Abstract
Objective
In recent years, the minimally invasive surgical treatment methods of ureteropelvic junctional obstruction (UPJO) have been diverse, but its approach and choice of surgical method are controversial. This network meta-analysis (NMA) aimed to compare the safety and effectiveness of minimally invasive surgeries for UPJO, which included robotic or laparoscopic pyeloplasty, via the retroperitoneal or transperitoneal approach.
Methods
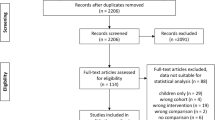
We searched relevant RCTs in PubMed, Embase, Web of Science, the Cochrane Library, and CNKI. To assess the results of operative time, complications and success rate, pairwise, and NMA were carried out. The models for analyses were performed by Revman 5.3, Addis V1.16.8 and R software.
Results
A total of 6 RCTs were included in this study involving four types of surgeries: transperitoneal laparoscopic pyeloplasty (T-LP), retroperitoneal laparoscopic pyeloplasty (R-LP), robot-assisted transperitoneal pyeloplasty (T-RALP), and robot-assisted retroperitoneal pyeloplasty (R-RALP). This study consisted of 381 patients overall. T-RALP had a quicker operational duration (SMD = 1.67, 95% CI 0.27–3.07, P = 0.02) than T-LP. According to the NMA's consistency model, T-RALP improved the surgical success rate more than T-LP (RR = 6303.19, CI 1.28 to 1.47 × 1011). Ranking probabilities indicated that RALP could be the better option than LP and retroperitoneal approach was comparable to transperitoneal approach. All procedures had high surgical success rates and few complications.
Conclusion
Outcomes for four surgical approaches used in the UPJO were comparable, with T-RALP being the most recommended approach. Selection between the transperitoneal and retroperitoneal approaches primarily depended on the surgeon's preference. Higher quality evidence is needed to further enhance the result.






Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Schuessler WW, Grune MT, Tecuanhuey LV, Preminger GM (1993) Laparoscopic dismembered pyeloplasty. J Urol 150(6):1795–1799
Gettman MT, Neururer R, Bartsch G, Peschel R (2002) Anderson-Hynes dismembered pyeloplasty performed using the da Vinci robotic system. Urology 60(3):509–513
Autorino R, Eden C, El-Ghoneimi A et al (2014) Robot-assisted and laparoscopic repair of ureteropelvic junction obstruction: a systematic review and meta-analysis. Eur Urol 65(2):430–452
Cestari A, Buffi NM, Lista G et al (2010) Retroperitoneal and transperitoneal robot-assisted pyeloplasty in adults: techniques and results. Eur Urol 58(5):711–718
Light A, Karthikeyan S, Maruthan S, Elhage O, Danuser H, Dasgupta P (2018) Peri-operative outcomes and complications after laparoscopic vs robot-assisted dismembered pyeloplasty: a systematic review and meta-analysis. BJU Int 122(2):181–194
Chua ME, Ming JM, Kim JK et al (2021) Meta-analysis of retroperitoneal vs transperitoneal laparoscopic and robot-assisted pyeloplasty for the management of pelvi-ureteric junction obstruction. BJU Int 127(6):687–702
Wan X, Wang W, Liu J, Tong T (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14(1):135
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805
Cipriani A, Higgins JP, Geddes JR, Salanti G (2013) Conceptual and technical challenges in network meta-analysis. Ann Intern Med 159(2):130–137
Veroniki AA, Vasiliadis HS, Higgins JP, Salanti G (2013) Evaluation of inconsistency in networks of interventions. Int J Epidemiol 42(1):332–345
Shoma AM, El Nahas AR, Bazeed MA (2007) Laparoscopic pyeloplasty: a prospective randomized comparison between the transperitoneal approach and retroperitoneoscopy. J Urol 178(5):2020–2024 (discussion 2024)
Singh V, Sinha RJ, Gupta DK, Kumar V, Pandey M, Akhtar A (2014) Prospective randomized comparison between transperitoneal laparoscopic pyeloplasty and retroperitoneoscopic pyeloplasty for primary ureteropelvic junction obstruction. J Soc Laparoendosc Surg 18(3):e201400366
Badawy H, Zoaier A, Ghoneim T, Hanno A (2015) Transperitoneal versus retroperitoneal laparoscopic pyeloplasty in children: randomized clinical trial. J Pediatr Urol 11(3):122.e121-126
Khoder WY, Waidelich R, Ghamdi AMA, Schulz T, Becker A, Stief CG (2018) A prospective randomised comparison between the transperitoneal and retroperitoneoscopic approaches for robotic-assisted pyeloplasty in a single surgeon, single centre study. J Robot Surg 12(1):131–137
Silay MS, Danacioglu O, Ozel K, Karaman MI, Caskurlu T (2020) Laparoscopy versus robotic-assisted pyeloplasty in children: preliminary results of a pilot prospective randomized controlled trial. World J Urol 38(8):1841–1848
Jha AA, Sandhu AS, Dash SC et al (2022) Comparison of surgical and functional outcome of laparoscopic pyeloplasty and robot-assisted pyeloplasty for congenital uretero pelvic junction obstruction. J Urol Surg 9(1):20–24
Bird VG, Leveillee RJ, Eldefrawy A, Bracho J, Aziz MS (2011) Comparison of robot-assisted versus conventional laparoscopic transperitoneal pyeloplasty for patients with ureteropelvic junction obstruction: a single-center study. Urology 77(3):730–734
Zuo W, Gao F, Yuan CW et al (2022) Trends in upper urinary tract reconstruction surgery over a decade based on a multi-center database. J Peking Univ Health Sci 54(4):692–698
