Abstract
Purpose
To assess the effects of a new ejaculation-sparing thulium laser enucleation of the prostate (ES-ThuLEP) technique on sexual functions and micturition, in patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia (BPH) and to evaluate how the surgical technique of ES-ThuLEP can lead to ejaculation preservation.
Methods
A prospective study was carried out between January 2015 and January 2018 on patients with surgical indication for BPH, who wished to preserve ejaculation. The patients were treated with ES-ThuLEP and were evaluated before and 3 and 6 months after surgery. Three validated questionnaires (ICIQ-MLUTSsex, IIEF-5 and IPSS) were used to assess changes in ejaculation, erectile function and urinary symptoms. Uroflowmetry (Qmax and Qavg), post-void residual volume and voided volume were also evaluated, to assess micturition improvement. Patients with moderate to severe erectile dysfunction were excluded. Statistical analysis was performed with the Student’s t test, Chi-square test and logistic regression analysis.
Results
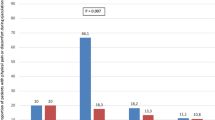
Two hundred and eighty three patients were enrolled. Ejaculation was spared in 203 and 219 patients at 3 and 6 months after surgery. No significant differences were observed between erectile function before and after surgery: baseline IIEF-5 = 16.2 ± 4.47 vs 16.7 ± 2.9 (p = 0.419) and 17.7 ± 3.2 (p = 0.410) at 3 and 6 months. Significant improvement in urinary symptoms was achieved: baseline IPSS = 19.4 ± 7.24 vs 5.8 ± 4.3 (p = 0.032) and 3.9 ± 4.1 (p = 0.029) at 3 and 6 months.
Conclusion
ES-ThuLEP effectively preserved ejaculation in over two thirds of the patients without compromising micturition improvement or erectile function. ES-ThuLEP could be a valid treatment option for BPH in young and sexually active men.
Similar content being viewed by others
References
Lee SWH, Chan EMC, Lai YK (2017) The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a systematic review and meta-analysis. Sci Rep 7(1):7984
Rosen R, Altwein J, Boyle P et al (2003) Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol 44(6):637–649
Naspro R, Gomez Sancha F, Manica M et al (2017) From “gold standard” resection to reproducible “future standard” endoscopic enucleation of the prostate: what we know about anatomical enucleation. Minerva Urol Nefrol 69(5):446–458
Herrmann TR (2016) Enucleation is enucleation is enucleation is enucleation. World J Urol 34(10):1353–1355
Gilling PJ, Kennett K, Das AK et al (1998) Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol 12(5):457–459
Herrmann TR, Bach T, Imkamp F et al (2010) Thulium laser enucleation of the prostate (ThuLEP): transurethral anatomical prostatectomy with laser support. Introduction of a novel technique for the treatment of benign prostatic obstruction. World J Urol 28(1):45–51
Bozzini G, Seveso M, Melegari S et al (2017) Thulium laser enucleation (ThuLEP) versus transurethral resection of the prostate in saline (TURis): a randomized prospective trial to compare intra and early postoperative outcomes. Actas Urol Esp 41(5):309–315
Sun F, Sun X, Shi Q et al (2018) Transurethral procedures in the treatment of benign prostatic hyperplasia: a systematic review and meta-analysis of effectiveness and complications. Medicine (Baltimore) 97(51):e13360
Lin Y, Wu X, Xu A et al (2016) Transurethral enucleation of the prostate versus transvesical open prostatectomy for large benign prostatic hyperplasia: a systematic review and meta-analysis of randomized controlled trials. World J Urol 34(9):1207–1219
Zhang J, Ou Z, Zhang X et al (2019) Holmium laser enucleation of the prostate versus thulium laser enucleation of the prostate for the treatment of large-volume prostates > 80 ml: 18-month follow-up results. World J Urol. https://doi.org/10.1007/s00345-019-02945-x
Gravas S, Cornu JN, Gacci M et al (2019) EAU guidelines on management of non-neurogenic male lower urinary tract symptoms (LUTS) incl. benign prostatic obstruction (BPO). EAU Guidelines Office, Arnhem, The Netherlands. https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/
DeLay KJ, Nutt M, McVary KT (2016) Ejaculatory dysfunction in the treatment of lower urinary tract symptoms. Transl Androl Urol 5(4):450–459
Marra G, Sturch P, Oderda M et al (2016) Systematic review of lower urinary tract symptoms/benign prostatic hyperplasia surgical treatments on men’s ejaculatory function: time for a bespoke approach? Int J Urol 23(1):22–35
