Abstract
Purpose
To describe the vacuum-assisted mini-percutaneous nephrolithotomy (vmPCNL) technique performed via the 16Ch ClearPetra sheath, to evaluate its outcomes and to analyze intrarenal pressure (IRP) fluctuations during surgery.
Methods
Data from all consecutive vmPCNL procedures from September 2017 to October 2019 were prospectively collected. Data included patients’ and stones characteristics, intra and peri-operative items, post-operative complications and stone clearance. Patients undergoing vmPCNL from March to October 2019 were submitted to IRP measurement during surgery.
Results
A total of 122 vmPCNL procedures were performed. Median stone volume was 1.92 cm3. Median operative time was 90 min and median lithotripsy and lapaxy time was 28 min. Stone clearance rate was 71.3%. Thirty-one (25.2%) patients experienced post-operative complications, seven of which were Clavien 3. Postoperative fever occurred in nine (7.4%) patients and one (0.8%) needed a transfusion. No sepsis were observed. IRPs were measured in 22 procedures. Mean IRP was 15.3 cmH2O and median accumulative time with IRP > 40.78 cmH2O (pyelovenous backflow threshold) was 28.52 sec. Maximum IRP peaks were reached during the surgical steps when aspiration is closed (mainly pyelograms), whereas during lithotripsy and suction-mediated lapaxy, the threshold of 40.78 cmH2O was overcome in three procedures.
Conclusions
vmPCNL is a safe procedure with satisfactory stone clearance rates. Mean IRP was always lower than the threshold of pyelo-venous backflow and the accumulative time with IRP over this limit was short in most of the procedures. During lithotripsy and vacuum-mediated lapaxy, IRP rarely raised over the threshold.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Percutaneous nephrolithotomy (PCNL) is the standard of care for large kidney stones [1], but complications like fever and bleeding can represent a major concern [2]. To reduce the morbidity associated with this procedure, miniaturized PCNL systems were developed [3,4,5,6]. However, these systems present some limitations such as a more difficult stone fragments retrieval, a smaller visual field, longer operative times (OT) and higher intrarenal pressures (IRPs) [7, 8]. In particular, IRP higher than 30 mmHg (40.78 cmH2O) has been proven to cause pyelovenous backflow [9], potentially leading to infectious complications [10]. To overcome these limitations, mini-PCNL systems provided with aspirating sheaths have been introduced. The real-time suction of irrigation fluid, stone fragments and blood throughout the procedure may lower IRP, ameliorate visibility and quicken the procedure. The aim of this study is to describe the vacuum-assisted mini-PCNL (vmPCNL) technique performed using the 16 Ch Clear Petra nephrostomic sheath and to evaluate its clinical outcomes. Ultimately, we aim to analyze IRPs profile during surgery and to identify the procedural steps during which IRP may rise the most.
Patients and methods
Data from all consecutive vmPCNL procedures performed at our academic referral stone center from September 2017 to October 2019 were prospectively collected. The indication to vmPCNL was given in all cases when PCNL was planned, except in case of large staghorn stones, for which standard PCNL (22–24 Ch) was indicated. In case of multiple stones allocated in different calyces with a significant total stone burden, for which a single standard-tract PCNL might not be surely efficacious, a multi-staged vmPCNL procedure was pre-operatively planned in order to reduce the operative time of the single procedures. Collected data concerned patients’ and stones’ characteristics, intra- and peri-operative items, post-operative complications, stone clearance and need of retreatment. Comorbidities were graded according to the Charlson Comorbidity Index [11]. Intraoperative items included number and location of the percutaneous tracts, fragments retrieval modality, lithotripsy and lapaxy time (LT) (from first laser activation to the end of fragments retrieval), exit strategy, operative time (OT) (from the beginning of ureteric catheter placement to the exit strategy) and intraoperative complications. Post-operative items included hemoglobin drop, need for transfusions, nephrostomy indwelling time and length of hospital stay. Post-operative complications were graded according to the PCNL-adjusted Clavien Score [12]. Sepsis was defined according to the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score criteria [13]. Stone clearance was defined as the absence of residual fragments larger than 4 mm at the CT scan or ultrasound (US) performed 1–3 months after surgery. All patients underwent pre-operative urographic CT scan and urine culture. In case of negative culture, one-shot antibiotic prophylaxis was administered; in case of positive culture, antibiotic targeted therapy was started 3–5 days before surgery. Stone volume was measured using the ellipsoid formula (a x b x c x π/6).
