Abstract
We aimed to externally validate five previously published predictive models (Ng score, Triple D score, S3HoCKwave score, Kim nomogram, Niwa nomogram) for shock wave lithotripsy (SWL) single-session outcomes in patients with a solitary stone in the upper ureter. The validation cohort included patients treated with SWL from September 2011 to December 2019 at our institution. Patient-related variables were retrospectively collected from the hospital records. Stone-related data including all measurements were retrieved from computed tomography prior to SWL. We estimated discrimination using area under the curve (AUC), calibration, and clinical net benefit based on decision curve analysis (DCA). A total of 384 patients with proximal ureter stones treated with SWL were included in the analysis. Median age was 55.5 years, and 282 (73%) of the sample were men. Median stone length was 8.0 mm. All models significantly predicted the SWL outcomes after one session. S3HoCKwave score, Niwa, and Kim nomograms had the highest accuracy in predicting outcomes, with AUC 0.716, 0.714 and 0.701, respectively. These three models outperformed both the Ng (AUC: 0.670) and Triple D (AUC: 0.667) scoring systems, approaching statistical significance (P = 0.05). Of all the models, the Niwa nomogram showed the strongest calibration and highest net benefit in DCA. To conclude, the models showed small differences in predictive power. The Niwa nomogram, however, demonstrated acceptable discrimination, the most accurate calibration, and the highest net benefit whilst having relatively simple design. Therefore, it could be useful for counselling patients with a solitary stone in the upper ureter.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With an incidence of 5–13% worldwide, urolithiasis is a rising global concern and a significant burden for healthcare systems [1, 2]. Epidemiological data have shown upward trends in both the prevalence of and interventions for kidney stone disease [3, 4]. Most ureteral stones (75–90%) pass spontaneously with no need for intervention and low morbidity [5]. Thus, majority of ureteral stones can be managed conservatively if there are no indications for active removal such as persistent pain, obstruction, or kidney failure [6]. However, stones in the upper ureter have a lower likelihood of spontaneous passage (22–48%) than those in other locations [7, 8] and their management may be especially challenging if they become impacted.
The European Association of Urology (EAU) considers both shock wave lithotripsy (SWL) and ureteroscopy (URS) first-line treatment options yielding similar outcomes for ureteral stones under 10 mm [6].
Although SWL is less invasive than URS and unlike other treatment modalities does not require general anaesthesia, a wide range of factors described in the literature may influence its efficacy [9]. Factors affecting SWL outcomes include stone size measured as one-dimensional stone length or stone volume, location, density, and skin-to-stone distance (SSD) [10,11,12,13,14]. Furthermore, parameters measured on computed tomography (CT) scans indicating an impacted ureteral stone also seem to be valuable predictors of SWL failure [15, 16].
Proximal ureteral stones often pose a challenge for the clinician to choose the most suitable treatment option. Since patient selection is key to successful SWL, numerous attempts have been made to develop a reliable predicting scoring model or nomogram to enhance clinical decision-making [17,18,19,20,21]. Although several predictive models are available, a solid ground for decision-making is still missing. A comparative external validation of the models may provide that missing ground.
The aim of this study was therefore to externally validate and compare the predictive scoring models and nomograms available in the literature and to evaluate their performances in terms of discrimination, calibration, and clinical usefulness in predicting SWL outcomes after one session.
Material and methods
Patient population (validation cohort)
Ethical approval was obtained from the Swedish Ethical Review Authority (2019-04689). We conducted a retrospective review of all 1383 consecutive patients treated with SWL in Örebro University Hospital in Sweden from September 2011 to December 2019. Exclusion criteria and numbers are shown in the flowchart (Fig. 1). Of the total sample, 384 were eligible for inclusion in the study. Patient characteristics are presented in Table 1.
Patient data
Clinical data such as age, sex, number of SWL sessions, and treatment outcomes were collected from patients’ medical records. Stone-related data were obtained from CT scans using the integrated PACS measurement tool (Sectra IDS7, Linköping, Sweden).
CT scans and measurement methodology
All patients were examined with CT before SWL. Typically, a low-dose unenhanced protocol for urinary tract stones was followed using similar settings (120 kV, CTDI 2–5 mGy). Axial, coronal, and sagittal reformations (3 or 5 mm) were generated. The same experienced urologist (MP) performed all measurements under supervision and in consensus with expert radiologists (ML, JJ). The reader was not aware of SWL outcomes at the time of measurements.
