Abstract
Objectives
To evaluate the accuracies of simultaneous 18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging ([18F]-FDG PET/MRI) in preoperative localization and the postsurgical prediction.
Methods
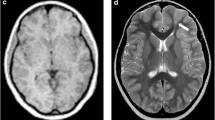
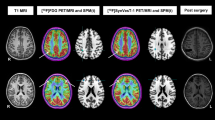
This retrospective study was performed on ninety-eight patients diagnosed with refractory epilepsy whose presurgical evaluation included [18F]-FDG PET/MRI, with 1-year post-surgery follow-up between August 2016 and December 2018. PET/MRI images were interpreted by two radiologists and a nuclear medicine physician to localize the EOZ using standard visual analysis and asymmetry index based on standard uptake value (SUV). The localization accuracy and predictive performance of simultaneous 18F-FDG PET/MRI based on the surgial pathology and postsurgical outcome were evaluated.
Results
A total of 41.8% (41/98) patients were found to have a definitely structural abnormality on the MR portion of PET/MRI; 93.9% (92/98) were shown hypometabolism on the PET portion of the hybrid PET/MRI. PET/MRI identified 18 cases with subtle structural abnormalities on MRI re-read. Six percent (6/98) of patients PET/MRI were negative. A total of 65.3% (64/98) patients showed seizure-free at 1-year follow-up after epilepsy surgery. The sensitivity, specificity, and accuracy of [18F]-FDG PET/MRI was 95.3%, 8.8%, and 65.3% for seizure onset localization based on surgical pathology and postsurgical outcome, respectively. Multivariate regression analysis indicated that concordant of EOZ localization between PET/MRI and surgical resection range, which was a good positive predictor of seizure freedom (Engel I) (OR = 14.741, 95% CI 3.934–55.033, p < 0.001).
Conclusions
[18F]-FDG PET/MRI used as two combined modalities providing additional sensitivity when detecting possible epileptic foci and will probably improve the surgical outcome.
Key Points
• Sensitivity, specificity, and accuracy of [18F]-FDG PET/MRI were 95.3%, 8.8%, and 65.3% for seizure onset localization based on surgical pathology and postsurgical outcome, respectively.
• Concordance of EOZ localization between PET/MRI and surgical resection range was a good positive predictor of seizure freedom; presurgical [ 18 F] -FDG PET/MRI will probably improve the surgical outcome.




Similar content being viewed by others
Abbreviations
- [18F]-FDG PET/MRI:
-
18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging
- AI:
-
Asymmetry index
- CD:
-
Cortical dysplasia
- CI:
-
Confidence interval
- EOZ:
-
Epileptogenic onset zone
- FCD:
-
Focal cortical dysplasia
- HS:
-
Hippocampus sclerosis
- OR:
-
Odds ratio
- SVA:
-
Standard visual analysis
- TSC:
-
Tuberous sclerosis complex
References
Thijs RD, Surges R, O'Brien TJ, Sander JW (2019) Epilepsy in adults. Lancet 393:689–701. https://doi.org/10.1016/S0140-6736(18)32596-0
Duncan JS, Sander JW, Sisodiya SM, Walker MC (2006) Adult epilepsy. Lancet 367:1087–1100. https://doi.org/10.1016/S0140-6736(06)68477-8
Widjaja E, Jain P, Demoe L, Guttmann A, Tomlinson G, Sander B (2020) Seizure outcome of pediatric epilepsy surgery: systematic review and meta-analyses. Neurology 94:311–321. https://doi.org/10.1212/WNL.0000000000008966
Spencer S, Huh L (2008) Outcomes of epilepsy surgery in adults and children. Lancet Neurol 7:525–537. https://doi.org/10.1016/S1474-4422(08)70109-1
Oldan JD, Shin HW, Khandani AH, Zamora C, Benefield T, Jewells V (2018) Subsequent experience in hybrid PET-MRI for evaluation of refractory focal onset epilepsy. Seizure 61:128–134. https://doi.org/10.1016/j.seizure.2018.07.022
Tellez-Zenteno JF, Hernandez RL, Moien-Afshari F, Wiebe S (2010) Surgical outcomes in lesional and non-lesional epilepsy: a systematic review and meta analysis. https://doi.org/10.1016/j.eplepsyres.2010.02.007
Rathore C, Dickson JC, Teotónio R, Ell P, Duncan JS (2014) The utility of 18F-fluorodeoxyglucose PET (FDG PET) in epilepsy surgery. Epilepsy Res 108:1306–1314. https://doi.org/10.1016/j.eplepsyres.2014.06.012
Shaikh Z, Torres A, Takeoka M (2019) Neuroimaging in pediatric epilepsy. Brain Sci 9:190. https://doi.org/10.3390/brainsci9080190
Tomás J, Pittau F, Hammers A et al (2019) The predictive value of hypometabolism in focal epilepsy: a prospective study in surgical candidates. Eur J Nucl Med Mol Imaging 46:1806–1816. https://doi.org/10.1007/s00259-019-04356-x
