Abstract
Objectives
The Prostate Imaging Quality (PI-QUAL) score is a new metric to evaluate the diagnostic quality of multiparametric magnetic resonance imaging (MRI) of the prostate. This study assesses the impact of an intervention, namely a prostate MRI quality training lecture, on the participant’s ability to apply PI-QUAL.
Methods
Sixteen participants (radiologists, urologists, physicists, and computer scientists) of varying experience in reviewing diagnostic prostate MRI all assessed the image quality of ten examinations from different vendors and machines. Then, they attended a dedicated lecture followed by a hands-on workshop on MRI quality assessment using the PI-QUAL score. Five scans assessed by the participants were evaluated in the workshop using the PI-QUAL score for teaching purposes. After the course, the same participants evaluated the image quality of a new set of ten scans applying the PI-QUAL score. Results were assessed using receiver operating characteristic analysis. The reference standard was the PI-QUAL score assessed by one of the developers of PI-QUAL.
Results
There was a significant improvement in average area under the curve for the evaluation of image quality from baseline (0.59 [95 % confidence intervals: 0.50–0.66]) to post-teaching (0.96 [0.92–0.98]), an improvement of 0.37 [0.21–0.41] (p < 0.001).
Conclusions
A teaching course (dedicated lecture + hands-on workshop) on PI-QUAL significantly improved the application of this scoring system to assess the quality of prostate MRI examinations.
Key Points
• A significant improvement in the application of PI-QUAL for the assessment of prostate MR image quality was observed after an educational intervention.
• Appropriate training on image quality can be delivered to those involved in the acquisition and interpretation of prostate MRI.
• Further investigation will be needed to understand the impact on improving the acquisition of high-quality diagnostic prostate MR examinations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate magnetic resonance imaging (MRI) examinations must be of high quality to allow for accurate interpretations. Low diagnostic quality examinations will increase uncertainty in MRI decision-making [1]. Against this backdrop, the Prostate Imaging Reporting and Data System (PI-RADS) standards Versions 2.0 and 2.1 were developed to include a set of minimal technical requirements for the acquisition of good-quality MRI of the prostate [2, 3]. Additionally, two panels of experts have advocated the creation of standardised quality criteria for the evaluation of the image quality of prostate MRI [4, 5].
The Prostate Imaging Quality (PI-QUAL) score for prostate MRI represents the first standardised scoring system that evaluates image quality using objective technical criteria together with subjective visual criteria from the images [6].
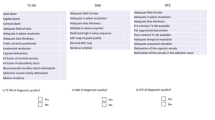
PI-QUAL score of 1 means that all MR sequences are below the minimum standard of diagnostic quality, a PI-QUAL score of 3 indicates that the study is of sufficient diagnostic quality (as at least two MR sequences taken together are of diagnostic quality), and a PI-QUAL score of 5 implies that all sequences are of optimal diagnostic quality (i.e., all clinically significant lesions can be ruled in AND ruled out) (Table 1).
The importance of reader training and experience in prostate MRI is both intuitive and evident from the literature [7, 8]. As the volume of prostate imaging grows, a larger and larger number of examinations are being performed in centres all over the world. Many sites are beginning for the first time, without a lot of experience in this examination. Dedicated imaging site and personnel efforts are required to ensure high quality.
The first step in reviewing a prostate MR exam is a critical review of its quality. In the current prostate cancer pathways, many patients will be seen by physicians with a prior prostate MR exam already performed elsewhere [9]. So, urologists, oncologists, and others without formal radiology training must be able to ascertain the overall quality of an exam and the resulting diagnostic report. Some men may require a repeat MR examination prior to deciding on treatment. Therefore, the ability to evaluate the quality of prostate MR studies is a crucial skill for clinicians treating prostate cancer.
The Nicholas Gourtsoyiannis Teaching Fellowship, established by the European School of Radiology (ESOR), is aimed at radiologists who wish to enhance their teaching and training skills by delivering lectures and undertaking interactive workshops. For the year 2021, the fellowship has been awarded to two separate projects on prostate MRI.
