsai CF et al (2015) HDAC inhibitors target HDAC5, upregulate microRNA-125a-5p, and induce apoptosis in breast cancer cells. Mol Ther 23(4):656–666. https://doi.org/10.1038/mt.2014.247
Jiang L, Huang Q, Chang J, Wang E, Qiu X (2011) MicroRNA HSA-miR-125a-5p induces apoptosis by activating p53 in lung cancer cells. Exp Lung Res 37(7):387–398. https://doi.org/10.3109/01902148.2010.492068
Archer TC, Ehrenberger T, Mundt F et al (2018) Proteomics, post-translational modifications, and integrative analyses reveal molecular heterogeneity within medulloblastoma subgroups. Cancer Cell 34(3):396-410.e8. https://doi.org/10.1016/j.ccell.2018.08.004
Li G, Ao S, Hou J, Lyu G (2019) Low expression of miR-125a-5p is associated with poor prognosis in patients with gastric cancer. Oncol Lett 18(2):1483–1490. https://doi.org/10.3892/ol.2019.10423
Lu G, Ma Y, Jia C et al (2017) Reduced miR-125a levels associated with poor survival of patients with hepatocellular cancer. Oncol Lett 14(5):5952–5958. https://doi.org/10.3892/ol.2017.6902
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Collection of study material was performed by Soheir M. Hamam, Eman Abdelzaher, and Hend A. Sharafeldin. Collection and revision of clinical data of the patients were performed by Shady H. Fadel and Hend A. Sharafeldin. IHC was performed by Hend A. Sharafeldin. PCR was performed by Rasha A. Nassra and Hend A. Sharafeldin. IHC and molecular studies were supervised by Soheir M. Hamam and Eman Abdelzaher. All authors contributed to acquisition, analysis, and interpretation of data. Drafting the work was performed by Soheir M. Hamam, Eman Abdelzaher, and Hend A. Sharafeldin. The work was critically revised by Soheir M. Hamam, Eman Abdelzaher, Shady H. Fadel, and Rasha A. Nassra. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Methodology for this study was approved by the Ethics committee of Faculty of Medicine, Alexandria University, IRB NO. 00012098, FWA NO. 00018699, (Ethics approval number: 0201228).
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hamam, S.M., Abdelzaher, E., Fadel, S.H. et al. Prognostic value of microRNA-125a expression status in molecular groups of pediatric medulloblastoma. Childs Nerv Syst 39, 1869–1880 (2023). https://doi.org/10.1007/s00381-023-05899-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-05899-z