Abstract
Purpose
This study aimed to develop a nomogram prediction model to predict the exact probability of urinary infection stones before surgery in order to better deal with the clinical problems caused by infection stones and take effective treatment measures.
Methods
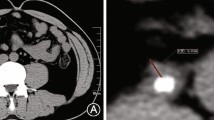
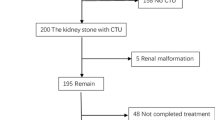
We retrospectively collected the clinical data of 390 patients who were diagnosed with urinary calculi by imaging examination and underwent postoperative stone analysis between August 2018 and August 2023. The patients were randomly divided into training group (n = 312) and validation group (n = 78) using the "caret" R package. The clinical data of the patients were evaluated. Univariate and multivariate logistic regression analysis were used to screen out the independent influencing factors and construct a nomogram prediction model. The receiver operating characteristic curve (ROC), calibration curves, and decision curve analysis (DCA) and clinical impact curves were used to evaluate the discrimination, accuracy, and clinical application efficacy of the prediction model.
Results
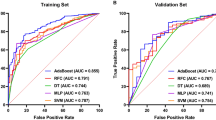
Gender, recurrence stones, blood uric acid value, urine pH, and urine bacterial culture (P < 0.05) were independent predictors of infection stones, and a nomogram prediction model (https://zhaoyshenjh.shinyapps.io/DynNomInfectionStone/) was constructed using these five parameters. The area under the ROC curve of the training group was 0.901, 95% confidence interval (CI) (0.865–0.936), and the area under the ROC curve of the validation group was 0.960, 95% CI (0.921–0.998). The results of the calibration curve for the training group showed a mean absolute error of 0.015 and the Hosmer–Lemeshow test P > 0.05. DCA and clinical impact curves showed that when the threshold probability value of the model was between 0.01 and 0.85, it had the maximum net clinical benefit.
Conclusions
The nomogram developed in this study has good clinical predictive value and clinical application efficiency can help with risk assessment and decision-making for infection stones in diagnosing and treating urolithiasis.




Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under curve
- CI:
-
Confidence interval
- DCA:
-
Decision curve analysis
- CT:
-
Computed tomography
- PCNL:
-
Percutaneous nephrolithotomy
- LPNL:
-
Laparoscopic nephrolithotomy
- URSL:
-
Ureteroscopic lithotripsy
- LUL:
-
Laparoscopic ureterolithotomy
- ESWL:
-
Extracorporeal shockwave lithotripsy
- OR:
-
Odds ratio
- BMI:
-
Body mass index
- D-J:
-
Double J
- WBC:
-
White blood cell
References
Zhang D, Li S, Zhang Z et al (2021) Urinary stone composition analysis and clinical characterization of 1520 patients in central China. Sci Rep 11(1):6467. https://doi.org/10.1038/s41598-021-85723-3
Espinosa-Ortiz EJ, Eisner BH, Lange D et al (2019) Current insights into the mechanisms and management of infection stones. Nat Rev Urol 16(1):35–53. https://doi.org/10.1038/s41585-018-0120-z
Rahman NU, Meng MV, Stoller ML (2003) Infections and urinary stone disease. Curr Pharm Des 9(12):975–981. https://doi.org/10.2174/1381612033455125
Gao X, Lu C, Xie F et al (2020) Risk factors for sepsis in patients with struvite stones following percutaneous nephrolithotomy. World J Urol 38(1):219–229. https://doi.org/10.1007/s00345-019-02748-0
Koras O, Bozkurt IH, Yonguc T et al (2015) Risk factors for postoperative infectious complications following percutaneous nephrolithotomy: a prospective clinical study. Urolithiasis 43(1):55–60. https://doi.org/10.1007/s00240-014-0730-8
Qin L, Zhou J, Hu W et al (2022) The combination of mean and maximum Hounsfield Unit allows more accurate prediction of uric acid stones. Urolithiasis 50(5):589–597. https://doi.org/10.1007/s00240-022-01333-2
Marchini GS, Gebreselassie S, Liu X et al (2013) Absolute Hounsfield unit measurement on noncontrast computed tomography cannot accurately predict struvite stone composition. J Endourol 27(2):162–167. https://doi.org/10.1089/end.2012.0470
Popiolek M, Jendeberg J, Sundqvist P et al (2023) Finding the optimal candidate for shock wave lithotripsy: external validation and comparison of five prediction models. Urolithiasis 51(1):66. https://doi.org/10.1007/s00240-023-01444-4
Ito H, Sakamaki K, Kawahara T et al (2015) Development and internal validation of a nomogram for predicting stone-free status after flexible ureteroscopy for renal stones. BJU Int 115(3):446–451. https://doi.org/10.1111/bju.12775
Xia K, Xu Y, Qi Q et al (2023) Establishment of a new predictive model for the recurrence of upper urinary tract stones. Int Urol Nephrol 55(10):2411–2420. https://doi.org/10.1007/s11255-023-03698-8
Ruhayel Y, Tepeler A, Dabestani S et al (2017) Tract sizes in miniaturized percutaneous nephrolithotomy: a systematic review from the European Association of Urology Urolithiasis Guidelines Panel. Eur Urol 72(2):220–235. https://doi.org/10.1016/j.eururo.2017.01.046