Woo HH, Bolton DM, Laborde E et al (2012) Preservation of sexual function with the prostatic urethral lift: a novel treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Sex Med 9(2):568–575
Albisinni S, Aoun F, Roumeguère T et al (2017) New treatment strategies for benign prostatic hyperplasia in the frail elderly population: a systematic review. Minerva Urol Nefrol 69(2):119–132
Gratzke C, Barber N, Speakman MJ et al (2017) Prostatic urethral lift vs transurethral resection of the prostate: 2-year results of the BPH6 prospective, multicentre, randomized study. BJU Int 119(5):767–775
Lebdai S, Chevrot A, Doizi S et al (2019) Do patients have to choose between ejaculation and miction? A systematic review about ejaculation preservation technics for benign prostatic obstruction surgical treatment. World J Urol 37(2):299–308
Marberger H (1974) The mechanisms of ejaculation. Basic Life Sci 4(PT. B):99–110
Gallizia P (1972) The smooth sphincter of the vesical neck, a genital organ. Urol Int 27(4):341–354
Sturch P, Woo HH, McNicholas T et al (2015) Ejaculatory dysfunction after treatment for lower urinary tract symptoms: retrograde ejaculation or retrograde thinking? BJU Int 115(2):186–187
Gil-Vernet JM Jr, Alvarez-Vijande R, Gil-Vernet A et al (1994) Ejaculation in men: a dynamic endorectal ultrasonographical study. Br J Urol 73(4):442–448
Dorschner W, Stolzenburg JU (1994) A new theory of micturition and urinary continence based on histomorphological studies. 3. The two parts of the musculus sphincter urethrae: physiological importance for continence in rest and stress. UrolInt 52(4):185–188
Ronzoni G, De Vecchis M (1998) Preservation of anterograde ejaculation after transurethral resection of both the prostate and bladder neck. Br J Urol 81(6):830–833
Alloussi SH, Lang C, Eichel R et al (2014) Ejaculation-preserving transurethral resection of prostate and bladder neck: short- and long-term results of a new innovative resection technique. J Endourol 28(1):84–89
Talab SS, Santiago-Lastra YA, Bachmann A et al (2013) The impact of ejaculation-preserving photo-selective vaporization of the prostate (EP-PVP) on lower urinary tract symptoms and ejaculatory function: results of a multicenter study. J Urol 189(4):e164
Vickers AJ, Sjoberg DD (2015) Guidelines for reporting of statistics in European urology. EurUrol 67:181–187
Briganti A, Naspro R, Gallina A et al (2006) Impact on sexual function of holmium laser enucleation versus transurethral resection of the prostate: results of a prospective, 2-center, randomized trial. J Urol 175(5):1817–1821
Carmignani L, Bozzini G, Macchi A et al (2015) Sexual outcome of patients undergoing thulium laser enucleation of the prostate for benign prostatic hyperplasia. Asian J Androl 17(5):802–806
Cacciamani GE, Cuhna F, Tafuri A et al (2019) Anterograde ejaculation preservation after endoscopic treatments in patients with bladder outlet obstruction: systematic review and pooled-analysis of randomized clinical trials. Minerva Urol Nefrol 71(5):427–434
Kim M, Song SH, Ku JH et al (2015) Pilot study of the clinical efficacy of ejaculatory hood sparing technique for ejaculation preservation in Holmium laser enucleation of the prostate. Int J Impot Res 27(1):20–24
Gravas S, Bachmann A, Reich O et al (2011) Critical review of lasers in benign prostatic hyperplasia (BPH). BJU Int 107(7):1030–1043
Funding
The authors declare that no extra institutional funding was received.
Author information
Authors and Affiliations
Contributions
Protocol/project development: GB, LB, UB, CB, AC, MM, SM, BR. Data collection or management: GB, PB, RL, MM, ALP, MCS. Data analysis: GB, RL, ALP, MCS. Manuscript writing/editing: GB, LB. Execution of surgical procedures: GB. Supervision: GB, CB, SM, AM, BR.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest or any known competing financial interests.
Ethical approval
The study was performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by our local Ethical Commitee.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
All patients gave their consent for the publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bozzini, G., Berti, L., Maltagliati, M. et al. Ejaculation-sparing thulium laser enucleation of the prostate (ES-ThuLEP): outcomes on a large cohort. World J Urol 39, 2029–2035 (2021). https://doi.org/10.1007/s00345-020-03442-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03442-2