Abstract
Objectives
To investigate biomechanical changes in lumbar disc herniations.
Methods
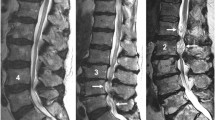
Patients with lumbar disc herniation verified on a 1.5–3-T magnetic resonance imaging (MRI) scanner were imaged in a weight-bearing 0.25-T MRI scanner in (1) standing position, (2) conventional supine position with relative lumbar flexion, and (3) supine position with a forced lumbar extension by adding a lumbar pillow. The L2-S1 lordosis angle, the disc cross-sectional area, the disc cross-sectional diameter, and the spinal canal cross-sectional diameter were measured for each position. Disc degeneration and nerve root compression were graded, and the pain intensity was reported during each scan position.
Results
Forty-three herniated discs in 37 patients (36.7 ± 11.9 years) were analyzed in each position. The L2-S1 lumbar angle increased in the standing position (mean difference [MD]: 5.61°, 95% confidence interval [95% CI]: 3.44 to 7.78) and with the lumbar pillow in the supine position (MD: 14.63°, 95% CI: 11.71 to 17.57), both compared with the conventional supine position. The herniated disc cross-sectional area and diameter increased during standing compared with during conventional supine position. No changes were found in the spinal canal cross-sectional diameter between positions. Higher nerve root compression grades for paracentral herniations were found during standing compared with during conventional supine position. This was neither found with a lumbar pillow nor for central herniations in any position compared with conventional supine.
Conclusion
Disc herniations displayed dynamic behavior with morphological changes in the standing position, leading to higher nerve root compression grades for paracentral herniated discs.
Key Points
• Lumbar herniated discs increased in size in the axial plane during standing.
• Increased nerve root compression grades for paracentral herniated discs were found during standing.
• Weight-bearing MRI may increase the diagnostic sensitivity of nerve root compression in lumbar disc herniations.



Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- FOV:
-
Field-of-view
- ICC:
-
Intra-class correlation coefficient
- LBP:
-
Low back pain
- MRI:
-
Magnetic resonance imaging
- NRS:
-
Numerical rating scale
- ODI:
-
Oswestry Disability Index
- PDQ:
-
Pain-Detect Questionnaire
References
Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Gabriel Rothman SL, Sze GK (2014) Lumbar disc nomenclature: version 2.0 Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J 14:2525–2545
McCall IW (2000) Lumbar Herniated Disks. Radiol Clin North Am 38:1293–1309
Ferreiro Perez A, Garcia Isidro M, Ayerbe E, Castedo J, Jinkins JR. (2007) Evaluation of intervertebral disc herniation and hypermobile intersegmental instability in symptomatic adult patients undergoing recumbent and upright MRI of the cervical or lumbosacral spines. Eur J Radiol 62:444–448
Tarantino U, Fanucci E, Iundusi R et al (2013) Lumbar spine MRI in upright position for diagnosing acute and chronic low back pain: statistical analysis of morphological changes. J Orthop Traumatol 14:15–22
Zamani AA, Moriarty T, Hsu L et al (1998) Functional MRI of the lumbar spine in erect position in a superconducting open-configuration MR system: preliminary results. J Magn Reson Imaging 8:1329–1333
Splendiani A, Perri M, Grattacaso G et al (2016) Magnetic resonance imaging (MRI) of the lumbar spine with dedicated G-scan machine in the upright position: a retrospective study and our experience in 10 years with 4305 patients. Radiol Med 121:38–44
Hansen BB, Bouert R, Bliddal H et al (2013) External pneumatic compression device prevents fainting in standing weight-bearing MRI: a cohort study. Skeletal Radiol 42:1437–1442
Vandenbroucke JP, von Elm E, Altman DG et al (2014) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg 12:1500–1524
Freynhagen R, Baron R, Gockel U, Tölle TR (2006) painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 22:1911–1920
Fairbank JCT, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25:2940–2953
Espeland A, Vetti N, Kråkenes J (2013) Are two readers more reliable than one? A study of upper neck ligament scoring on magnetic resonance images. BMC Med Imaging 13:4
Pfirrmann CWA, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878
Pfirrmann CWA, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N (2004) MR image–based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology 230:583–588
Mauch F, Jung C, Huth J, Bauer G (2010) Changes in the lumbar spine of athletes from supine to the true-standing position in magnetic resonance imaging. Spine (Phila Pa 1976) 35:1002–1007