We report here the results from the second project, which focussed on how an educational intervention can be used to understand and apply the PI-QUAL score to evaluate the quality of prostate MRI images [6].
Our hypothesis was that dedicated training in assessing image quality by using the PI-QUAL score would significantly improve the ability of participants with different levels of experience and training backgrounds in determining the adequacy of the images.
Materials and methods
The 2021 fellowship recipient (F.G.) is a Consultant Radiologist with a particular interest in genitourinary imaging and highly experienced in prostate MRI (i.e., reporting more than 2,500 prostate MR scans per year), and who is also one of the developers of the PI-QUAL score [6].
The second teaching fellowship took place at Harvard Medical School/ Brigham and Women’s Hospital in Boston, MA, USA (Fig. 1), between January 10 and January 16, 2022.
Setting and participants
Study participants with different levels of experience in prostate MRI and training backgrounds (but all linked to the MR pathway for the diagnosis of prostate cancer) were invited from the departments of radiology and surgery/urology. The only prerequisites for participation were to have general knowledge of the anatomy of the prostate on MRI and to have been exposed to multiparametric MR images of the prostate before the course.
All participants were unaware of the specifics of the PI-QUAL assessment procedure and how to apply it.
MR examinations
All MR examinations included T2-weighted, diffusion-weighted, and dynamic contrast-enhanced sequences and it is important to mention that they were not always fully compliant with the PI-RADS recommendations (i.e., technical details), reflecting the heterogeneity of the conduct of prostate MRI across different centres [9]. The scans had been performed between November 2018 and September 2021 without an endorectal coil. All MR exams and images had been previously anonymised and uploaded onto a dedicated DICOM viewer. All participants reviewed all sets of cases and were blinded to the magnet vendor, field strength, and all clinical data.
Due to the institutional restrictions in place at the time of the fellowship (following the rapid spread of the Omicron variant of COVID-19), the teaching course was conducted on-site in Boston, USA, but it was decided to hold the lecture and the workshop also via a video-meeting platform to allow the attendees to join the lecture and the workshop remotely.
Specific of the educational intervention:
Figure 2 shows the framework of each step of the teaching fellowship during the week.
-
Day 1 and day 2 (pre-teaching case review)
In the two days prior to the lecture, the participants were asked to go through a set of different MR scans of the prostate independently. They filled a scoring sheet (Fig. 3) that was specifically created for this project by the course director (F.G.) in which they evaluated the quality of each of the three sequences (i.e., T2-weighted imaging, diffusion-weighted imaging and dynamic contrast-enhanced sequences). They were also asked to state if they would have repeated the scan due to poor image quality. No further instructions or guidelines were given, and the participants relied only on their previous knowledge in prostate MRI. Although we kept track of time, participants were allowed to work at their own pace to interpret the scans. The scoring sheets were returned and collated before the lecture and the workshop.
-
Day 3 (lecture + hands-on workshop)
All participants attended the lecture (1 h), which was followed by a Q and A session (30 min) in which they were encouraged to ask questions to improve their understanding of the subject.
Lecture framework
The lecture, whose title was: “Prostate MR and image quality: it is time to improve,” consisted of two modules:
-
Module 1-Prostate MRI: introduction to (i) the different MR sequences, (ii) the anatomy of the prostate gland, and (iii) the appearance of prostate cancer on MRI
-
Module 2-Review of the currently available papers addressing the issue of prostate MRI quality and explanation of the PI-QUAL score using a recently published primer [10]
Hands-on workshop framework
The workshop, whose title was: “The PI-QUAL score: from theory to practice,” was carried out after the lecture and included hands-on training to familiarise the participants with the PI-QUAL scoring system. During the workshop, which lasted for approximately 1 h, five scans from the pre-training cohort were reviewed and discussed collegially. The participants were taught how to evaluate image quality and assess the PI-QUAL score using the dedicated scoring sheet (Fig. 4) and the PI-QUAL primer. [10]
PI-QUAL scoring sheet for post-teaching scans. Reprinted with permission from Elsevier from Giganti F, Allen C, Emberton M, Moore CM, Kasivisvanathan V, for the PRECISION study group. Prostate Imaging Quality (PI-QUAL): A New Quality Control Scoring System for Multiparametric Magnetic Resonance Imaging of the Prostate from the PRECISION trial. Eur Urol Oncol (2020); 3(5):615-619.