Armamentarium
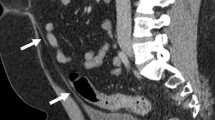
The vmPCNL procedures were performed using a 12 Ch nephroscope (MIP set, Karl Storz) and a 16 Ch Clear Petra disposable nephrostomic sheath (Well Lead Medical Co.). This sheath is externally plugged to prevent the medium from flowing out and it is equipped with a lateral oblique arm connected to the central vacuum system (Fig. 1). This allows the continuous aspiration of stone powder and irrigation fluid beside the scope during lithotripsy. Larger fragments are retrieved by drawing back the nephroscope inside the sheath as far as the internal opening of the lateral aspiration arm, wide enough to allow the passage of stones as large as 8 mm. Aspirated stones are collected in a dedicated plastic bottle. Irrigation is provided by a saline gravity bag allocated 1.5 m above the kidney level. The aspiration pressure can be regulated throughout the procedure according to surgical needs as shown in Fig. 1, in particular it can be enhanced to ameliorate visibility in the presence of stone powder or blood and while withdrawing the nephroscope inside the sheath to extract stone fragments.
a The ClearPetra set (Well Lead Medical Co., Ltd., China) is composed of a Y-shaped nephrostomic sheath connected, by means of an aspiration tube, to a stone collection bottle (200 ml), which is in turn linked to the central vacuum system. b A valve on the stone collection bottle regulates the aspiration pressure. c A vent on the lateral arm of the sheath can be closed with a finger to increase aspiration pressure during lapaxy. In the meantime the nephroscope d is slowly drawn back until the red stripe on the sheath, thus allowing fragments to fall in the lateral arm of the sheath and in the stone collection bottle
Surgical technique
The procedure starts by placing a ureteric catheter in the renal pelvis and obtaining a retrograde pyelogram. With the patient in the semi-supine Valdivia position, renal puncture is performed under fluoroscopic/ultrasonographic control. Tract dilation is performed one-shot, using the 16 Ch Clear Petra sheath assembled with its stylet. After introducing the nephroscope in the renal cavities, the aspiration valve is switched on. Lithotripsy is performed via a 550 μm Holmium: YAG laser fiber. Stone fragments are real-time evacuated during lithotripsy through suction; a basket can be employed to catch fragments in calyces not aligned with the aspirating sheath, only reachable with a flexible scope. A nephrostomy tube is usually placed as exit strategy.
Intrarenal pressure measurement
The subgroup of continuous patients undergoing vmPCNL from March to October 2019 were submitted to IRP measurement. After zero adjustment, IRP was measured throughout the procedures, with a frequency of 50 measurements per second, through the open-end ureteric catheter in the renal pelvis, whose external end was connected to a pressure transducer of the urodynamic machine (Medtronic, Duet®Multi-P). Basal IRP was recorded before renal puncture. Mean and maximum IRPs and the accumulative time with IRP > 40.78 cmH2O were calculated for every procedure. The procedures were split in different surgical steps to analyze IRP fluctuations along surgery.
Statistical analysis
Data collection and analysis were performed using the statistical software SPSS 25.0.0.1 (©IBM Corp.). Mean and standard deviation (SD) and median and interquartile ranges (IQRs) were reported for continuous variables and proportions and percentages for categorical variables.
