Abstract
Objectives
3D chemical shift–encoded (CSE) MRI enables accurate and precise quantification of proton density fat fraction (PDFF) and R2*, biomarkers of hepatic fat and iron deposition. Unfortunately, 3D CSE-MRI requires reliable breath-holding. Free-breathing 2D CSE-MRI with sequential radiofrequency excitation is a motion-robust alternative but suffers from low signal-to-noise-ratio (SNR). To overcome this limitation, this work explores the combination of flip angle–modulated (FAM) 2D CSE imaging with a non-local means (NLM) motion-corrected averaging technique.
Methods
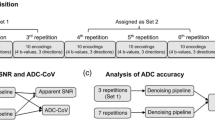
In this prospective study, 35 healthy subjects (27 children/8 adults) were imaged on a 3T MRI-system. Multi-echo 3D CSE (“3D”) and 2D CSE FAM (“FAM”) images were acquired during breath-hold and free-breathing, respectively, to obtain PDFF and R2* maps of the liver. Multi-repetition FAM was postprocessed with direct averaging (DA)– and NLM-based averaging and compared to 3D CSE using Bland-Altmann and regression analysis. Image qualities of PDFF and R2* maps were reviewed by two radiologists using a Likert-like scale (score 1–5, 5 = best).
Results
Compared to 3D CSE, multi-repetition FAM-NLM showed excellent agreement (regression slope = 1.0, R2 = 0.996) for PDFF and good agreement (regression slope 1.08–1.15, R2 ≥ 0.899) for R2*. Further, multi-repetition FAM-NLM PDFF and R2* maps had fewer artifacts (score 3.8 vs. 3.2, p < 0.0001 for PDFF; score 3.2 vs. 2.6, p < 0.001 for R2*) and better overall image quality (score 4.0 vs. 3.5, p < 0.0001 for PDFF; score 3.4 vs. 2.7, p < 0.0001 for R2*).
Conclusions
Free-breathing FAM-NLM provides superior image quality of the liver compared to the conventional breath-hold 3D CSE-MRI, while minimizing bias for PDFF and R2* quantification.
Key Points
• 2D CSE FAM-NLM is a free-breathing method for liver fat and iron quantification and viable alternative for patients unable to hold their breath.
• 2D CSE FAM-NLM is a feasible alternative to breath-hold 3D CSE methods, with low bias in proton density fat fraction (PDFF) and no clinically significant bias in R2*.
• Quantitatively, multiple repetitions in 2D CSE FAM-NLM lead to improved SNR.





Similar content being viewed by others
Abbreviations
- CSE:
-
Chemical shift–encoded
- DA:
-
Direct averaging
- FAM:
-
Flip angle modulation
- NLM:
-
Non-local means
- PDFF:
-
Proton density fat fraction
- REP:
-
Repetition
- SNR:
-
Signal-to-noise ratio
References
Reeder SB, Cruite I, Hamilton G, Sirlin CB (2011) Quantitative assessment of liver fat with magnetic resonance imaging and spectroscopy. J Magn Reson Imaging 34:729–749
Yokoo T, Serai SD, Pirasteh A et al (2018) Linearity, bias, and precision of hepatic proton density fat fraction measurements by using MR imaging: a meta-analysis. Radiology 286:486–498
Reeder SB, Hu HH, Sirlin CB (2012) Proton density fat-fraction: a standardized MR-based biomarker of tissue fat concentration. J Magn Reson Imaging 36:1011–1014
Caussy C, Reeder SB, Sirlin CB, Loomba R (2018) Noninvasive, quantitative assessment of liver fat by MRI-PDFF as an endpoint in NASH trials. Hepatology 68:763–772
Younossi ZM, Koenig AB, Abdelatif D et al (2016) Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64:73–84
Hernando D, Levin YS, Sirlin CB, Reeder SB (2014) Quantification of liver iron with MRI: State of the art and remaining challenges. J Magn Reson Imaging 40:1003–1021
Kühn J-P, Hernando D, Muñoz del Rio A et al (2012) Effect of multipeak spectral modeling of fat for liver iron and fat quantification: correlation of biopsy with MR imaging results. Radiology 265:133–142
