Abstract
Purpose
This study aimed to evaluate the diagnostic value of serum and CT factors to establish a convenient diagnostic method for differentiating small (≤ 4 cm) fat-poor angiomyolipoma (AML) from renal cell carcinoma (RCC).
Materials and methods
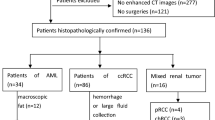
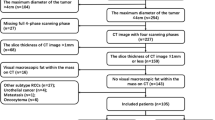
This study analyzed the preoperative serum laboratory data and CT data of 32 fat-poor AML patients and 133 RCC patients. The CT attenuation value of tumor (AVT), relative enhancement ratio (RER), and heterogeneous degree of tumor were detected using region of interest on precontrast phase (PCP) and the corticomedullary phase. Multivariate regression was performed to filter the main factors. The main factors were selected to establish the prediction models. The area under the curve (AUC) was measured to evaluate the diagnostic efficacy.
Results
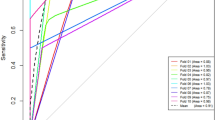
Fat-poor AML was more common found in younger (47.91 ± 2.09 years vs 53.63 ± 1.17 years, P = 0.02) and female (70.68 vs 28.13%, P < 0.001) patients. Alkaline phosphatase (ALP) was higher in RCC patients (81.80 ± 1.75 vs 63.25 ± 2.95 U/L, P < 0.01). For CT factors, fat-poor AML was higher in PCP_AVT (40.30 ± 1.49 vs 32.98 ± 0.69Hu, P < 0.01) but lower in RER (67.17 ± 3.17 vs 84.64 ± 2.73, P < 0.01). Gender, ALP, PCP_AVT and RER was found valuable for the differentiation. When compared with laboratory-based or CT-based diagnostic models, the combination model integrating gender, ALP, PCP_AVT and RER shows the best diagnostic performance (AUC = 0.922).
Conclusion
ALP was found higher in RCC patients. Female patients with ALP < 70.50U/L, PCP_AVT > 35.97Hu and RER < 82.66 are more likely to be diagnose as fat-poor AML.
Similar content being viewed by others
Data availability
For data availability, please contact the corresponding author.
References
Sanchez A, Feldman AS, Hakimi AA (2018) Current management of small renal masses, including patient selection, renal tumor biopsy, active surveillance, and thermal ablation. J Clin Oncol 36(36):3591–3600. https://doi.org/10.1200/JCO.2018.79.2341
Hakim SW, Schieda N, Hodgdon T, McInnes MD, Dilauro M, Flood TA (2016) Angiomyolipoma (AML) without visible fat: ultrasound, CT and MR imaging features with pathological correlation. Eur Radiol 26(2):592–600. https://doi.org/10.1007/s00330-015-3851-8
Carbonara U, Simone G, Minervini A et al (2021) Robotic-assisted partial nephrectomy for “very small” (<2 cm) renal mass: results of a multicenter contemporary cohort. Eur Urol Focus 7(5):1115–1120. https://doi.org/10.1016/j.euf.2020.10.001
Okhunov Z, Gorin MA, Jefferson FA et al (2021) Can preoperative renal mass biopsy change clinical practice and reduce surgical intervention for small renal masses? Urol Oncol 39(10):735 e17-735 e23. https://doi.org/10.1016/j.urolonc.2021.05.024
Su ZT, Patel HD, Huang MM et al (2022) Active surveillance versus immediate intervention for small renal masses: a cost-effectiveness and clinical decision analysis. J Urol 208(4):794–803. https://doi.org/10.1097/JU.0000000000002812
Wang X, Song G, Jiang H (2021) Differentiation of renal angiomyolipoma without visible fat from small clear cell renal cell carcinoma by using specific region of interest on contrast-enhanced CT: a new combination of quantitative tools. Cancer Imaging 21(1):47. https://doi.org/10.1186/s40644-021-00417-3
Kuusk T, Neves JB, Tran M, Bex A (2021) Radiomics to better characterize small renal masses. World J Urol 39(8):2861–2868. https://doi.org/10.1007/s00345-021-03602-y
Gong P, Liu Y, Gong Y et al (2021) The association of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio with post-thrombolysis early neurological outcomes in patients with acute ischemic stroke. J Neuroinflammation 18(1):51. https://doi.org/10.1186/s12974-021-02090-6
Razik A, Das CJ, Sharma S (2019) Angiomyolipoma of the kidneys: current perspectives and challenges in diagnostic imaging and image-guided therapy. Curr Probl Diagn Radiol 48(3):251–261. https://doi.org/10.1067/j.cpradiol.2018.03.006
Verma SK, Mitchell DG, Yang R et al (2010) Exophytic renal masses: angular interface with renal parenchyma for distinguishing benign from malignant lesions at MR imaging. Radiology 255(2):501–507. https://doi.org/10.1148/radiol.09091109
Tang Z, Yu D, Ni T, Zhao T, Jin Y, Dong E (2020) Quantitative analysis of multiphase contrast-enhanced CT Images: a pilot study of preoperative prediction of fat-poor angiomyolipoma and renal cell carcinoma. AJR Am J Roentgenol 214(2):370–382. https://doi.org/10.2214/AJR.19.21625
Li A, Xing W, Li H et al (2018) Subtype differentiation of small (</= 4 cm) solid renal mass using volumetric histogram analysis of DWI at 3-T MRI. AJR Am J Roentgenol 211(3):614–623. https://doi.org/10.2214/AJR.17.19278
Sagreiya H, Akhbardeh A, Li D et al (2019) Point shear wave elastography using machine learning to differentiate renal cell carcinoma and angiomyolipoma. Ultrasound Med Biol 45(8):1944–1954. https://doi.org/10.1016/j.ultrasmedbio.2019.04.009
