Abstract
Background and objective
In addition to the evaluation of voiding symptoms, in the evaluation of patients with nocturia, one should also consider other related causes such as sleep disorders, obstructive sleep apnoea (OSAS), diabetes and heart failure. In this study, we have aimed to assess the current knowledge and implementation of the EAU guidelines regarding nocturia in common urological practice in the Netherlands.
Setting and participants
In a national cross-sectional survey distributed among 450 urologists and urology residents in the Netherlands, the implementation of the recommendations of the European Association of Urology (EAU) guidelines on nocturia evaluation and management was studied.
Results and limitations
This survey revealed that only some aspects of the EAU guidelines are applied in the daily clinical practice and that some important parts are not. For example, only a minority asks about alcohol consumption and symptoms suggestive for diabetes or OSAS. In addition, a majority reported to use a bladder diary for 1–3 days instead of for a minimum of 3 days as recommended by the EAU guidelines. In the management of nocturia, a trial of timed diuretic therapy is only reported by a minority, whereas the use of beta-3 antagonists, which is not mentioned in the guidelines, is applied by a large majority. Desmopressin recommended for nocturnal polyuria is prescribed by two-third of Dutch urologists.
Conclusions
These observations mandate better education and campaigns to raise the awareness on the EAU-guideline recommendations for nocturia.


Similar content being viewed by others
References
Abrams P, Cardozo L, Fall M et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:167
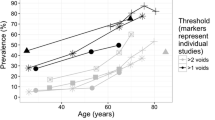
Zumrutbas AE, Bozkurt AI, Alkis O et al (2016) The prevalence of nocturia and nocturnal polyuria: can new cutoff values be suggested according to age and sex? Int Neurourol J 20:304
Sakalis VI, Karavitakis M, Bedretdinova D et al (2017) Medical treatment of nocturia in men with lower urinary tract symptoms: systematic review by the European Association of Urology guidelines panel for male lower urinary tract symptoms. Eur Urol 72:757
Djavan B (2005) The impact of tamsulosin oral controlled absorption system (OCAS) on nocturia and the quality of sleep: preliminary results of a pilot study. Eur Urol Suppl 4:61–68
Yokoyama O, Hiro S, Hotta S et al (2014) Efficacy of fesoterodine on nocturia and quality of sleep in Asian patients with overactive bladder. Urology 83:750
Johnson TM 2nd, Burrows PK, Kusek JW et al (2007) The effect of doxazosin, finasteride and combination therapy on nocturia in men with benign prostatic hyperplasia. J Urol 178:2045
Oelke M, Roehrborn CG, D’Ancona C et al (2014) Impact of dutasteride on nocturia in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia (LUTS/BPH): a pooled analysis of three phase III studies. World J Urol 32:1141
Oelke M, Weiss JP, Mamoulakis C et al (2014) Effects of tadalafil on nighttime voiding (nocturia) in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a post hoc analysis of pooled data from four randomized, placebo-controlled clinical studies. World J Urol 32:1127
Cornu JN, Abrams P, Chapple CR et al (2012) A contemporary assessment of nocturia: definition, epidemiology, pathophysiology, and management—a systematic review and meta-analysis. Eur Urol 62:877
Gulur DM, Mevcha AM, Drake MJ (2011) Nocturia as a manifestation of systemic disease. BJU Int 107:702
Drake MJ (2015) Should nocturia not be called a lower urinary tract symptom? Eur Urol 67:289
Bosch JL, Everaert K, Weiss JP et al (2016) Would a new definition and classification of nocturia and nocturnal polyuria improve our management of patients? ICI-RS 2014. Neurourol Urodyn 35:283
Grimshaw JM, Russell IT (1993) Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 342:1317
Nestler T, Baunacke M, Drager D et al (2018) Testicular cancer guideline adherence and patterns of care in Germany: a nationwide survey. Eur J Cancer Care (Engl) 25:e12917. https://doi.org/10.1111/ecc.12917
Cacciamani G, Artibani W, Briganti A et al (2018) Adherence to the European Association of Urology guidelines: a national survey among Italian urologists. Urol Int 100:139
Hendricksen K, Aziz A, Bes P et al (2017) Discrepancy between European Association of Urology guidelines and daily practice in the management of non-muscle-invasive bladder cancer: results of a European survey. Eur Urol Focus. https://doi.org/10.1016/j.euf.2017.09.002
Denys MA, Cherian J, Rahnama’i MS et al (2016) ICI-RS 2015—Is a better understanding of sleep the key in managing nocturia? Neurourol Urodyn 37(7):2048–2052. https://doi.org/10.1002/nau.23032
Visser PS, Krosnick JA, Marquette J, Curtin M (1996) Mail surveys for election forecasting? An evaluation of the Colombia Dispatch poll. Public Opin Q 60:181–227
Keeter S, Kennedy C (2006) Gauging the impact of growing nonresponse on estimates from a national RDD telephone survey. Public Opin Q 70:759
Author information
Authors and Affiliations
Contributions
MSR: protocol/project development; data collection or management; data analysis manuscript writing/editing. DMJV: data collection or management; data analysis manuscript writing/editing. SH: data analysis manuscript writing/editing. GAK: data analysis manuscript writing/editing. TATM: protocol/project development; data collection or management; data analysis manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Patient summary In a survey, Dutch urologists were asked about how they applied the recommendations made by European guidelines on how to treat patients bothered by nocturia. The study revealed that some important aspects of the guidelines are not applied in the clinical practice.
Rights and permissions
About this article
Cite this article
Rahnama’i, M.S., Vrijens, D.M.J., Hajebrahimi, S. et al. The discrepancy between European Association of Urology (EAU) guidelines and daily practice in the evaluation and management of nocturia: results of a Dutch survey. World J Urol 37, 2517–2522 (2019). https://doi.org/10.1007/s00345-019-02638-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02638-5