Results
A total of 122 vmPCNL procedures were performed on 119 renal units of 115 patients. Patients’ and stones’ baseline characteristics are reported in Table 1. Seventy-four (60.7%) patients had multiple stones and the median stone volume was 1.92 cm3. Surgery-related variables and post-operative outcomes are shown in Table 2. Eleven procedures (9%) were performed with multiple Clear Petra tracts. A basket was employed for fragments retrieval in 44 (36.1%) procedure in addition to suction. The median OT was 90 min and the median LT was 28 min. A total of 31 (25.2%) patients experienced post-operative complications, seven out of which were Clavien 3: three cases of renal colic managed by double J placement; three cases of bleeding, one requiring bladder irrigations and two needing angioembolization; and one case of colon perforation managed by temporary colostomy. One (0.8%) patient needed a blood transfusion and nine (7.4%) patients experienced fever managed by antibiotics (Clavien 2). No case of sepsis was observed. Stone clearance was obtained in eighty-seven (71.3%) patients. Out of the 35 patients (28.7%) who did not reach the stone clear status, nine (7.4% of the total) were retreated within the first 6 month of follow-up for residual fragments larger than 10 mm: seven of them underwent a second PCNL procedure, in a pre-operatively planned multi-staged procedure, and two were submitted to retrograde intrarenal surgery. All of them resulted stone clear after the second procedure. The remaining 26 (21.3% of the total) patients had non-obstructing residual fragments smaller than 10 mm and were planned to undergo follow-up imaging.
Data related to IRPs are reported in Table 3a. Twenty-two patients were included in the IRP measurement sub-cohort. The mean IRP during the procedures was 15.38 cmH2O. In all procedures but three, peaks over the threshold of 40.78 cmH2O were registered. Median accumulative time with IRP > 40.78 cmH2O was 28.52 s. During lithotripsy and suction-mediated lapaxy, the mean IRP was 13.29 cmH2O and the threshold of 40.78 cmH2O was overcome in three procedures. Maximum peaks were reached during pyelograms in thirteen (59%) procedures, during nephroscopy with closed aspiration in seven (32%) and during puncture in two (9%). IRP values during the different surgical steps are reported in Table 3b. Graphics representing the complete IRP profile during the 22 procedures are available as Online Resource. Two patients undergoing IRP measurement experienced Clavien 2 post-operative complications: one case of bleeding needing transfusion and one case of fever.
Discussion
To the best of our knowledge, this is the first study describing the vmPCNL technique performed with the Clear Petra nephrostomic sheath and analyzing IRPs profile during this procedure. The most described aspiration-assisted mini-PCNL system is the super-mini-PCNL (SMP) [14, 15], consisting of a fiberoptic nephroscope and a Y-shaped nephrostomic sheath connected to the aspiration. The Clear Petra sheath employs the same principles of SMP. One of the main advantages of these sets is that, while working with the aspirating sheath in close contact with the stone, the vacuum keeps the calculus in position during lithotripsy and directly attract fragments, thus preventing their scattering. In the first series of 141 patients treated with SMP [14], Zeng and colleagues reported a stone clearance rate of 90.1%, a fever rate of 11.3% and no transfusions. In our series, we obtained stone clearance in 71.3% of the patients. This result may be considered satisfactory for our real-life population, with multiple stones in 60.7% of the cases and a median total stone volume of 1.97 cm3. Patients treated with SMP had single stones in 88.7% of the cases and a mean diameter of 2.2 cm [14]. We recorded a median OT of 90 min, lower than the safety limit of 120 min described in the Literature [16], and a median LT of 28 min. As in the SMP series [14], we observed lower post-operative fever (7.4%) and transfusion (0.8%) rates than reported in the Literature for PCNL (10.8% and 7%, respectively) [2]. These results confirm that the principles of mini-invasiveness are respected and that short OTs and controlled IRPs could play a role in the prevention of infectious complications. This may be of extreme relevance in the present scenario characterized by increasingly frequent infections sustained by multi-drug-resistant pathogens [17, 18]. To investigate the association between elevated IRPs and infectious complications, Zhong and colleagues [19] inspected IRPs in-vivo during miniaturized