-
Day 4 and day 5 (post-teaching case review)
All participants were asked to evaluate independently the image quality of a new set of 10 cases using the PI-QUAL scoring sheet. At the end of the workshop, their results were collated for analysis.
Clinical cohort and reference standard
All patients included in this study gave written informed consent to have their images used for research and teaching purposes. No Institutional Review Board approval was needed for this study, as the scans were from different MR systems and MR vendors at different centres and were randomly selected by a research assistant not involved in the study and with no clinical background.
The quality assessment given by the course director was used as the reference standard for the evaluation of the participants’ performance before and after the course.
Statistical analysis
The primary outcome was the change in the average area under the curve (AUC) for detection of suboptimal and optimal image quality (stratified by PI-QUAL 1-3 vs PI-QUAL 4-5) before and after teaching.
The pre-teaching scores given in the dedicated scoring sheet (i.e., inadequate image quality vs adequate image quality) were dichotomised into PI-QUAL 1-3 vs PI-QUAL 4-5.
Receiver operating characteristic (ROC) curves were based on generalised linear mixed models with participant and case ID taken as random effects. This approach generalises the Obuchowski-Rockette method [11] and is described by Liu et al [12].
For each ROC curve and AUC value, 95% confidence intervals (CIs) were computed by conditional bootstrap resampling (B = 50,000 samples).
Exact p values were computed by permutation methods to avoid any distributional assumption or asymptotic approximation and considered significant when < 0.05.
All statistical analyses were performed in R v. 4.1.3 (R Foundation for Statistical Computing).
Results
A total of sixteen participants completed the study. A total of twenty scans from twenty different patients were included. The image analysis sessions consisted of 10 cases in the pre- and 10 cases in the post-intervention groups. Table 2 shows the list of participants with their background and their level of experience in prostate MRI.
The MR examinations were diverse in vendor and field strength: 8/20 (40%) patients were scanned on Siemens®, 6/20 (30%) on General Electric®, and 6/20 (30%) on Philips® scanners.
Eleven out of twenty studies (55%) were conducted on a 1.5 T and 9/20 (45%) studies were conducted on a 3 T system.
Table 3 shows the MR vendors and systems, magnets and PI-QUAL scores (according to the reference standard) for each scan in the pre- and post-teaching cohorts.
PI-QUAL score
In the pre-teaching cohort, 5/10 (50%) scans were scored PI-QUAL 2, one (10%) scan was scored PI-QUAL 3, 3/10 (30%) scans were scored PI-QUAL 4, and for only one (10%) scan all sequences were of optimal diagnostic quality (i.e., PI-QUAL 5), according to the reference standard reported in each PI-QUAL scoring sheet (Supplementary Table 1).
In the post-teaching cohort, 2/10 (20%) scans were scored PI-QUAL 1, one (10%) scan was scored PI-QUAL 2, 5/10 (50%) scans were scored PI-QUAL 4, and 2/10 (20%) scans were scored PI-QUAL 5, according to the reference standard reported in each PI-QUAL scoring sheet (Supplementary Table 2).
Accuracy in evaluating image quality before and after teaching
There was a significant improvement in the average AUC for the evaluation of image quality (suboptimal vs optimal) from pre-teaching (0.59; [0.50-0.66]) to post-teaching (0.96 [0.92-0.98]), an improvement of 0.37 [0.21-0.41] (p < 0.001). The ROC curves presented in Fig. 5a summarise the average accuracy levels in evaluating image quality (stratified by PI-QUAL 1-3 vs PI-QUAL 4-5) before and after the teaching course.