All measurements were performed in a standardized soft-tissue window (C50, W400) with selected zoom level (pixel-to-pixel × 6–8). A special care was devoted to measurements of attenuation in small stones (stone length < 5 mm) as obtaining precise values is not always straightforward in these cases. To increase accuracy, we took several measurements on different CT slices in high zoom level and, if necessary, a bone window (C400, W1500) was used to assess stone structure and identify areas with highest attenuation. The largest diameter of the stone was obtained in all reformations (axial, coronal, and sagittal) and the longest was defined as the stone length. The measurements were reported in mm to one decimal place. The stone volume was estimated with the ellipsoid formula using stone diameters in three axes measured on coronal and axial reformations [22]. SSD was measured on axial reformation dorsally from the centre of the stone to the skin in both vertical (SSD 90°) and oblique (SSD 45°) directions. The presence of hydronephrosis was graded 0–4 (0 = none, 1 = mild, 2 = moderate, 3 = pronounced, 4 = massive) [23]. Proximal ureter was defined as the segment between the ureteropelvic junction and the level of ureter projecting over the upper border of the sacroiliac joint.
Shock wave lithotripsy
SWL was performed using Siemens Lithostar Modularis (Siemens AG, Erlangen, Germany) under fluoroscopic control. The patient received suppository diclofenac 100 mg prior to treatment. During the procedure, a combination of intravenous alfentanil and propolipid was administered intermittently in small doses to provide analgesia and sedation. According to the local protocol, stones in the ureter within the level of the kidney parenchyma were treated with a maximum energy of 4 kV and 4000 shockwaves. Stones below the parenchyma were treated with maximal energy of 6 kV and 2500 shockwaves. A frequency of 60 shock waves per minute (1 Hz) was used in all cases. All patients were treated in supine position with the shock wave head placed obliquely underneath the table. Treatment outcome was evaluated with follow-up imaging (kidney, ureter, and bladder radiograph [n = 22], antegrade pyelogram [n = 10], intravenous urography [n = 68], and CT [n = 284]) at 2 to 6 weeks depending on the presumed results of the first session. Stone-free status was defined as no stones in the ureter (zero residuals) on follow-up examination.
Predictive models
We performed a literature search for nomograms and scoring systems predicting SWL outcomes based on information from CT after one session in patients with proximal ureteral stones. Five predictive models that fulfilled these criteria (Ng score, Triple D score, S3HoCKwave score, Niwa nomogram, Kim nomogram) were included in the study for external validation [17,18,19,20,21]. The variables included in each model are summarized in Table 2.
Sample size calculation
Steyerberg et al. recommended as a rule of thumb at least 100 events and 100 non-events in an external sample to achieve a reasonable power for statistical analysis to validate a prediction model [24]. According to the results of an internal audit at our institution, the success rates in proximal ureteral stones after one SWL session ranged from 50 to 70%. Based on these numbers, we estimated that the validation cohort should include 200 to 350 study subjects.
Statistics
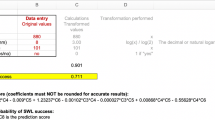
The statistical analysis was performed using IBM SPSS v27.0.1.0 (SPSS Inc., Chicago, IL, USA) and Stata MP 17.0 (StataCorp, Texas, USA). The parameters in our study were analysed using absolute and relative frequencies for quantitative variables. Continuous variables are reported as mean and standard deviation (SD) or median and interquartile range (IQR). Pearson’s chi-square or Fisher exact test was used to verify associations between quantitative variables. Between-group comparisons for qualitative variables were performed using student T test or Mann–Whitney U test. To calculate the predicted probability of successful SWL, we used the beta-coefficients from regression models provided by the authors (Niwa nomogram, Kim nomogram, and S3HoCKwave scores). We used published estimates to validate Triple D and Ng scores and performed the validation process following TRIPOD’s recommended steps [25].