Zaher DM, El-Gamal MI, Omar HA et al (2020) Recent advances with alkaline phosphatase isoenzymes and their inhibitors. Arch Pharm (Weinheim) 353(5):2000011. https://doi.org/10.1002/ardp.202000011
Lou Z, Lin W, Zhao H et al (2021) Alkaline phosphatase downregulation promotes lung adenocarcinoma metastasis via the c-Myc/RhoA axis. Cancer Cell Int. https://doi.org/10.1186/s12935-021-01919-7
Huang CW, Wu TH, Hsu HY et al (2022) Reappraisal of the role of alkaline phosphatase in hepatocellular carcinoma. J Pers Med. https://doi.org/10.3390/jpm12040518
Rao SR, Snaith AE, Marino D et al (2017) Tumour-derived alkaline phosphatase regulates tumour growth, epithelial plasticity and disease-free survival in metastatic prostate cancer. Br J Cancer 116(2):227–236. https://doi.org/10.1038/bjc.2016.402
Yu J, Zheng Q, Ding X et al (2019) Systematic re-analysis strategy of serum indices identifies alkaline phosphatase as a potential predictive factor for cervical cancer. Oncol Lett 18(3):2356–2365. https://doi.org/10.3892/ol.2019.10527
Nam HK, Sharma M, Liu J, Hatch NE (2017) Tissue nonspecific alkaline phosphatase (TNAP) regulates cranial base growth and synchondrosis maturation. Front Physiol 8:161. https://doi.org/10.3389/fphys.2017.00161
Choueiri TK, Kaelin WG Jr (2020) Targeting the HIF2-VEGF axis in renal cell carcinoma. Nat Med 26(10):1519–1530. https://doi.org/10.1038/s41591-020-1093-z
Liu Y, Lv H, Li X et al (2021) Cyclovirobuxine inhibits the progression of clear cell renal cell carcinoma by suppressing the IGFBP3-AKT/STAT3/MAPK-Snail signalling pathway. Int J Biol Sci 17(13):3522–3537. https://doi.org/10.7150/ijbs.62114
van der Doelen MJ, Stockhaus A, Ma Y et al (2021) Early alkaline phosphatase dynamics as biomarker of survival in metastatic castration-resistant prostate cancer patients treated with radium-223. Eur J Nucl Med Mol Imaging 48(10):3325–3334. https://doi.org/10.1007/s00259-021-05283-6
Li SJ, Lv WY, Du H et al (2019) Albumin-to-alkaline phosphatase ratio as a novel prognostic indicator for patients undergoing minimally invasive lung cancer surgery: propensity score matching analysis using a prospective database. Int J Surg 69:32–42. https://doi.org/10.1016/j.ijsu.2019.07.008
Tan P, Xie N, Ai J et al (2018) The prognostic significance of albumin-to-alkaline phosphatase ratio in upper tract urothelial carcinoma. Sci Rep 8(1):12311. https://doi.org/10.1038/s41598-018-29833-5
Brozovich A, Garmezy B, Pan T, Wang L, Farach-Carson MC, Satcher RL (2021) All bone metastases are not created equal: revisiting treatment resistance in renal cell carcinoma. J Bone Oncol 31:100399. https://doi.org/10.1016/j.jbo.2021.100399
Chen XY, Lan M, Zhou Y et al (2017) Risk factors for bone metastasis from renal cell cancer. J Bone Oncol 9:29–33. https://doi.org/10.1016/j.jbo.2017.10.004
Pecoraro A, Palumbo C, Knipper S et al (2021) Synchronous metastasis rates in T1 renal cell carcinoma: a surveillance, epidemiology, and end results database-based study. Eur Urol Focus 7(4):818–826. https://doi.org/10.1016/j.euf.2020.02.011
Kang HS, Park JJ (2021) Circularity index on contrast-enhanced computed tomography helps distinguish fat-poor angiomyolipoma from renal cell carcinoma: retrospective analyses of histologically proven 257 small renal tumors less than 4 cm. Korean J Radiol 22(5):735–741. https://doi.org/10.3348/kjr.2020.0865
Acknowledgements
We thank all of the members of the team. We are grateful to the financial support of the Department of Finance of Guangdong Province and Guangdong Provincial People’s Hospital.
Funding
This work was supported by Special Funding of Department of Finance of Guangdong Province (No. KS012022267) and NSFC Incubation Project of Guangdong Provincial People’s Hospital (No.KY0120220029).
Author information
Authors and Affiliations
Contributions
JL: Protocol development, Manuscript editing; TP: Data collection, Data analysis, Manuscript writing; JF: Data analysis, Manuscript writing; BX: Data collection, Data analysis; QW: Data collection; YC: Data collection; YL: Data collection; KW: Data collection; CF: Data collection; TL: Data collection; HC: Data collection, Data analysis; XP: Data management, Manuscript editing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval and consent to participate
The study has been approved by the Research Ethics Committee of Guangdong Provincial People’s Hospital (No. KY-Q-2022-122-01). As a retrospective study, the informed consent was waived by the committee.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peng, T., Fan, J., Xie, B. et al. Alkaline phosphatase combines with CT factors for differentiating small (≤ 4 cm) fat-poor angiomyolipoma from renal cell carcinoma: a multiple quantitative tool. World J Urol 41, 1345–1351 (2023). https://doi.org/10.1007/s00345-023-04367-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04367-2