Average area under the curve (AUC) for the evaluation of image quality (suboptimal vs optimal) in the pre-teaching (blue, dash-dotted line) and post-teaching (red, dashed line) cohorts, with shaded areas and square brackets representing the 95% confidence intervals (A). AUCs for the evaluation of image quality stratified by experience (i.e., < or > than 100 prostate MR scans evaluated) before (B) and after (C) teaching
We also evaluated the AUC in the assessment of image quality stratified by experience before and after teaching. Given the different background of the participants, this was stratified as non-experienced participants (i.e., < 100 prostate MR scans seen before the course) and experienced participants (i.e., > 100 prostate MR scans seen before the course).
For non-experienced participants, the pre-teaching AUC was 0.62 [0.47-0.76] and the post-teaching AUC was 0.93 [0.86-0.98], a difference of 0.31 [0.20-0.38] (p < 0.001).
For experienced participants, the pre-teaching AUC was 0.57 [0.47-0.67] and the post-teaching AUC was 0.98 [0.95-0.99], a difference of 0.41 [0.30-0.50] (p < 0.001).
The ROC curves shown in Fig. 5b (pre-teaching) and 5c (post-teaching) are a visual representation of these findings.
The PI-QUAL scores given by each participant after the course are presented in Table 4 and two examples of prostate MR examinations (one from the pre-teaching cohort and one from the post-teaching cohort) with their corresponding PI-QUAL scores (according to the reference standard) are presented in Fig. 6.
Two cases of prostate MRI from the two cohorts (pre- and post-teaching). The first case [A axial T2-weighted imaging; B diffusion-weighted imaging (high b value: 1,000 s/mm2); C apparent diffusion coefficient map; D dynamic-contrast enhanced sequences] is from the pre-teaching cohort and the reference standard was PI-QUAL 2, as only T2-WI is of sufficient diagnostic quality. Only 7/16 participants gave the correct PI-QUAL score for this scan, with 1/16 giving a PI-QUAL score of 3, 3/16 a PI-QUAL score of 4 and 5/16 a PI-QUAL score of 5. The second case [E axial T2-weighted imaging; F diffusion-weighted imaging (high b value: 2,000 s/mm2); G apparent diffusion coefficient map; H dynamic-contrast enhanced sequences] is from the post-teaching cohort and the reference standard was PI-QUAL 5. All patients scored this scan as of optimal diagnostic quality (i.e., PI-QUAL score 4 or 5; in detail: 9/16 scored PI-QUAL 4 and 7/16 scored PI-QUAL 5)
Discussion
In our study, we have shown that a dedicated teaching course on the application of PI-QUAL to evaluate the quality of prostate MRI is useful for radiologists and non-radiologists with different clinical background and levels of expertise in prostate MRI, ranging from radiologists with more than 30 years of prostate MR reporting to urologists and computer scientists who had seen only a few prostate MR exams before the course.
Our overall goal of providing an intervention to educate a diverse audience has been shown to be successful.
PI-QUAL can be understood and applied by participants and we hope, be an important contribution when used in the clinic to assess the overall value of prostate MRI.
In particular, the participants’ average accuracy in evaluating image quality (suboptimal vs optimal) significantly increased after a didactic lecture and a hands-on workshop.
Numerous efforts have been made to improve MR image quality in different organs other than the prostate, including the heart [13], liver [14], brain [15], and breast [16], as radiologists should become familiar with the requirements for good-quality MRI and strive to meet the expected standards to enhance patient quality and safety.
It has already been shown that dedicated teaching courses improve readers’ performances in MRI [17, 18]. The widespread use of this technique in prostate cancer has resulted in high variability of image quality for each sequence and clinical decisions can be compromised if the scans are not acquired at the highest standard [3].
A consensus report by the European Society of Urogenital Radiology (ESUR) and the European Association of Urology - Section of Urologic Imaging (ESUI) has pointed out the vast inconsistency in the conduction of prostate MRI [4].
In this pilot study, the study participants who evaluated the image quality had different backgrounds and different levels of experience in prostate MRI as reported in Table 2. The participants ranged from very experienced radiologists (i.e., reporting more than 1,500 prostate MR scans) scans to other expert clinicians (i.e., urologists) or physicists/computer scientists/engineers with very little experience.
