Abstract
Purpose
To evaluate the role of adrenergic and nitrergic signaling on ureteric peristaltic frequency and contraction force in vivo using a large animal model.
Methods
Twelve female pigs (72 ± 4 kg) were chronically instrumented with an electronic pressure-monitoring catheter in the right ureter. Nephrostomy, cystostomy, and arterial and venous catheters were left in situ. Ureteral peristalsis was recorded before and after the administration of propranolol, isoprenaline, doxazosin, urapidil, phenylephrine, LNNA (Nω-nitro-l-arginine), and l-arginine.
Results
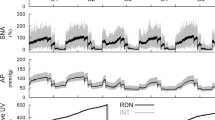
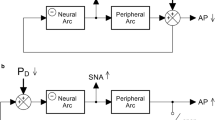
α1-Adrenergic receptor stimulation resulted in an increased P max and peristaltic frequency. However, α1-inhibition decreased P max alone. Similarly, β-adrenergic stimulation decreased P max and peristaltic frequency, whereas β-inhibition increased only P max. LNNA administration increased P max in the distal ureter and hydrostatic pressure in the pyelocalyceal system. l-Arginine did not affect P max or frequency, but resulted in a significantly higher diuresis. Either agonist or antagonist of NO did not affect peristaltic frequency and length of contraction.
Conclusions
Activation of α- and β-adrenergic receptors, respectively, stimulates and inhibits ureteric peristalsis. The biological effect of NO on ureteric motility is regionally determined and corresponds to the distribution of NOS-positive nerves. Inhibition of NOS activity increases P max in the distal ureter and tonic activity of the ureteric muscle resulting in higher hydrostatic pressure in the renal pelvis.




Similar content being viewed by others
References
Osman F, Romics I, Nyírády P et al (2009) Ureteral motility. Acta Physiol Hung 96:407–426. doi:10.1556/APhysiol.96.2009.4.2
Santicioli P, Maggi CA (1998) Myogenic and neurogenic factors in the control of pyeloureteral motility and ureteral peristalsis. Pharmacol Rev 50:683–722
Lang RJ, Davidson ME, Exintaris B (2002) Pyeloureteral motility and ureteral peristalsis: essential role of sensory nerves and endogenous prostaglandins. Exp Physiol 87:129–146
Matsumoto R, Otsuka A, Suzuki T et al (2013) Expression and functional role of β3-adrenoceptors in the human ureter. Int J Urol 20:1007–1014. doi:10.1111/iju.12093
Hernández M, Prieto D, Simonsen U et al (1992) Noradrenaline modulates smooth muscle activity of the isolated intravesical ureter of the pig through different types of adrenoceptors. Br J Pharmacol 107:924–931
Andersson KE, Persson K (1994) Nitric oxide synthase and nitric oxide-mediated effects in lower urinary tract smooth muscles. World J Urol 12:274–280
Roshani H, Dabhoiwala NF, Dijkhuis T et al (2003) Pharmacological modulation of ureteral peristalsis in a chronically instrumented conscious pig model. I: effect of cholinergic stimulation and inhibition. J Urol 170:264–267. doi:10.1097/01.ju.0000071964.04804.e4
Roshani H, Dabhoiwala NF, Dijkhuis T, Lamers WH (2002) Intraluminal pressure changes in vivo in the middle and distal pig ureter during propagation of a peristaltic wave. Urology 59:298–302
Björk L, Nylén O (1972) Cineradiographic investigations of contraction in the normal upper urinary tract in man. Acta Radiol Diagn (Stockh) 12:25–33
Constantinou CE (1974) Renal pelvic pacemaker control of ureteral peristaltic rate. Am J Physiol 226:1413–1419
Jung HU, Frimodt-Møller PC, Osther PJ, Mortensen J (2006) Pharmacological effect on pyeloureteric dynamics with a clinical perspective: a review of the literature. Urol Res 34:341–350. doi:10.1007/s00240-006-0069-x
Arrighi N, Bodei S, Zani D et al (2007) Alpha1 adrenoceptors in human urinary tract: expression, distribution and clinical implications. Urologia 74:53–60
Hakim TS, Sugimori K, Camporesi EM, Anderson G (1996) Half-life of nitric oxide in aqueous solutions with and without haemoglobin. Physiol Meas 17:267–277
Wang X-H, Wang X, Shi M-J et al (2015) Systematic review and meta-analysis on phosphodiesterase 5 inhibitors and α-adrenoceptor antagonists used alone or combined for treatment of LUTS due to BPH. Asian J Androl. doi:10.4103/1008-682X.154990
Author’s contribution
Protocol/project development, N. F. Dabhoiwala; Supervision, W. H. Lamers; Data collection or management, H. Roshani; Data analysis, H. Roshani; Manuscript writing/editing, S. Weltings.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Experimental procedure and its hardware, data analysis and animal care
Experimental procedure operation