PCNL. They observed that mean IRP ≥ 20 mmHg and accumulative time with IRP > 30 mmHg longer than 50 s were correlated with post-operative fever. Then, not only IRP peaks can be dangerous for kidney injuries development, but mostly the accumulative time at high pressures can be detrimental for infectious complications. Indeed, elevated IRPs and pyelo-venous backflow are associated with potential systemic absorption of bacteria often colonizing stones and subsequently contaminating the irrigation fluid during lithotripsy. In our series, mean IRP during vmPCNL procedures was 13.19 cmH2O and in no procedure a mean IRP > 27.19 cmH2O (20 mmHg) was recorded. Alsmadi and colleagues [20], who measured IRPs during SMP, registered an overall average IRP of 19.51 mmHg (26.52 cmH2O) and a mean IRP > 20 mmHg in 29.7% of the procedures. In both the studies, the threshold of 40.78 cmH2O was overpassed in most of the procedures (86% in our series and 79.7% in Alsmadi’s). However, we registered prolonged accumulative time with IRP > 40,78 cmH2O only in a minority of the cases (31.8%, 22.7% and 13.6% for more than 50 s, 60 s and 70 s, respectively) and the median accumulative time with IRP over the threshold was 28.52 s. Alsmadi and colleagues calculated accumulative time with IRP > 40,78 cmH2O longer than 50 s, 60 s and 70 s in 36%, 32.4% and 27% of the cases, respectively, and a median accumulative time with IRP over the threshold of 55 s. The slightly higher IRPs registered during SMP might be due to the use a continuous perfusion pump, that was never applied during the procedures described in the present study, in which irrigation was always provided by gravity, limiting the fluid inflow. In our series, among the cases studied for IRP fluctuations, only one patient experienced post-operative fever, thus, it was not possible to identify IRP-related predictive factors for infectious events. This patient had positive pre-operative urine culture and stone culture, treated with targeted full-course peri-operative antibiotic therapy. Mean IRP during this procedure was 13.9 cmH2O and the accumulative time with IRP > 40.78 cmH2O was 15 s, with a maximum peak at 60 cmH2O during a pyelography (Graphic n.5 in the Online Resource). IRP does not seem to have contributed to post-operative fever in this patient, but the positive cultures, even if treated, represented a risk factor. Potentially, even short times with IRP over the backflow threshold are enough to determine bacterial reabsorption in case of clearly contaminated irrigation fluids.
For what concerns the IRP fluctuations, we observed that during lithotripsy and suction-mediated lapaxy, the threshold of 40.78 cmH2O was overcome in only three procedures (13.6%) (Graphics n. 9, 11, 12 in the Online Resource), meaning that when aspiration is activated, the risk of uncontrolled pressures is low. During surgical steps, when aspiration is closed, we registered rises in IRP. Maximum pressure peeks were registered during pyelograms in 13 (59%) procedures, during nephroscopy with closed aspiration in 7 (32%) and during puncture in 2 (9%). However, the mentioned steps usually are not prolonged in duration, and do not expose the patient to long time elevated IRPs.
The main limitation of this study is the lack of a control group of mini-PCNL procedures performed without aspiration systems which could render our results more significant. One more limitation is represented by the non-uniformity of the imaging modality we adopted in the follow-up: indeed, although CT scan is much more sensitive in identifying residual fragments, in order to reduce the radiation exposure, in particular in recurrent stone formers, we routinely perform US after uneventful procedures performed for small single stones, in which the chance of residual fragments is low. In case of residual fragments at US, a CT scan is performed to plan a retreatment.
Conclusions
VmPCNL via the 16 Ch Clear Petra sheath is characterized by a good safety profile and satisfactory stone clearance rates. The most interesting features of this technique are the easy suction-mediated stone fragments removal, the low complications rate and the favorable IRP profile. In particular, in our series, the mean IRP during surgery was always lower than the threshold of pyelo-venous backflow and the accumulative time with IRP over this limit was very short in most of the procedures. The maximal IRP peaks were registered during the surgical steps when aspiration is closed and mostly during pyelograms, whereas, during lithotripsy and vacuum-mediated lapaxy, IRP rarely raised over the threshold.