Mcaleer IM, Kaplan GW, Bradley JS et al (2003) Endotoxin content in renal calculi. J Urol 169(5):1813–1814. https://doi.org/10.1097/01.ju.0000061965.51478.79
Popovtzer B, Khusid JA, Bamberger JN et al (2022) Do infection-associated stone subtypes behave the same clinically? A retrospective bicenter study. J Endourol 36(5):688–693. https://doi.org/10.1089/end.2021.0460
Chen T, Zhang Y, Dou Q et al (2022) Machine learning-assisted preoperative diagnosis of infection stones in urolithiasis patients. J Endourol 36(8):1091–1098. https://doi.org/10.1089/end.2021.0783
D’costa MR, Pais VM, Rule AD (2019) Leave no stone unturned: defining recurrence in kidney stone formers. Curr Opin Nephrol Hypertens 28(2):148–153. https://doi.org/10.1097/mnh.0000000000000478
Zhu C, Wang DQ, Zi H et al (2021) Epidemiological trends of urinary tract infections, urolithiasis and benign prostatic hyperplasia in 203 countries and territories from 1990 to 2019. Military Med Res 8(1):64. https://doi.org/10.1186/s40779-021-00359-8
Ye Z, Zeng G, Yang H et al (2020) The status and characteristics of urinary stone composition in China. BJU Int 125(6):801–809. https://doi.org/10.1111/bju.14765
Anderson GG, Palermo JJ, Schilling JD et al (2003) Intracellular bacterial biofilm-like pods in urinary tract infections. Science 301(5629):105–107. https://doi.org/10.1126/science.1084550
Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284(5418):1318–1322. https://doi.org/10.1126/science.284.5418.1318
Halinski A, Bhatti KH, Boeri L et al (2022) Spectrum of bacterial pathogens from urinary infections associated with struvite and metabolic stones. Diagnostics (Basel) 13(1):80
Arkusz K, Pasik K, Halinski A et al (2021) Surface analysis of ureteral stent before and after implantation in the bodies of child patients. Urolithiasis 49(1):83–92. https://doi.org/10.1007/s00240-020-01211-9
Hobbs T, Schultz LN, Lauchnor EG et al (2018) Evaluation of biofilm induced urinary infection stone formation in a novel laboratory model system. J Urol 199(1):178–185. https://doi.org/10.1016/j.juro.2017.08.083
Carpentier X, Daudon M, Traxer O et al (2009) Relationships between carbonation rate of carbapatite and morphologic characteristics of calcium phosphate stones and etiology. Urology 73(5):968–975. https://doi.org/10.1016/j.urology.2008.12.049
Das P, Gupta G, Velu V et al (2017) Formation of struvite urinary stones and approaches towards the inhibition—a review. Biomed Pharmacother 96:361–370. https://doi.org/10.1016/j.biopha.2017.10.015
Ariyanto E, Sen T, Ang H (2014) The influence of various physico-chemical process parameters on kinetics and growth mechanism of struvite crystallisation. Adv Powder Technol 25(2):682–694. https://doi.org/10.1016/j.apt.2013.10.014
Wen W, Li Y, Chen Q et al (2022) Serum and urine uric acid level may have different predictive value for urinary stone composition: a retrospective cohort study of 718 patients in Chinese population. Int Urol Nephrol 54(9):2247–2254. https://doi.org/10.1007/s11255-022-03121-8
Bichler KH, Eipper E, Naber K et al (2002) Urinary infection stones. Int J Antimicrob Agents 19(6):488–498. https://doi.org/10.1016/s0924-8579(02)00088-2
Parkhomenko E, De Fazio A, Tran T et al (2017) A multi-institutional study of struvite stones: patterns of infection and colonization. J Endourol 31(5):533–537. https://doi.org/10.1089/end.2016.0885
Paonessa JE, Gnessin E, Bhojani N et al (2016) Preoperative bladder urine culture as a predictor of intraoperative stone culture results: clinical implications and relationship to stone composition. J Urol 196(3):769–774. https://doi.org/10.1016/j.juro.2016.03.148
Liu M, Cui Z, Zhu Z et al (2022) Development of a nomogram predicting the infection stones in kidney for better clinical management: a retrospective study. J Endourol 36(7):947–953. https://doi.org/10.1089/end.2021.0735
Acknowledgements
This study was supported by the Xuzhou Key Research and Development Project (No. KC22152).
Author information
Authors and Affiliations
Contributions
SJH contributed to paper design, data analysis, and draft of manuscript. XZL was involved in data collection and management. WXT collected data. ZY performed revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing interests exist.
Ethics approval
All data analysis was carried out in accordance with applicable laws and regulations described in the Declaration of Helsinki and approved by Medical Ethics Committee of Xuzhou Central Hospital approval, reference number: XZXY-LK-20230801-0129. This study is a retrospective study, all data are anonymous, and formal consent is not required with the consent of the Medical Ethics Committee of Xuzhou Central Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, J., Xiao, Z., Wang, X. et al. A nomogram clinical prediction model for predicting urinary infection stones: development and validation in a retrospective study. World J Urol 42, 211 (2024). https://doi.org/10.1007/s00345-024-04904-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04904-7