To assess the discrimination capability of the models, we calculated and compared the areas under the curves (AUC) of the receiver operator characteristics (ROC). Calibration was assessed by visual representation of the relationship between the predicted and observed values using a flexible curve on calibration plots. Additional calibration measures such as intercept and slope were also included. Calibration intercept is an assessment of calibration-in-the-large (CITL) and has a target value of zero [26]. Values below zero suggest overestimation; those over zero suggest underestimation. Calibration slope is a measure of the spread of an estimate and has a target value of 1. When CITL is close to zero, a slope close to 1 indicates good calibration across all subgroups. Decision curve analysis (DCA) was performed to estimate the net benefit of the models with regard to different clinically relevant thresholds [27]. A two-sided P < 0.05 was considered statistically significant.
Results
Validation cohort
Baseline patient and stone characteristics for the validation cohort are summarized in Table 2. Median age was 55.5 years (IQR: 45–68) and 282 (73%) were males. Median stone length was 8.0 mm (IQR: 6.4–9.9), and median estimated volume was 138 mm3 (IQR: 82–225). Mean average and maximal CT attenuation were 952 ± 255 HU and 1213 ± 288 HU, respectively. Mean SSD was 13.0 ± 1.9 cm at 90 degrees and 13.9 ± 2.0 cm at 45 degrees. Stone-free status was achieved in 228 (59%) patients after one session and in 298 (78%) after all sessions (range 1–4, mean 1.36). Overall, approximately 30% had hydronephrosis grade 2–4. A comparison of the successfully treated group and patients with failed SWL outcome is presented in Table 1.
Discrimination
The discriminatory capacity of the model is visually presented on ROC plots (Fig. 2). All the models significantly predicted the SWL outcomes after one session. S3HoCKwave score, Niwa and Kim nomogram had highest accuracy for prediction of successful outcome with AUC 0.716 (95% CI 0.664–0.769), 0.714 (95% CI 0.661–0.766) and 0.701 (95% CI 0.648–0.755), respectively. These three models outperformed Ng (AUC: 0.670; 95% CI 0.614–0.726) and Triple D (AUC: 0.667; 95% CI 0.612–0.721) scoring systems’ discrimination power. Sensitivity, specificity and accuracy for probability threshold of 50% are presented in Table 3.The pairwise differences between the Ng score or Triple D score and S3oCKwave score, Niwa nomogram, Kim nomogram were statistically significant (P < 0.05). However, there was no significant difference between and S3oCKwave score, Niwa nomogram and Kim nomogram (P = 0.64).
Calibration
Calibration plots including key measures are presented in Fig. 3. Of all models, Ng score and Triple D score showed the weakest overall calibration with CITLs of 0.774 and 0.893, respectively. Both S3HoCKwave score and Kim nomogram had CITLs above zero (0.349 and 0.183), indicating slight systematic underestimation of these models’ predictions. The Niwa nomogram showed the strongest calibration of all models, with a CITL close to zero (0.024). However, the calibration slope for this model was 0.879, suggesting it had weaker calibration in some subgroups.
Decision curve analysis (DCA): net benefit
In the DCA, Ng scores and Triple D scores showed no net benefit as their decision curves oscillated close to the “treat all strategy” curve (Fig. 4). In contrast, S3HoCKwave score and both Kim and Niwa nomograms provided a net benefit, over treating all patients or none of them. Of these three, the Niwa nomogram showed the highest net benefit over the widest range of thresholds (20–80%).
Discussion
In this study, we compared the performance of five prediction models for SWL outcomes after one session in an independent retrospective cohort. The models showed moderate predictive capacity. There were small, but statistically significant, differences in discriminative AUC, calibration, and net benefit according to DCA. In our cohort, Ng score and Triple D score showed slightly lower discrimination (AUC 0.660 and 0.667, respectively) and poorer calibration, making them less useful in clinical praxis.
Yoshioka et al. tested the Triple D score performance and found that the AUC for this model in their cohort was 0.68, which was strikingly similar to AUC for this model in our study (0.67) but differed greatly from that reported in the original paper (0.78). Although S3HoCKwave score, Kim nomogram, and Niwa nomogram performed slightly better in terms of discrimination, the AUCs for these models were only moderate. There was no significant difference between these three latter models (P = 0.64). Kim nomogram and S3HoCKwave score also demonstrated some miscalibration, which diminished their net benefit. Niwa nomogram, however, showed adequate calibration and the highest net benefit. In addition, it includes fewer parameters than S3HoCKwave score or Kim nomogram. Furthermore, maximum stone attenuation and vertical SSD used in this model are easier to obtain than mean stone attenuation and oblique SSD and are less dependent on the reader.