Intravenous anesthesia was induced using Thiopental® (5 mg/kg, Nesdonal Rhône Meurieux, France) and atropine (0.1 mg/kg). Pigs were intubated and ventilated. Booster doses of Sufentanyl® (0.04 mg/kg, Janssen Farmaceutical, Holland), Midazolam (0.6 mg/kg) and Pancuronium® (0.1 mg/kg, Pavulon/Organon Oss, The Netherlands) were administered. Anesthesia was maintained using Sufentanyl® (0.1 ml/kg/h), Midazolam (0.13 ml/kg/h) and Pancuronium® (0.06 ml/kg/h). Animals were hydrated with 0.9 % saline (approx. 10 ml/kg/h), and continuous ECG monitoring was undertaken. Perioperative antibiotic cover was administered using 0.067 mg penicillin/kg body weight. An 8F ureteric balloon catheter was endoscopically manipulated into the distal right ureter, and the balloon was only minimally inflated. Under fluoroscopic control, iodine contrast was injected through the core channel of this catheter to visualize the pyelocalyceal system. Under ultrasound guidance, fine-needle puncture of the right pyelocalyceal system was undertaken, and under fluoroscopic control, a guide wire was positioned in ureter. The puncture traject was then dilated telescopically over this guide wire. An electronic 6F pressure-monitoring catheter with twin measuring points was then tunneled subcutaneously from the cervical area via a small skin incision into the renal pelvis and subsequently into the distal right ureter. The distal measuring point was positioned at the juxtavesical portion of the ureter and the proximal point 6.5 cm more cranial in the lumen of the ureter. A pigtail nephrostomy catheter was also anchored in situ under fluoroscopic control in the small intrarenal pelvis of the pig. Additionally, a tunneled vesicostomy catheter for bladder pressure measurements was anchored in situ through a mini-laparotomy. Separate arterial and venous catheters were also tunneled and inserted into the carotid artery and jugular vein. All tunneled catheters were protected using a Kevlar® jacket (van Baal, Utrecht, the Netherlands). After the procedure, animals were allowed to recover fully during 9 days in their pen. During this postoperative recovery period, control registration of ureteric peristalsis was performed daily to assess post-surgery recovery time of ureteric peristalsis subsequent to renal pelvis manipulation.
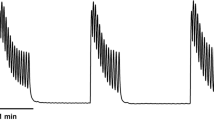
Pressure-monitoring catheter and hardware
A special F6 measuring catheter (Gealtec, Dunvegan, Isle of Skye, Scotland) with a twin pressure crystal transducer was used to record peristalsis. Distance between the two pressure measuring points was 6.5 cm. Two electrodes were localized adjacent to each pressure transducer to measure the EMG and impedance, and served as a positive control for the peristaltic waves. Ureteric EMG was registered using a bipolar setting and filter between 0 and 100 Hz. The ECG was also registered as a superimposed signal on the EMG curves. Impedance was measured between the two intraluminally placed ureteric electrodes and a skin electrode placed on a shaved, defatted area of skin in the homolateral lumbar region. The skin electrode was used to earth the animal. Impedance measurements were fed using an alternating current of 500 Hz and a 12-V transducer. Direct current resistance was <5 KΩ. The measurement box was hung about 1 m above the animal and was connected to the computer using a glass fiber cable. All data obtained were registered using LabVIEW (National Instrument Corp®, Austin, TX) software running on a Windows NT4® (Microsoft, Redmond, Oregon) operating system. The hardware and software required were specially developed in collaboration with the Department of Medical Physics at the Academic Medical Center (AMC), Amsterdam and BIOSEMI® (Amsterdam, The Netherlands). The catheter was zeroed every time before introduction at operation and was again checked before every data registration session.
Monitoring of hemo- and urodynamic signals
A multichannel Hewlett-Packard [HP-78342A (Hewlett-Packard, Andover, MA)] pressure transducer was used to register blood pressure via the arterial catheter. The jugular venous catheter was used for drug administration. To register the hydrostatic pressure in the renal pelvis and the bladder, the nephrostomy and cystostomy catheters, respectively, were used. The pressure transduction chambers were flushed and zeroed regularly at the level of the organ concerned.
Care and maintenance of animals
Each animal was physically examined daily. Pigs were fed a mineral-poor diet. They could drink and move freely within the pen. In all animals, urinary leakage from the nephrostomy ceased within 24 h. Urinary sediment and culture samples were collected systematically at regular intervals and were always negative. Ultrasound studies (using the B&K 3535 machine from B-K Medical, Herlev, Denmark) of the kidneys were undertaken before every registration session to determine the status of the upper tract. Only one animal revealed dilatation of its pyelocalyceal system and was excluded from the study. Nursing care of the animals was also regularly undertaken by the investigator to strengthen further the social bond with the animals and reduce animal stress to a minimum during the study period. Pigs are by nature inquisitive and intelligent but also destructive animals. It was therefore a great challenge to position and maintain intact all tunneled measuring catheters in situ during the weeks of experimentation. Despite our best efforts, we did lose one catheter as reported. All animal movement affects the registration of small signals negatively. To this end, the pig’s socialization program with the investigator was of crucial importance. It helped considerably to reduce the number of artifacts to a minimum and assure the success of the experiments.
