Abstract
Purpose
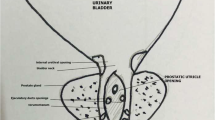
To determine the prevalence, radiological characteristics, and clinical symptomatology of enlarged prostatic utricles and vagina masculinus in boys with disorders of sex development.
Methods
Over 10 years (from February 2012 to March 2022), 102 boys with severe hypospadias underwent voiding cystourethrography. All patients presented with disorders of sex development and Y material in the karyotype (46,XY karyotype, 46,XY/45,X mosaic, etc.). The age of the patients at the first examination ranged from 4 days to 27 months (mean age 2.7 months).
Results
Voiding cystourethrography revealed the presence of a cyst posterior to the urethra in 66 patients (64.7% of cases). There were 15 cases of “vagina masculinus” and 51 of enlarged prostatic utricles. These dilations were classified according to the Ikoma classification and cyst size. In more than 2/3 of cases, the cysts were small (less than 20 mm), and in less than 8% of cases, these cysts were large. In addition, retrograde opacification revealed the presence of vesicoureteral reflux in 20% of boys with a male vagina. The most severe hypospadias with a scrotal or perineal meatus are most at risk of developing an enlarged prostatic utricle, and 80% of patients with Ikoma Grade III had a scrotal or perineal meatus.
Conclusion
This study shows that the prevalence of enlarged prostatic utricles and vagina masculinus is high in patients with severe hypospadias. Therefore, their search should be systematic, and for clinical and therapeutic interest, the enlarged prostatic utricles should be classified according to cyst size.

Similar content being viewed by others
References
Meyer R (1909) Zur Entwicklungsgeschichte und Anatomie des Utriculus prostaticus beim Menschen. Arch Mikrosk Anat 74:84–89
Shapiro E, Huang H, McFadden DE, Masch RJ, Eliza NG, Lepor H, Wu X-R (2004) The prostatic utricle is not a Müllerian duct remnant: immunohistochemical evidence for a distinct urogenital sinus origin. J Urol 172:1753–1756
Shebel HM, Farg HM, Kolokythas O, El-Diasty T (2013) Cysts of the lower male genitourinary tract: embryologic and anatomic considerations and differential diagnosis. Radiographics 33:1125–1143
Wolffenbuttel KP, Holmdahl G (2019) Perineal hypospadias repair with preservation of a coincidental vagina or perineal utricle in boys with disorders of sex development. J Pediatr Urol 15:626.e1-626.e5
Ikoma F, Shima H, Yabumoto H (1985) Classification of enlarged prostatic utricle in patients with hypospadias. Br J Urol 51:334–337
Ramachandra M, Bendre PS, Redkar RG, Taide DV (2009) Isolated prostatic utricle. J Indian Assoc Pediatr Surg 14:228–229
Acimi S, Abderrahmane N, Debbous L, Acimi MA, Mansouri J (2021) Koyanagi–Snow–Hayashi urethroplasty in severe hypospadias repair: between hope and reality. Urology 152:129–135
Oh CS, Chung IH, Won HS, Kim JH, Nam KI (2009) Morphologic variations of the prostatic utricle. Clin Anat 22:358–364
Kojima Y, Hayashi Y, Maruyama T, Sasaki S, Kohri K (2001) Comparison between ultrasonography and retrograde urethrography for detection of prostatic utricle associated with hypospadias. Urology 57:1151–1155
Siegel JF, Brock WA, Pena A (1995) Transrectal posterior sagittal approach to prostatic utricle (Mullerian duct cyst). J Urol 153:785–787
Howard FS (1948) Hypospadias with enlargement of the prostatic utricle. Surg Gynecol Obstet 86:307–316
Krstić ZD, Smoljanić Ž, Mićović Ž, Vukadinović V, Sretenović A, Varinac D (2001) Surgical treatment of the Müllerian duct remnants. J Pediatr Surg 36:870–876. https://doi.org/10.1053/jpsu.2001.23958
Yeung CK, Sihoe JDY, Tam YH, Lee KH (2001) Laparoscopic excision of prostatic utricles in children. BJU Int 87(6):505–508. https://doi.org/10.1046/j.1464-410X.2001.00132.x
Goruppi I, Avolio L, Romano P, Raffaele A, Pelizzo G (2015) Robotic-assisted surgery for excision of an enlarged prostatic utricle. Int J Surg Case Rep 10:94–96
Funding
None.
Author information
Authors and Affiliations
Contributions
SA, NB and NA contributed to the design and implementation of the research, SA, NA, LD, MAA to the analysis of the results and to the writing of the manuscript. SA conceived the original and supervised the project.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have NO affiliations with or involvement in any organization or entity with any financial interest in the subject matter or materials discussed in this manuscript.
Ethical compliance
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Acimi, S., Abderrahmane, N., Debbous, L. et al. Enlarged prostatic utricle and vagina masculinus in boys with disorders of sex development. World J Urol 41, 595–600 (2023). https://doi.org/10.1007/s00345-022-04273-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-04273-z