Recent improvements in ureteroscopy such as new laser technologies and new ureteroscopes with high quality vision have led over the last decade to a rapid increase in its popularity over that of SWL treatment [28]. Yet, SWL is still a viable treatment option for upper urinary tract stones [29]. Proximal ureteral stones may be challenging to manage if they become impacted. According to EAU Urolithiasis Guidelines, stones with a low likelihood of spontaneous passage should be considered for early intervention. However, the panel concludes that no exact cut-off values for stone size can be provided due to a lack of evidence. EAU guidelines recommend either SWL or URS to manage proximal ureteral stones sized < 10 mm, but favour neither over the other [6] and which is preferable remains controversial. A recently published RCT found that SWL for ureteric stones is the more cost-effective option but requires more treatments than URS and results in a lower quality of life [30]. According to Cone et al., a stone-free rate of at least 60% after one session should be achieved with SWL to consider it a cost-effective treatment compared with URS. This implies the necessity of adequate patient selection for SWL to be the most cost-effective overall.
Non-contrast CT is frequently used prior to SWL to assess the patient and stone-related factors influencing stone-free rate [31]. Several reports show that factors such as stone size, stone CT attenuation, and SSD are strong predictors of various SWL outcomes. Longest diameter of the stone is a proxy parameter of stone burden. Choi et al. found that stone size was an independent predictive factor influencing the outcomes of SWL [14]. In a study by Wagenius et al., stone size and age were found to be independent predictive factors for SWL failure [12]. Ng et al. observed that SSD measured vertically in patients with stones in the upper ureter had a significant predictive value for SWL outcomes [18]. Stone CT attenuation is one of the most cited predictive factors. Ouzaid et al. found that SFR dropped from 96 to 38% for stones with mean stone attenuation of ≥ 970 HU [13]. In contrast, Niwa et al. demonstrated that maximum CT attenuation value was a more significant predictor than mean attenuation [19]. None of these factors alone, however, is powerful enough to base a clinical decision on, as the SWL result is the product of a complex process with multifactorial interactions. Thus, predictive tools, such as nomograms and scoring systems, combining different predictors, have been developed to facilitate clinical decision-making and avoid unnecessary procedures.
To our knowledge, this is the first study to externally validate and compare several predictive models for SWL outcomes in proximal ureteral stones. According to our findings, the Niwa nomogram seems to be the most beneficial of all validated models and therefore may be considered an interesting candidate for use in decision-making with patients with solitary calculi in the upper ureter. However, given that the discrimination accuracy was only slightly above 0.7 (AUC), there is still room for improvement. Recently, Bulbul et al. showed that increased ureteral wall thickness on the CT scans was an independent predictive factor for SWL failure [15]. It is likely that including ureteral wall thickness into predictive models, as a measure of potential stone impaction, may increase the models’ discrimination power.
Our study has some limitations. Its retrospective methodology increases the risk of misclassification and selection bias and reflects only those patients already selected for SWL at the study site. Moreover, not all consecutive patients managed at our institution with proximal ureteral stones, suitable for active treatment, underwent SWL because stones > 10 mm were preferably treated with URS in line with EAU Urolithiasis Guidelines. The patients underwent CT on several different scanners with slightly different protocols, which may have had an impact on the measurements and presents another risk of possibly skewed results. However, this variation in scanners may also reflect real-world better than strictly controlled data. A multicentre study would also increase the generalizability of the results of this single-centre study. Nonetheless, all the treatments were executed with methodological consistency according to the local protocols for shock wave rate, energy, and sedation/analgesia regime, which improves the validity of this study. Lastly, although all measurements were performed by only one reader, which increases the risk of systematic error, they were done under supervision and according to the methodology described in detail in the study protocol.
Conclusions
In our cohort, although there were small differences, the Niwa nomogram showed acceptable discrimination compared with the other methods, the most accurate calibration, and the highest net benefit with a relatively simple design. It could therefore be useful in counselling patients with a solitary stone in the upper ureter during the decision-making process. Recalibration of other models could be considered in future studies to increase their accuracy and clinical usefulness.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to current data protection legislation, but are available from the corresponding author on reasonable request, if appropriate permits are obtained from adequate authorities.