Animal euthanasia
Pigs were sedated as described. Fluoroscopic imaging of the upper urinary tract was undertaken after perfusion (0.25 ml/min) of the nephrostomy with dilute iodine contrast as described in an earlier publication by us to confirm the presence of normal peristalsis 6 weeks postoperatively. The intraluminal catheter was found to have advanced in every case approximately two cm proximally towards the renal pelvis. When compared to its position on the day of introduction This was due in part to animal growth and/or some traction movement due to free mobility of the animal in the pen. Pigs were then euthanized in accordance with our animal laboratory guidelines (10 ml pentobarbital sodium 200 mg/ml I.V.). All urinary tracts were immediately harvested for histological analysis.
Data analysis
The amplitude (P max, cm H2O) of every pressure signal, its duration (s), and frequency (min−1) of the peristaltic curves were manually analyzed and recorded in a spreadsheet program. The duration of the pressure signal is converted into pressure signal length (mm) by multiplying duration with propagation velocity. Frequency distribution analysis of our data revealed a normal distribution pattern. This fact enabled us to determine the mean, standard error of the mean (SEM), and the P value using a two-tailed, unpaired student t test.
Appendix 2: Systemic effects of studied drug
β-Adrenergic group
Propranolol and isoprenaline administration significantly decreased (60 ± 3 min−1) and increased (186 ± 3 min−1) the heart rate (control: 83 ± 4 min−1, P < 0.05), respectively. Blood pressure dropped to 90/20 ± 2/5 mmHg with isoprenaline and to 120/75 ± 7/5 mmHg with propranolol in comparison to 150/85 ± 6/7 mmHg in the control phase (P < 0.05). The average diuresis of pigs in the propranolol, isoprenaline and control groups was 69 ± 1, 32 ± 1 and 66 ± 0 ml/h, respectively (isoprenaline: P < 0.05). Isoprenaline also caused intense reddening (flushing) of the skin due to extensive peripheral vasodilatation. Some pigs vomited and one pig died 92 min after administration of isoprenaline despite resuscitative measures being undertaken.
α1-Adrenergic group
Doxazosin (120 ± 4 min−1), urapidil (89 ± 1 min−1), and phenylephrine (150 ± 6 min−1) increased the heart rate in comparison with controls (83 ± 4 min−1, P < 0.05). Doxazosin (120/70 ± 8/6 mmHg) and urapidil (110/60 ± 4/4 mmHg) had an anti-hypertensive effect, whereas phenylephrine (200/112 ± 12/9 mmHg) increased blood pressure (control: 150/85 ± 6/7 mmHg, P < 0.05). The average rate of diuresis during doxazosin, urapidil, and phenylephrine treatment were 67 ± 1, 63 ± 0 and 67 ± 0 ml/h, as compared to 66 ± 0 ml/hour in the control group (P > 0.05).
Nitrergic group
In this study, inhibition of NO synthesis with LNNA resulted in hypertension, lasting approximately 3 days. The heart rate was increased as well. The diuresis, however, was not significantly different from the control group, perhaps because the increased blood pressure neutralizes the effects of vasoconstriction in the renal vascular bed. l-Arginine did result in a significantly higher diuresis rate due to its vasodilatory effect, increasing renal blood flow without significantly changing blood pressure.
l-arginine caused a nonsignificant decrease in heart rate from 81 ± 4 min−1 in controls to 75 ± 4 min−1. LNNA increased the heart rate to 120 ± 2 min−1; P < 0.05). Blood pressure decreased from 130/90 ± 6/7 mmHg in the control group to 120/90 ± 8/5 mmHg in the l-arginine group and increased to 300/190 ± 9/7 mmHg in the LNNA group (P < 0.05). The average diuresis of the pigs in the LNNA, l-arginine and control groups was 74 ± 2, 82 ± 1 and 70 ± 1 ml/h, respectively (P < 0.05 for the l-arginine group). No general symptoms were observed after l-arginine administration. Seven of the 11 pigs developed a nystagmus upon administration of LNNA.
Rights and permissions
About this article
Cite this article
Roshani, H., Weltings, S., Dabhoiwala, N.F. et al. Pharmacological modulation of ureteric peristalsis in a chronically instrumented conscious pig model: effect of adrenergic and nitrergic modulation. World J Urol 34, 747–754 (2016). https://doi.org/10.1007/s00345-015-1663-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1663-8