All participants achieved very high and significant accuracy levels in the evaluation of image quality after the course, both overall and when split according to their experience (with the highest values for the experienced participants).
It is important to mention that MR examinations require careful oversight and attention to detail by radiographers and technologists. When starting out in many practices, it can be challenging, as the experience may be lacking. Prostate MR exams from non-academic centres can be variable and can be of suboptimal imaging quality due to a lack of awareness of the quality [9]. In contradistinction, quality is more consistent in high-volume academic centres where there are dedicated teams to oversee quality and radiologists are often involved in clinical research activities relating to prostate cancer imaging. Also, centres where there are large active biopsy programmes will also have more consistent quality as they often provide the MR images for MR-ultrasound fusion biopsy devices [9].
PI-QUAL is the first such effort to alert the MR imaging community of the importance of prostate MR quality. Therefore, the widespread understanding, awareness, application, and validation of this approach is necessary for future adoption [19,20,21], and the format of this course, with pre- and post-teaching assessment of MR image quality, could be very helpful to disseminate the use of the PI-QUAL score and promote the awareness of the importance of image quality in prostate MRI [22,23,24,25,26,27].
We believe that the results of our pilot study represent a first step in the right direction, although we should point out that the very high AUC after teaching does not reflect a true experience in evaluating prostate MR images, as this is something that can be achieved only after viewing several prostate MR scans.
This study has limitations; foremost is the small number of participants and MR examinations, but as a pilot study, it provided an impetus for more work with larger numbers.
In addition to this, the reference standard was based on the scores given by a single reader, although highly experienced in the evaluation of image quality by means of PI-QUAL. Given the promising results in terms of inter-reader agreement of PI-QUAL [1, 22, 27], future studies should include the readings from at least two experts as a reference standard.
Another may be the limitation of “one test for all,” as we noted that our participants are diverse, and it may be wise to consider tailoring the PI-QUAL assessment to fit the experience and needs of the different groups. Clearly, radiologists will assess a study with a view to interpretation, whereas urologists will assess quality to determine how valid is the result. We believe that future courses like this should be encouraged.
It should be noted that the PI-QUAL primer [10] was conceived to be used both by clinicians (whose main task is to rule in and rule out the presence of clinically significant prostate cancer, and to target the lesions at biopsy) and by physicists, computer scientists, and radiographers who are involved in the acquisition of adequate prostate MR images at different levels (i.e., from setting up the machine to positioning the patient and injecting intravenous contrast at the right time and speed).
It is crucial to reduce the variability in the conduction and quality of prostate MRI so that clinicians can be confident to use it in the prostate diagnosis and treatment pathways, and although there is plenty of useful teaching material on prostate MRI for self-learning available online, the results from our pilot study reiterate the importance of dedicated hands-on training courses for the evaluation of prostate MR image quality.
In conclusion, we believe that a combination of simultaneous lectures and practical workshops can educate and improve the application of PI-QUAL for prostate MRI.
Also, we hope that our initial results from this teaching fellowship, along with those from the other experience [28], represent fertile ground for the widespread use of such courses for other initiatives and that this paper could act as a source of inspiration for future applicants.