References
Scales CD Jr (2014) Comparative effectiveness of shock wave lithotripsy and ureteroscopy for treating patients with kidney stones. JAMA Surg 149:648–653
Saigal CS, Joyce G, Timilsina AR, Urologic Diseases in America Project (2005) Direct and indirect costs of nephrolithiasis in an employed population: opportunity for disease management? Kidney Int 68:1808–1814
Sorokin I, Mamoulakis C, Miyazawa K, Rodgers A, Talati J, Lotan Y (2017) Epidemiology of stone disease across the world. World J Urol 35:1301–1320
Abufaraj M, Xu T, Cao C et al (2021) Prevalence and trends in kidney stone among adults in the USA: analyses of national health and nutrition examination survey 2007–2018 data. Eur Urol Focus 7:1468–1475. https://doi.org/10.1016/j.euf.2020.08.011
Sandegard E (1956) Prognosis of stone in the ureter. Acta Chir Scand Suppl 219:1–67
EAU Guidelines (2022) presented at the EAU Annual Congress Amsterdam, 2022. ISBN 978–94–92671–16–5.
Jendeberg J, Geijer H, Alshamari M, Cierzniak B, Lidén M (2017) Size matters: the width and location of a ureteral stone accurately predict the chance of spontaneous passage. Eur Radiol 27:4775–4785. https://doi.org/10.1007/s00330-017-4852-6
Coll DM, Varanelli MJ, Smith RC (2002) Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. AJR Am J Roentgenol 178:101–103. https://doi.org/10.2214/ajr.178.1.1780101
Kroczak T, Scotland KB, Chew B, Pace KT (2017) Shockwave lithotripsy: techniques for improving outcomes. World J Urol 35:1341–1346. https://doi.org/10.1007/s00345-017-2056-y
Park BH, Choi H, Kim J-B, Chang Y-S (2012) Analyzing the effect of distance from skin to stone by computed tomography scan on the extracorporeal shock wave lithotripsy stone-free rate of renal stones. Korean J Urol 53:40–43. https://doi.org/10.4111/kju.2012.53.1.40
Bandi G, Meiners RJ, Pickhardt PJ, Nakada SY (2009) Stone measurement by volumetric three-dimensional computed tomography for predicting the outcome after extracorporeal shock wave lithotripsy. BJU Int 103:524–528. https://doi.org/10.1111/j.1464-410X.2008.08069.x
Wagenius M, Oddason K, Utter M, Popiolek M, Forsvall A, Lundström KJ, Linder A (2022) Factors influencing stone-free rate of extracorporeal shock wave lithotripsy (ESWL); a cohort study. Scand J Urol 56:237–243. https://doi.org/10.1080/21681805.2022.2055137
Ouzaid I, Al-qahtani S, Dominique S et al (2012) A 970 Hounsfield units (HU) threshold of kidney stone density on non-contrast computed tomography (NCCT) improves patients’ selection for extracorporeal shockwave lithotripsy (ESWL): evidence from a prospective study. BJU Int 110(11 Pt B):E438–E442. https://doi.org/10.1111/j.1464-410X.2012.10964.x
Choi JW, Song PH, Kim HT (2012) Predictive factors of the outcome of extracorporeal shockwave lithotripsy for ureteral stones. Korean J Urol 53:424–430. https://doi.org/10.4111/kju.2012.53.6.424
Bulbul E, Ilki FY, Gultekin MH et al (2021) Ureteral wall thickness is an independent parameter affecting the success of extracorporeal shock wave lithotripsy treatment in ureteral stones above the iliac crest. Int J Clin Prac 75:e14264. https://doi.org/10.1111/ijcp.14264
Sarica K, Kafkasli A, Yazici Ö et al (2015) Ureteral wall thickness at the impacted ureteral stone site: a critical predictor for success rates after SWL. Urolithiasis 43:83–88. https://doi.org/10.1007/s00240-014-0724-6
Kim JK, Ha SB, Jeion CH et al (2016) Clinical nomograms to predict stone-free rates after shock wave lithotripsy: development and internal-validation. PLoS One 11:e0149333. https://doi.org/10.1371/journal.pone.0149333
Ng CF, Siu DY-W, Wong A, Goggins W, Chan ES, Wong K-T (2009) Development of a scoring system from noncontrast computerized tomography measurements to improve the selection of upper ureteral stone for extracorporeal shock wave lithotripsy. J Urol 181:1151–1157. https://doi.org/10.1016/j.juro.2008.10.161