Starekova J, Reeder SB (2020) Liver fat quantification: where do we stand? Abdom Radiol (NY) 45:3386–3399
Zhao R, Zhang Y, Wang X et al (2020) Motion-robust, high-SNR liver fat quantification using a 2D sequential acquisition with a variable flip angle approach. Magn Reson Med 84:2004–2017
Motosugi U, Hernando D, Bannas P et al (2015) Quantification of liver fat with respiratory-gated quantitative chemical shift encoded MRI. J Magn Reson Imaging 42:1241–1248
Armstrong T, Dregely I, Stemmer A et al (2018) Free-breathing liver fat quantification using a multiecho 3D stack-of-radial technique. Magn Reson Med 79:370–382
Luo H, Zhu A, Wiens CN et al (2021) Free-breathing liver fat and quantification using motion-corrected averaging based on a nonlocal means algorithm. Magn Reson Med 85:653–666
Moriguchi H, Lewin JS, Duerk JL (2003) Dixon techniques in spiral trajectories with off-resonance correction: a new approach for fat signal suppression without spatial-spectral RF pulses. Magn Reson Med 50:915–924
Börnert P, Koken P, Eggers H (2010) Spiral water-fat imaging with integrated off-resonance correction on a clinical scanner. J Magn Reson Imaging 32:1262–1267
Pipe JG (1999) Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 42:963–969
Moran CJ, Brodsky EK, Bancroft LH et al (2014) High-resolution 3D radial bSSFP with IDEAL. Magn Reson Med 71:95–104
Hernando D, Sharma SD, Aliyari Ghasabeh M et al (2017) Multisite, multivendor validation of the accuracy and reproducibility of proton-density fat-fraction quantification at 1.5 T and 3T using a fat-water phantom. Magn Reson Med 77:1516–1524
Liu CY, McKenzie CA, Yu H et al (2007) Fat quantification with IDEAL gradient echo imaging: correction of bias from T1 and noise. Magn Reson Med 58:354–364
Pooler BD, Hernando D, Ruby JA et al (2018) Validation of a motion-robust 2D sequential technique for quantification of hepatic proton density fat fraction during free breathing. J Magn Reson Imaging 48:1578–1585
Rehm JL, Wolfgram PM, Hernando D et al (2015) Proton density fat-fraction is an accurate biomarker of hepatic steatosis in adolescent girls and young women. Eur Radiol 25:2921–2930
di Martino M, Pacifico L, Bezzi M et al (2016) Comparison of magnetic resonance spectroscopy, proton density fat fraction and histological analysis in the quantification of liver steatosis in children and adolescents. World J Gastroenterol 22:8812–8819
Kwee TC, Takahara T, Koh DM et al (2008) Comparison and reproducibility of ADC measurements in breathhold, respiratory triggered, and free-breathing diffusion-weighted MR imaging of the liver. J Magn Reson Imaging 28:1141–1148
Hamilton G, Middleton MS, Hooker JC et al (2015) In vivo breath-hold 1H MRS simultaneous estimation of liver proton density fat fraction, and T1 and T2 of water and fat, with a multi-TR, multi-TE sequence. J Magn Reson Imaging 42:1538–1543
Hernando D, Hamilton G, Roldan-Alzate A, Reeder SB (2014) Fully automated processing of multi-echo spectroscopy data for liver fat quantification. . In Proceedings of the Annual Meeting of the International Society for Magnetic Resonance in Medicine, Milan(10-16 May), Abstract 2884
Hines CDG, Frydrychowicz A, Hamilton G et al (2011) T1 independent, T2* corrected chemical shift-based fat-water separation with multi-peak fat spectral modeling is an accurate and precise measure of hepatic steatosis. J Magn Reson Imaging 33:873–881
Holdsworth SJ, MacPherson SJ, Yeom KW et al (2018) Clinical evaluation of silent T1-weighted MRI and silent MR angiography of the brain. AJR Am J Roentgenol 210:404–411
Kenkel D, Barth BK, Piccirelli M et al (2017) Simultaneous multislice diffusion-weighted imaging of the kidney. Invest Radiol 52:163–169