Abbreviations
- AUC:
-
Area under the curve
- CI:
-
Confidence intervals
- COVID-19:
-
Coronavirus disease 19
- DICOM:
-
Digital Imaging and Communications in Medicine
- ESOR:
-
European School of Radiology
- ESUI:
-
European association of urology Section of Urologic Imaging
- ESUR:
-
European Society of Urogenital Radiology
- mpMRI:
-
Multiparametric magnetic resonance imaging
- PI-QUAL:
-
Prostate Imaging QUALity
- PI-RADS:
-
Prostate Imaging Reporting and Data System
- ROC:
-
Receiver operating characteristic
References
Karanasios E, Caglic I, Zawaideh JP, Barrett TL (2022) Prostate MRI quality: clinical impact of the PI-QUAL score in prostate cancer diagnostic work-up. Br J Radiol 1;95(1133):20211372. https://doi.org/10.1259/bjr.20211372
Weinreb JC, Barentsz JO, Choyke PL et al (2016) PI-RADS prostate imaging-reporting and data system: 2015, Version 2. Eur Urol 69(1):16–40
Turkbey B, Rosenkrantz AB, Haider MA et al (2019) Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol 0232:1–12
De Rooij M, Israël B, Tummers M et al (2020) ESUR / ESUI consensus statements on multi-parametric MRI for the detection of clinically significant prostate cancer: quality requirements for image acquisition, interpretation, and radiologists’ training. Eur Radiol 30(10):5404–5416
Brizmohun Appayya M, Adshead J, Ahmed H et al (2018) National implementation of multi-parametric MRI for prostate cancer detection - recommendations from a UK consensus meeting. BJU Int 122(1):13–25
Giganti F, Allen C, Emberton M, Moore CM, Kasivisvanathan V (2020) Prostate Imaging Quality (PI-QUAL): a new quality control scoring system for multiparametric magnetic resonance imaging of the prostate from the PRECISION trial. Eur Urol Oncol 3(5):615–619
Akin O, Riedl CC, Ishill NM, Moskowitz CS, Zhang J, Hricak H (2010) Interactive dedicated training curriculum improves accuracy in the interpretation of MR imaging of prostate cancer. Eur Radiol 20:995–1002
Rosenkrantz AB, Ayoola A, Hoffman D et al (2017) The learning curve in prostate MRI Interpretation: self-directed learning versus continual reader feedback. AJR Am J Roentgenol 208(3):W92–W100
Burn PR, Freeman SJ, Andreou A, Burns-Cox N, Persad R, Barrett T (2019) A multicentre assessment of prostate MRI quality and compliance with UK and international standards. Clin Radiol 74(11):894.e19–894.e25
Giganti F, Kirkham A, Kasivisvanathan V et al (2021) Understanding PI-QUAL for prostate MRI quality: a practical primer for radiologists. Insights Imaging 12(1):59
Obuchowski NA (1995) Multireader, multimodality receiver operating characteristic curve studies: hypothesis testing and sample size estimation using an analysis of variance approach with dependent observations. Acad Radiol 2:S22–S29 discussion S57-64, S70-1 pas
Liu W, Pantoja-Galicia N, Zhang B et al (2017) Generalized linear mixed models for multi-reader multi-case studies of diagnostic tests. Stat Methods Med Res 26:1373–1388
Kaasalainen T, Kivistö S, Holmström M et al (2016) Cardiac MRI in patients with cardiac pacemakers: practical methods for reducing susceptibility artifacts and optimizing image quality. Acta Radiol 57(2):178–187
Rosenkrantz AB, Patel JM, Babb JS, Storey P, Hecht EM (2010) Liver MRI at 3 T using a respiratory-triggered time-efficient 3D T2-weighted technique: impact on artifacts and image quality. AJR Am J Roentgenol 194(3):634–641
Lunden L, Wolff S, Sönke P et al (2020) MRI in patients with implanted active devices: how to combine safety and image quality using a limited transmission field? Eur Radiol 30(5):2571–2582
Ruiz-Flores L, Whitman GJ, Carissa Le-Petross HT, Hess KR, Parikh JR (2020) Variation in Technical Quality of Breast MRI. Acad Radiol 27(4):468–475
Linver MN, Paster SB, Rosenberg RD, Key CR, Stidley CA, King WV (1992) Improvement in mammography interpretation skills in a community radiology practice after dedicated teaching courses: 2-year medical audit of 38,633 cases. Radiology 184(1):39–43
Kasivisvanathan V, Ambrosi A, Giganti F et al (2019) A dedicated prostate MRI teaching course improves the ability of the urologist to interpret clinically significant prostate cancer on multiparametric MRI. Eur Urol 75(1):203–204