Niwa N, McGillen K, Blanchard Cone E, Pareek G (2017) Simple and practical nomograms for predicting the stone-free rate after shock wave lithotripsy in patients with a solitary upper ureteral stone. World J Urol 35:1455–1461. https://doi.org/10.1089/end.2014.0212
Tran TY, McGillen K, Blanchard Cone E, Gyan Pareek J (2015) Triple D Score is a reportable predictor of shockwave lithotripsy stone-free rates. J Endourol. https://doi.org/10.1089/end.2014.0212
Yoshioka T, Ikenoue T, Hashimoto H et al (2020) Development and validation of a prediction model for failed shockwave lithotripsy of upper urinary tract calculi using computed tomography information: the S3HoCKwave score. World J Urol 38:3267–3273. https://doi.org/10.1007/s00345-020-03125-y
Finch W, Johnston R, Shaida N, Winterbottom A, Wiseman O (2014) Measuring stone volume—three-dimensional software reconstruction or an ellipsoid algebra formula? BJU Int 113:610–614. https://doi.org/10.1111/bju.12456
Beetz R, Bökenkamp A, Brandis M et al (2001) Diagnosis of congenital dilatation of the urinary tract. Consensus Group of the Pediatric Nephrology Working Society in cooperation with the Pediatric Urology Working Group of the German Society of Urology and with the Pediatric Urology Working Society in the Germany Society of Pediatric Surgery. Urologe A 40:495–507. https://doi.org/10.1007/s001200170015
Steyerberg EW (2019) Validation of prediction models. In: Steyerberg EW (ed) Clinical prediction models. Springer, pp 329–344
Collins GS, Reitsma JB, Altman DG, Moons KGM (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Eur Urol 67:1142–1151
Van Calster B, McLernon DJ, van Smeden M, Wynants L, Steyerberg EW (2019) Calibration: the Achilles heel of predictive analytics. BMC Med 17:230
Vickers AJ, Elkin EB (2006) Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making 26:565–574. https://doi.org/10.1177/0272989X06295361
Herout R, Baunacke M, Groeben C et al (2022) Contemporary treatment trends for upper urinary tract stones in a total population analysis in Germany from 2006 to 2019: will shock wave lithotripsy become extinct? World J Urol 40:185–191. https://doi.org/10.1007/s00345-021-03818-y
Juliebø-Jones P, Keller EX, Tailly T, Æsøy MS, Esperto F, Mykoniatis I et al (2022) The art of shockwave lithotripsy is an endangered species and is worth saving: the perspective of the European Association of Urology (EAU) Young Academic Urology (YAU) Urolithiasis group. World J Urol 40:1265–1266. https://doi.org/10.1007/s00345-021-03883-3
Dasgupta R, Cameron S, Aucott L et al (2022) Shockwave lithotripsy compared with ureteroscopic stone treatment for adults with ureteric stones: the TISU non-inferiority RCT. Health Technol Assess 26:1–70. https://doi.org/10.3310/WUZW9042
Kacker R, Zhao L, Macejko A, Thaxton CS, Stern J, Liu JJ, Nadler RB (2008) Radiographic parameters on noncontrast computerized tomography predictive of shock wave lithotripsy success. J Urol 179:1866–1871. https://doi.org/10.1016/j.juro.2008.01.038
Funding
Open access funding provided by Örebro University. This work was supported by the Örebro County Council [grant numbers OLL-935231, OLL-979997].
Author information
Authors and Affiliations
Contributions
Project development: MP, JJ, MW, PS, ML; Data collection: MP; Data analysis: MP, ML; Manuscript writing: MP; Critical review and final editing: MP, JJ, MW, PS, ML.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This retrospective study was performed in accordance with the ethical standards of the regional research committee and the 1964 Helsinki declaration and its later amendments. The Swedish Ethical Review Authority approved the study protocol and waived the informed consent requirement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Popiolek, M., Jendeberg, J., Sundqvist, P. et al. Finding the optimal candidate for shock wave lithotripsy: external validation and comparison of five prediction models. Urolithiasis 51, 66 (2023). https://doi.org/10.1007/s00240-023-01444-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00240-023-01444-4