Campo CA, Hernando D, Schubert T et al (2017) Standardized approach for ROI-based measurements of proton density fat fraction and R2* in the liver. AJR Am J Roentgenol 209:592–603
Fernandez-Seara MA, Wehrli FW (2000) Postprocessing technique to correct for background gradients in image-based R*(2) measurements. Magn Reson Med 44:358–366
Hernando D, Vigen KK, Shimakawa A, Reeder SB (2012) R2* mapping in the presence of macroscopic B0 field variations. Magn Reson Med 68:830–840
Zhong X, Armstrong T, Nickel MD et al (2020) Effect of respiratory motion on free-breathing 3D stack-of-radial liver R*2 relaxometry and improved quantification accuracy using self-gating. Magn Reson Medicine 83:1964–1978
Armstrong T, Ly Kv., Ghahremani S, et al (2019) Free-breathing 3-D quantification of infant body composition and hepatic fat using a stack-of-radial magnetic resonance imaging technique. Pediatric Radiology 49:876–888
Rohani SC, Morin CE, Zhong X et al (2021, 2021) Hepatic iron quantification using a free-breathing 3D radial gradient echo technique and validation with a 2D biopsy-calibrated R2* relaxometry method. J Magn Reson Imaging. https://doi.org/10.1002/jmri.27921
Doneva M, Börnert P, Eggers H et al (2010) Compressed sensing for chemical shift-based water-fat separation. Magn Reson Med 64:1749–1759
Noureddin M, Lam J, Peterson MR et al (2013) Utility of magnetic resonance imaging versus histology for quantifying changes in liver fat in nonalcoholic fatty liver disease trials. Hepatology 58:1930–1940
Kim B, Kim SY, Kim KW et al (2018) MRI in donor candidates for living donor liver transplant: technical and practical considerations. J Magn Reson Imaging 48:1453–1467
Acknowledgements
The authors thank David T Harris, PhD, for his assistance with the organization and recruitment.
Funding
The authors wish to acknowledge support from GE Healthcare and Bracco Diagnostics who provide research support to the University of Wisconsin, and support from the NIH (K24 DK102595, R01 DK088925, R01 DK100651, R44-EB025729, R01-DK117354). Dr. Reeder is a Romnes Faculty Fellow, and has received an award provided by the University of Wisconsin-Madison Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation. All funding was in compliance with ethical standards.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Diego Hernando, PhD.
Conflicts of interest
The authors of this manuscript declare relationships with the following companies unrelated to this work: SBR has ownership interests in Calimetrix, Reveal Pharmaceuticals, Elucent Medical, Cellectar Biosciences, and HeartVista; DH has ownership interests in Calimetrix. SAW is a paid consultant for Ethicon Inc. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethics approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
All of the subjects used in this manuscript were reported in a previous manuscript (https://pubmed.ncbi.nlm.nih.gov/32243665/) focused on the development of FAM-based fat quantification. However, the previous manuscript used separate FAM acquisitions obtained on these subjects, as well as different image processing and analysis.
Methodology
• prospective
• prospective cohort study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 446 kb)
Rights and permissions
About this article
Cite this article
Starekova, J., Zhao, R., Colgan, T.J. et al. Improved free-breathing liver fat and iron quantification using a 2D chemical shift–encoded MRI with flip angle modulation and motion-corrected averaging. Eur Radiol 32, 5458–5467 (2022). https://doi.org/10.1007/s00330-022-08682-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08682-x