Hansen BB, Hansen P, Grindsted J et al (2017) Conventional supine MRI with a lumbar pillow—an alternative to weight-bearing MRI for diagnosing spinal stenosis? Spine (Phila Pa 1976) 42:662–669
Hansen BB, Bendix T, Grindsted J et al (2015) Effect of lumbar disc degeneration and low-back pain on the lumbar lordosis in supine and standing. Spine (Phila Pa 1976) 40:1690–1696
Boos N, Rieder R, Schade V, Spratt KF, Semmer NAM (1995) The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine (Phila Pa 1976):2613–2625
Adams MA, Lama P, Zehra U, Dolan P (2015) Why do some intervertebral discs degenerate, when others (in the same spine) do not? Clin Anat 28:195–204
Adams MA, Dolan P (2012) Intervertebral disc degeneration: evidence for two distinct phenotypes. J Anat 221:497–506
Zou J, Yang H, Miyazaki M et al (2009) Dynamic bulging of intervertebral discs in the degenerative lumbar spine. Spine (Phila Pa 1976) 34:2545–2550
Zou J, Yang H, Miyazaki M et al (2008) Missed lumbar disc herniations diagnosed with kinetic magnetic resonance imaging. Spine (Phila Pa 1976) 33:E140–E144
Jinkins JR, Dworkin JS, Damadian RV (2005) Upright, weight-bearing, dynamic–kinetic MRI of the spine: initial results. Eur Radiol 15:1815–1825
Schmid MR, Stucki G, Duewell S, Wildermuth S, Romanowski B, Hodler J (1999) Changes in cross-sectional measurements of the spinal canal and intervertebral foramina as a function of body position: in vivo studies on an open-configuration MR system. AJR Am J Roentgenol 172:1095–1102
Alyas F, Connell D, Saifuddin A (2008) Upright positional MRI of the lumbar spine. Clin Radiol 63:1035–1048
Hirasawa Y, Bashir WA, Smith FW, Magnusson ML, Pope MH, Takahashi K (2007) Postural changes of the dural sac in the lumbar spines of asymptomatic individuals using positional stand-up magnetic resonance imaging. Spine (Phila Pa 1976) 32:E136–E140
Weishaupt D, Schmid MR, Zanetti M et al (2000) Positional MR imaging of the lumbar spine: does it demonstrate nerve root compromise not visible at conventional MR imaging? Radiology 215:247–253
Brinjikji W, Luetmer PH, Comstock B et al (2015) Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol 36:811–816
Ramadorai U, Hire J, DeVine J, Brodt ED, Dettori JR (2014) Incidental findings on magnetic resonance imaging of the spine in the asymptomatic pediatric population: a systematic review. Evid Based Spine Care J 05:095–100
Stadnik TW, Lee RR, Coen HL, Neirynck EC, Buisseret TS, Osteaux MJ (1998) Annular tears and disk herniation: prevalence and contrast enhancement on MR images in the absence of low back pain or sciatica. Radiology 206:49–55
Weishaupt D, Zanetti M, Hodler J, Boos N (1998) MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology 209:661–666
Nordberg CL, Hansen BB, Nybing JD et al (2019) Weight-bearing MRI of the lumbar spine: technical aspects. Semin Musculoskelet Radiol 23:609–620
Lee RKL, Griffith JF, Lau YYO et al (2015) Diagnostic capability of low- versus high-field magnetic resonance imaging for lumbar degenerative disease. Spine (Phila Pa 1976) 40:382–391
Acknowledgments
The authors thank the staff at the Department of Radiology, Bispebjerg and Frederiksberg Hospital for their support running the study. The authors thank radiologists Jacob Grindsted, MD, and Zoreh Rasti, MD, Department of Radiology, Frederiksberg Hospital, Denmark, for inspiration, evaluation of the MR images, and discussions. The authors would also like to thank Sabrina Mai Nielsen for statistical support and methodological feedback.
Funding
This study was supported by unrestricted grants from The Oak Foundation (grant number: OCAY-13-309), the Danish Rheumatism Association, and Frederiksberg and Bispebjerg Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Bjarke Brandt Hansen, MD, PhD.
Conflict of interest
Mikael Boesen has been an invited speaker regarding the use of G-scanner for imaging of the lumbar spine for ESAOTE, Genoa, Italy, the manufacturer of the G-scanner, at ESSR 2012, 2014 and 2017, Modena Meeting Nov. 2013, Imola Meeting June 2017, and ECR 2014 as well as the 1st, 2nd, and 3rd International Weight-bearing Meeting (2016, 2018, and 2019). Philip Hansen has received a travel grant from ESAOTE for the 1st International Weight-bearing Meeting 2016. The other authors have no conflict of interests to declare.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Local Ethics Committee approval: KF 01–045/03.
Methodology
• prospective
• cross-sectional study
• single-center study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Nordberg, C.L., Boesen, M., Fournier, G.L. et al. Positional changes in lumbar disc herniation during standing or lumbar extension: a cross-sectional weight-bearing MRI study. Eur Radiol 31, 804–812 (2021). https://doi.org/10.1007/s00330-020-07132-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07132-w