Merseburger AS, Herrmann TR, Shariat SF et al (2013) EAU guidelines on robotic and single-site surgery in urology. Eur Urol 64(2):277–291
Song P, Shu M, Peng Z et al (2022) Transperitoneal versus retroperitoneal approaches of pyeloplasty in management of ureteropelvic junction obstruction: a meta-analysis. Asian J Surg 45(1):1–7
Uhlig A, Uhlig J, Trojan L, Hinterthaner M, von Hammerstein-Equord A, Strauss A (2019) Surgical approaches for treatment of ureteropelvic junction obstruction: a systematic review and network meta-analysis. BMC Urol 19(1):112
Watt J, Tricco AC, Straus S, Veroniki AA, Naglie G, Drucker AM (2019) Research techniques made simple: network meta-analysis. J Invest Dermatol 139(1):4-12.e11
Hutton B, Salanti G, Caldwell DM et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784
Chandrasekharam VVS, Babu R (2022) A systematic review and metaanalysis of open, conventional laparoscopic and robot-assisted laparoscopic techniques for re-do pyeloplasty for recurrent uretero pelvic junction obstruction in children. J Pediatr Urol. https://doi.org/10.1016/j.jpurol.2022.08.025
Cohen S, Raisin G, Dothan D, Jaber J, Kocherov S, Chertin B (2022) Robotic-assisted laparoscopic pyeloplasty (RALP), for ureteropelvic junction obstruction (UPJO), is an alternative to open pyeloplasty in the pediatric population. J Robot Surg 16(5):1117–1122
Andolfi C, Adamic B, Oommen J, Gundeti MS (2020) Robot-assisted laparoscopic pyeloplasty in infants and children: is it superior to conventional laparoscopy? World J Urol 38(8):1827–1833
Chandrasekharam VVS, Babu R (2021) A systematic review and meta-analysis of conventional laparoscopic versus robot-assisted laparoscopic pyeloplasty in infants. J Pediatr Urol 17(4):502–510
Andolfi C, Rodríguez VM, Galansky L, Gundeti MS (2021) Infant robot-assisted laparoscopic pyeloplasty: outcomes at a single institution, and tips for safety and success. Eur Urol 80(5):621–631
Pelizzo G, Nakib G, Romano P et al (2015) Five millimetre-instruments in paediatric robotic surgery: advantages and shortcomings. Minim Invasive Ther Allied Technol 24(3):148–153
Esposito C, Masieri L, Blanc T et al (2021) Robot-assisted laparoscopic pyeloplasty (RALP) in children with complex pelvi-ureteric junction obstruction (PUJO): results of a multicenter European report. World J Urol 39(5):1641–1647
Dothan D, Raisin G, Jaber J, Kocherov S, Chertin B (2021) Learning curve of robotic-assisted laparoscopic pyeloplasty (RALP) in children: how to reach a level of excellence? J Robot Surg 15(1):93–97
Casella DP, Fox JA, Schneck FX, Cannon GM, Ost MC (2013) Cost analysis of pediatric robot-assisted and laparoscopic pyeloplasty. J Urol 189(3):1083–1086
Janetschek G, Peschel R, Altarac S, Bartsch G (1996) Laparoscopic and retroperitoneoscopic repair of ureteropelvic junction obstruction. Urology 47(3):311–316
Rassweiler JJ, Teber D, Frede T (2008) Complications of laparoscopic pyeloplasty. World J Urol 26(6):539–547
Davenport K, Minervini A, Timoney AG, Keeley FX Jr (2005) Our experience with retroperitoneal and transperitoneal laparoscopic pyeloplasty for pelvi-ureteric junction obstruction. Eur Urol 48(6):973–977
Inagaki T, Rha KH, Ong AM, Kavoussi LR, Jarrett TW (2005) Laparoscopic pyeloplasty: current status. BJU Int 95(Suppl 2):102–105
Kaouk JH, Hafron J, Parekattil S et al (2008) Is retroperitoneal approach feasible for robotic dismembered pyeloplasty: initial experience and long-term results. J Endourol 22(9):2153–2159
Blanc T, Abbo O, Vatta F et al (2022) Transperitoneal versus retroperitoneal robotic-assisted laparoscopic pyeloplasty for ureteropelvic junction obstruction in children. A multicentre prospective study. Eur Urol Open Sci 41:134–140
El-Ghoneimi A, Farhat W, Bolduc S et al (2003) Laparoscopic dismembered pyeloplasty by a retroperitoneal approach in children. BJU Int 92(1):104–108
Acknowledgements
This study is funded by 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYGD18011). The authors thank again all who contributed to this project, for the help and support provided.
Author information
Authors and Affiliations
Contributions
P L and Y M contributed to conception and design of the study, and data analysis and/or interpretation; P L, X J, and K W were involved in acquisition of data; P L, Y M, and L X performed drafting of the manuscript and/or critical revision; H L and K W were responsible for revising and approving the final version of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
No ethical concerns.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
345_2023_4559_MOESM5_ESM.pdf
Supplementary file5 Figure S1. Risk of bias evaluation for all studies included. (A) Risk of bias graph. (B) Risk of bias summary. (PDF 173 KB)
345_2023_4559_MOESM6_ESM.png
Supplementary file6 Figure S2. The outcome for hospital stays. (A) Network meta-analysis. (B) Ranking probability. (C) Benefit-risk analysis including length of hospital stay indicator. (PNG 379 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, P., Ma, Y., Jin, X. et al. Comparative efficacy and safety of different minimal invasive pyeloplasty in treating patients with ureteropelvic junction obstruction: a network meta-analysis. World J Urol 41, 2659–2669 (2023). https://doi.org/10.1007/s00345-023-04559-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04559-w