Padhani AR, Schoots I, Turkbey B, Giannarini G, Barentsz JO (2021) A multifaceted approach to quality in the MRI-directed biopsy pathway for prostate cancer diagnosis. Eur Radiol 31(6):4386–4389
Arnoldner MA, Polanec SH, Lazar M et al (2022) Rectal preparation significantly improves prostate imaging quality: assessment of the PI-QUAL score with visual grading characteristics. Eur J Radiol 147:110145
Boschheidgen M, Ullrich T, Blondin D et al (2021) Comparison and prediction of artefact severity due to total hip replacement in 1.5T versus 3T MRI of the prostate. Eur J Radiol 144:109949
Giganti F, Dinneen E, Kasivisvanathan V et al (2022) Inter-reader agreement of the PI-QUAL score for prostate MRI quality in the NeuroSAFE PROOF trial. Eur Radiol 32(2):879–889
De Rooij M, Barentsz JO (2022) PI-QUAL v. 1: the first step towards good-quality prostate MRI. Eur Radiol 32(2):876–878
Turkbey B (2022) Better image quality for diffusion-weighted MRI of the prostate using deep learning. Radiology 303(2):382–383. https://doi.org/10.1148/radiol.212078
Turkbey B, Choyke PL (2020) PI-QUAL, a new system for evaluating prostate magnetic resonance imaging quality: is beauty in the eye of the beholder? Eur Urol Oncol 3(5):620–621
Giannarini G, Valotto C, Girometti R, Dal Moro F, Briganti A, Padhani AR (2021) Measuring the quality of diagnostic prostate magnetic resonance imaging: a urologist’s perspective. Eur Urol 79(4):440–441
Girometti R, Blandino A, Zichichi C et al (2022) Inter-reader agreement of the Prostate Imaging Quality (PI-QUAL) score: a bicentric study. Eur J Radiol 150:110267. https://doi.org/10.1016/j.ejrad.2022.110267
Giganti F, Aupin L, Thoumin C et al (2022) Promoting the use of the PRECISE score for prostate MRI during active surveillance: results from the ESOR Nicholas Gourtsoyiannis teaching fellowship. Insights Imaging. https://doi.org/10.1186/s13244-022-01252-1
Acknowledgements
The authors would like to thank Professor Valérie Vilgrain (ESOR Scientific / Educational Director), Ms. Brigitte Lindlbauer (ESOR Administrative Director), Mrs. Isabella Davicino (ESOR Scholarship/Fellowship Coordinator), and the whole ESOR team for their support.
Funding
This study has received funding from the European School of Radiology (ESOR) 2021 Nicholas Gourtsoyiannis teaching fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Francesco Giganti.
Conflict of interest
The authors of this manuscript declare relationships with the following companies:
FG is a recipient of the 2020 Young Investigator Award (20YOUN15) funded by the Prostate Cancer Foundation / CRIS Cancer Foundation. FG has been the recipient of the 2021 ESOR Nicholas Gourtsoyiannis teaching fellowship.
APC is supported by Pfizer and the American Cancer Society.
LGB reports consulting fees from Delfina outside of the submitted work and research funding from the Office of Scholarly Engagement at Harvard Medical School.
VK is an Academic Clinical Lecturer funded by the UK National Institute for Health Research (NIHR).
AK is supported by the UCLH/UCL Biomedical Research Centre.
ME receives research support from the United kingdom’s National Institute of Health Research (NIHR) UCLH and UCL Biomedical Research Centre.
CMM is supported by the UKNIHR, Movember, PCUK, and the EAU Research Foundation.
CMT receives NIH research funding (EB 028741 and EB 025823) and is a medical advisor for Profound Medical, Medscape and Promaxo.
Statistics and biometry
One of the authors (AA) has significant statistical expertise.
Informed consent
All patients gave written informed consent.
Ethical approval
All patients included in this report gave written informed consent to have their images used for research and teaching purposes. No IRB approval was needed for this study.
Methodology
• retrospective
• experimental
• multi-centre study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 34 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Giganti, F., Cole, A.P., Fennessy, F.M. et al. Promoting the use of the PI-QUAL score for prostate MRI quality: results from the ESOR Nicholas Gourtsoyiannis teaching fellowship. Eur Radiol 33, 461–471 (2023). https://doi.org/10.1007/s00330-022-08947-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08947-5