LoPinto-Khoury C, Sperling MR, Skidmore C et al (2012) Surgical outcome in PET-positive, MRI-negative patients with temporal lobe epilepsy. Epilepsia 53:342–348. https://doi.org/10.1111/j.1528-1167.2011.03359.x
Carne RP, O'Brien TJ, Kilpatrick CJ et al (2004) MRI-negative PET-positive temporal lobe epilepsy: a distinct surgically remediable syndrome. Brain 127(Pt 10):2276–2285. https://doi.org/10.1093/brain/awh257
Chassoux F, Rodrigo S, Semah F et al (2010) FDG-PET improves surgical outcome in negative MRI Taylor-type focal cortical dysplasias. Neurology 75:2168–2175. https://doi.org/10.1212/WNL.0b013e31820203a9
Werner P, Barthel H, Drzezga A, Sabri O (2015) Current status and future role of brain PET/MRI in clinical and research settings. Eur J Nucl Med Mol Imaging 42:512–526. https://doi.org/10.1007/s00259-014-2970-9
Wieser HG, Blume WT, Fish D et al (2001) ILAE Commission Report. Proposal for a new classification of outcome with respect to epileptic seizures following epilepsy surgery. Epilepsia 2:282–286
von Oertzen J, Urbach H, Jungbluth S et al (2002) Standard MRI is inadequate for patients with refractory focal epilepsy. J Neurol Neurosurg Psychiatry 73:643–647. https://doi.org/10.1136/jnnp.73.6.643
Bien CG, Szinay M, Wagner J, Clusmann H, Becker AJ, Urbach H (2009) Characteristics and surgical outcomes of patients with refractory magnetic resonance imaging-negative epilepsies. Arch Neurol 66:1491–1499. https://doi.org/10.1001/archneurol.2009.283
S Fernández, A. Donaire , E Serès et al (2015) PET/MRI and PET/MRI/SISCOM coregistration in the pre-surgical evaluation of refractory focal epilepsy. Epilepsy Res 111: 1-9. https://doi.org/10.1016/j.eplepsyres.2014.12.011
Desarnaud S, Mellerio C, Semah F et al (2018) 18F-FDG PET in drug-resistant epilepsy due to focal cortical dysplasia type 2: additional value of electroclinical data and coregistration with MRI. Eur J Nucl Med Mol Imaging 45:1449–1460. https://doi.org/10.1007/s00259-018-3994-3
Garibotto V, Heinzer S, Vulliemoz S et al (2013) Clinical applications of hybrid PET/MRI in neuroimaging. Clin Nucl Med 38:e13–e18. https://doi.org/10.1097/RLU.0b013e3182638ea6
Yerys BE, Jankowski KF, Shook D, Rosenberger LR, Barnes KA, Berl MM (2009) The fMRI success rate of children and adolescents: typical development, epilepsy, attention deficit/hyperactivity disorder, and autism spectrum disorders. Hum Brain Mapp 30:3426–3435. https://doi.org/10.1002/hbm.20767
Grouiller F, Delattre B, Pittau F et al (2015) All-in one interictal presurgical imaging in patients with epilepsy: single –session EEG/PET/(f)MRI. Eur J Nucl Med Mol Imaging 42:1133–1143. https://doi.org/10.1007/s00259-015-3045-2
Ormond DR, Clusmann H, Sassen R et al (2019) Pediatric temporal lobe epilepsy surgery in bonn and review of the literature. Neurosurgery 2019(84):844–856. https://doi.org/10.1093/neuros/nyy125
Bonini F, McGonigal A, Scavarda D et al (2018) Predictive factors of surgical outcome in frontal lobe epilepsy explored with stereoelectroencephalography. Neurosurgery 2018(83):217–225. https://doi.org/10.1093/neuros/nyx342
Salamon N, Kung J, Shaw SJ et al (2008) FDG-PET co-registration improves detection of cortical dysplasia in patients with epilepsy. Neurology 71:1594–1601. https://doi.org/10.1212/01.wnl.0000334752.41807.2f
Chassoux F, Rodrigo S, Semah F et al (2010) FDG-PET improves surgical outcome in negative MRI Taylor-type focal cortical dysplasias. Neurology 75:2168–2175. https://doi.org/10.1212/WNL.0b013e31820203a9
Kikuchi K, Togao O, Yamashita K et al (2020) Diagnostic accuracy for the epileptogenic zone detection in focal epilepsy could be higher in FDG-PET/MRI than in FDG-PET/CT. Eur Radiol. https://doi.org/10.1007/s00330-020-07389-1
Funding
This study was supported by the Project of Beijing Municipal Administration of Hospital’s Ascent Plan, Code:DFL 20180802.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jie Lu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
-
retrospective
-
diagnostic or prognostic study
-
performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guo, K., Cui, B., Shang, K. et al. Assessment of localization accuracy and postsurgical prediction of simultaneous 18F-FDG PET/MRI in refractory epilepsy patients. Eur Radiol 31, 6974–6982 (2021). https://doi.org/10.1007/s00330-021-07738-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-07738-8