Abstract
Objectives
To assess the performance of gadoxetate dynamic contrast–enhanced (DCE) MRI of the liver and spleen for noninvasive diagnosis of portal hypertension (PH).
Methods
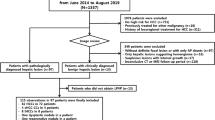
Thirty-five patients (M/F 22/13, mean age 55 years) with chronic liver disease who underwent hepatic venous pressure gradient (HVPG) measurements were prospectively enrolled in this IRB-approved study. All patients underwent multiparametric MRI including gadoxetate DCE-MRI acquisition. Model-based and model-free DCE-MRI analyses were performed. The correlation between DCE-MRI parameters and HVPG was assessed. ROC analysis was employed to determine the diagnostic performance of DCE-MRI parameters alone and in combination for prediction of PH and clinically significant (CS)PH (HVPG > 5 and ≥ 10 mmHg, respectively).
Results
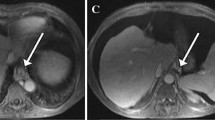
Mean HVPG was 7.0 ± 5.0 mmHg (range 0–18 mmHg). Twenty-one (60%) patients had PH, of whom 9 had CSPH. Modeled liver uptake fraction fi and uptake rate ki and model-free parameters liver upslope and uptake were all significantly negatively correlated with HVPG (r range − 0.490 to − 0.398, p value range 0.003–0.018), while spleen interstitial fraction ve was significantly positively correlated with HVPG (r = 0.336, p = 0.048). For PH diagnosis, liver ki showed the best diagnostic performance with an AUC, sensitivity, and specificity of 0.74 (confidence interval (CI) 0.57–0.91), 71.4%, and 78.6%. The combination of liver ki and spleen ve was selected as the best classifier for diagnosis of CSPH with an AUC, sensitivity, and specificity of 0.87 (CI 0.75–0.99), 100%, and 73.1%.
Conclusions
Our results demonstrate the potential utility of hepatocyte uptake parameters and spleen interstitial fraction obtained with gadoxetate DCE-MRI for the diagnosis of PH and CSPH.
Key Points
• Liver uptake and spleen interstitial fraction estimates from gadoxetate DCE-MRI are significantly correlated with portal pressure measurements.
• Liver uptake rate shows good diagnostic performance for the diagnosis of portal hypertension.
• The combination of liver uptake rate with spleen interstitial fraction exhibits excellent diagnostic performance for the diagnosis of clinically significant portal hypertension.



Similar content being viewed by others
Abbreviations
- ART:
-
Arterial fraction
- CPA:
-
Collagen proportionate area
- CSPH:
-
Clinically significant portal hypertension
- DCE-MRI:
-
Dynamic contrast–enhanced MRI
- F a :
-
Arterial flow
- f i :
-
Uptake fraction
- F p :
-
Portal flow
- F t :
-
Total flow
- HVPG:
-
Hepatic venous pressure gradient
- k i :
-
Intracellular uptake rate
- MTT:
-
Mean transit time
- PH:
-
Portal hypertension
- ROI:
-
Region of interest
- SI:
-
Signal intensity
- TTP:
-
Time to peak
- v e :
-
Interstitial volume fraction
References
Bosch J, Garcia-Pagan JC (2000) Complications of cirrhosis. I. Portal hypertension. J Hepatol 32:141–156
Turco L, Garcia-Tsao G (2019) Portal hypertension: pathogenesis and diagnosis. Clin Liver Dis 23:573–587
de Franchis R, Baveno VF (2010) Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol 53:762–768
Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J (2017) Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 65:310–335
Qi X, Berzigotti A, Cardenas A, Sarin SK (2018) Emerging non-invasive approaches for diagnosis and monitoring of portal hypertension. Lancet Gastroenterol Hepatol 3:708–719
Elkrief L, Rautou PE, Ronot M et al (2015) Prospective comparison of spleen and liver stiffness by using shear-wave and transient elastography for detection of portal hypertension in cirrhosis. Radiology 275:589–598
Kim TY, Jeong WK, Sohn JH, Kim J, Kim MY, Kim Y (2015) Evaluation of portal hypertension by real-time shear wave elastography in cirrhotic patients. Liver Int 35:2416–2424
You MW, Kim KW, Pyo J et al (2017) A meta-analysis for the diagnostic performance of transient elastography for clinically significant portal hypertension. Ultrasound Med Biol 43:59–68
Ronot M, Lambert S, Elkrief L et al (2014) Assessment of portal hypertension and high-risk oesophageal varices with liver and spleen three-dimensional multifrequency MR elastography in liver cirrhosis. Eur Radiol 24:1394–1402
Wagner M, Hectors S, Bane O et al (2018) Noninvasive prediction of portal pressure with MR elastography and DCE-MRI of the liver and spleen: preliminary results. J Magn Reson Imaging 48:1091–1103
Choi SL, Lee ES, Ko A et al (2020) Technical success rates and reliability of spin-echo echo-planar imaging (SE-EPI) MR elastography in patients with chronic liver disease or liver cirrhosis. Eur Radiol 30:1730–1737
Wagner M, Corcuera-Solano I, Lo G et al (2017) Technical failure of MR elastography examinations of the liver: experience from a large single-center study. Radiology 284:401–412
Annet L, Materne R, Danse E, Jamart J, Horsmans Y, Van Beers BE (2003) Hepatic flow parameters measured with MR imaging and Doppler US: correlations with degree of cirrhosis and portal hypertension. Radiology 229:409–414