References
Turk CSC, Skolarikos A, Neisius A, Petrik A (2019) EAU guidelines. Edn. Presented at the EAU annual congress in Barcelona
Seitz C et al (2012) Incidence, prevention, and management of complications following percutaneous nephrolitholapaxy. Eur Urol 61(1):146–158
Jackman SV, Docimo SG, Cadeddu JA, Bishoff JT, Kavoussi LR, Jarrett TW (1998) The ‘mini-perc’ technique: a less invasive alternative to percutaneous nephrolithotomy. World J Urol 16(6):371–374
Desai J, Solanki R (2013) Ultra-mini percutaneous nephrolithotomy (UMP): one more armamentarium. BJU Int 112(7):1046–1049
Bader MJ, Gratzke C, Seitz M, Sharma R, Stief CG, Desai M (2011) The ‘all-seeing needle’: initial results of an optical puncture system confirming access in percutaneous nephrolithotomy. Eur Urol 59(6):1054–1059
Ganpule AP, Bhattu AS, Desai M (2014) PCNL in the twenty-first century: role of Microperc, Miniperc, and Ultraminiperc. World J Urol 33(2):235–240
Wu C, Hua L-X, Zhang J-Z, Zhou X-R, Zhong W, Ni H-D (2017) Comparison of renal pelvic pressure and postoperative fever incidence between standard- and mini-tract percutaneous nephrolithotomy. Kaohsiung J Med Sci 33(1):36–43
Doizi S, Uzan A, Keller E, De Coninck V, Rodriauez-Monsalve Herrero M, Traxer O (2018) Comparison of intrarenal pelvic pressure levels during flexible ureteroscopy, minipercutaneous nephrolithotomy and conventional percutaneous nephrolithotomy in a kidney model. Eur Urol Suppl 17(2):e1400–e1401
Hinman F (1926) F; Redewill, “pyelovenous back flow”. J Am Med Assoc 87:1287–1293
Kreydin EI, Eisner BH (2013) Risk factors for sepsis after percutaneous renal stone surgery. Nat Rev Urol 10(10):598–605
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40(5):373–383
de la Rosette JJMCH et al (2012) Categorisation of complications and validation of the clavien score for percutaneous nephrolithotomy. Eur Urol 62(2):246–255
Singer M et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315(8):801
Zeng G et al (2016) Super-mini percutaneous nephrolithotomy (SMP): a new concept in technique and instrumentation. BJU Int 117(4):655–661
Zeng G, Zhu W, Liu Y, Fan J, Zhao Z, Cai C (2017) The new generation super-mini percutaneous nephrolithotomy (SMP) system: a step-by-step guide. BJU Int 120(5):735–738
Xu S et al (2014) A prospective comparative study of haemodynamic, electrolyte, and metabolic changes during percutaneous nephrolithotomy and minimally invasive percutaneous nephrolithotomy. World J Urol 32(5):1275–1280
Tandogdu Z, Wagenlehner FME (2016) Global epidemiology of urinary tract infections. Curr Opin Infect Dis 29(1):73–79
Foxman B (2014) Urinary tract infection syndromes. Infect Dis Clin North Am 28(1):1–13
Zhong W, Zeng G, Wu K, Li X, Chen W, Yang H (2008) Does a smaller tract in percutaneous nephrolithotomy contribute to high renal pelvic pressure and postoperative fever? J Endourol 22(9):2147–2151
Alsmadi J, Fan J, Zhu W, Wen Z, Zeng G (2018) The influence of super-mini percutaneous nephrolithotomy on renal pelvic pressure in vivo. J Endourol 32(9):819–823
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
SPZ: protocol development; project development; data collection; data analysis; manuscript writing. EL: project development; data collection; manuscript editing. MF: protocol development; data management; data collection. MT: data collection. AG: manuscript editing. FL: project development. GA: project development. EDL: project development. EM: protocol development, project development, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was conducted collecting data obtained for clinical purposes and all the procedures were performed as part of the routine care. Then, our study did not need ethical approval. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study prior to the procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zanetti, S.P., Lievore, E., Fontana, M. et al. Vacuum-assisted mini-percutaneous nephrolithotomy: a new perspective in fragments clearance and intrarenal pressure control. World J Urol 39, 1717–1723 (2021). https://doi.org/10.1007/s00345-020-03318-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03318-5