Dyvorne HA, Jajamovich GH, Bane O et al (2016) Prospective comparison of magnetic resonance imaging to transient elastography and serum markers for liver fibrosis detection. Liver Int 36:659–666
Bolognesi M, Merkel C, Sacerdoti D, Nava V, Gatta A (2002) Role of spleen enlargement in cirrhosis with portal hypertension. Dig Liver Dis 34:144–150
Mejias M, Garcia-Pras E, Gallego J, Mendez R, Bosch J, Fernandez M (2010) Relevance of the mTOR signaling pathway in the pathophysiology of splenomegaly in rats with chronic portal hypertension. J Hepatol 52:529–539
Sourbron S, Sommer WH, Reiser MF, Zech CJ (2012) Combined quantification of liver perfusion and function with dynamic gadoxetic acid-enhanced MR imaging. Radiology 263:874–883
Jajamovich GH, Dyvorne H, Donnerhack C, Taouli B (2014) Quantitative liver MRI combining phase contrast imaging, elastography, and DWI: assessment of reproducibility and postprandial effect at 3.0 T. PLoS One 9:e97355
Hectors SJ, Wagner M, Besa C et al (2016) Intravoxel incoherent motion diffusion-weighted imaging of hepatocellular carcinoma: is there a correlation with flow and perfusion metrics obtained with dynamic contrast-enhanced MRI? J Magn Reson Imaging 44:856–864
Hectors SJ, Bane O, Stocker D et al (2020) Splenic T1rho as a noninvasive biomarker for portal hypertension. J Magn Reson Imaging. https://doi.org/10.1002/jmri.27087
Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR (1999) Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol 94:2467–2474
Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24:289–293
Calvaruso V, Burroughs AK, Standish R et al (2009) Computer-assisted image analysis of liver collagen: relationship to Ishak scoring and hepatic venous pressure gradient. Hepatology 49:1236–1244
Verloh N, Probst U, Utpatel K et al (2019) Influence of hepatic fibrosis and inflammation: correlation between histopathological changes and Gd-EOB-DTPA-enhanced MR imaging. PLoS One 14:e0215752
Verloh N, Utpatel K, Haimerl M et al (2015) Liver fibrosis and Gd-EOB-DTPA-enhanced MRI: a histopathologic correlation. Sci Rep 5:15408
Georgiou L, Penny J, Nicholls G et al (2017) Quantitative assessment of liver function using gadoxetate-enhanced magnetic resonance imaging: monitoring transporter-mediated processes in healthy volunteers. Invest Radiol 52:111–119
Asenbaum U, Ba-Ssalamah A, Mandorfer M et al (2017) Effects of portal hypertension on gadoxetic acid-enhanced liver magnetic resonance: diagnostic and prognostic implications. Invest Radiol 52:462–469
Tamada T, Ito K, Higaki A et al (2011) Gd-EOB-DTPA-enhanced MR imaging: evaluation of hepatic enhancement effects in normal and cirrhotic livers. Eur J Radiol 80:e311–e316
McConnell M, Iwakiri Y (2018) Biology of portal hypertension. Hepatol Int 12:11–23
Aronhime S, Calcagno C, Jajamovich GH et al (2014) DCE-MRI of the liver: effect of linear and nonlinear conversions on hepatic perfusion quantification and reproducibility. J Magn Reson Imaging 40:90–98
Berzigotti A, Ashkenazi E, Reverter E, Abraldes JG, Bosch J (2011) Non-invasive diagnostic and prognostic evaluation of liver cirrhosis and portal hypertension. Dis Markers 31:129–138
Luetkens JA, Klein S, Traber F et al (2018) Quantification of liver fibrosis at T1 and T2 mapping with extracellular volume fraction MRI: preclinical results. Radiology 288:748–754
Levick C, Phillips-Hughes J, Collier J et al (2019) Non-invasive assessment of portal hypertension by multi-parametric magnetic resonance imaging of the spleen: a proof of concept study. PLoS One 14:e0221066
Jajamovich GH, Calcagno C, Dyvorne HA, Rusinek H, Taouli B (2014) DCE-MRI of the liver: reconstruction of the arterial input function using a low dose pre-bolus contrast injection. PLoS One 9:e115667
Feng L, Axel L, Chandarana H, Block KT, Sodickson DK, Otazo R (2016) XD-GRASP: golden-angle radial MRI with reconstruction of extra motion-state dimensions using compressed sensing. Magn Reson Med 75:775–788
Qiu W, Li D, Jin X et al (2019) Sliding motion compensated low-rank plus sparse (SMC-LS) reconstruction for high spatiotemporal free-breathing liver 4D DCE-MRI. Magn Reson Imaging 58:56–66
Nalepa J, Ribalta Lorenzo P, Marcinkiewicz M et al (2020) Fully-automated deep learning-powered system for DCE-MRI analysis of brain tumors. Artif Intell Med 102:101769
Funding
This research was supported by NIDDK grant R01DK113272.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Bachir Taouli.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Twenty-five of the included patients have been previously reported in Hectors et al Splenic T1ρ as a noninvasive biomarker for portal hypertension. J Magn Reson Imaging. doi: 10.1002/jmri.27087.
Methodology
• prospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hectors, S.J., Bane, O., Kennedy, P. et al. Noninvasive diagnosis of portal hypertension using gadoxetate DCE-MRI of the liver and spleen. Eur Radiol 31, 4804–4812 (2021). https://doi.org/10.1007/s00330-020-07495-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07495-0