Abstract
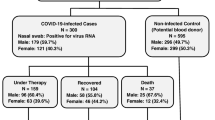
An association between coronavirus disease 2019 (COVID-19) and the ABO blood group has been reported. However, such an association has not been studied in the Japanese population on a large scale. Little is known about the association between COVID-19 and ABO genotype. This study investigated the association between COVID-19 and ABO blood group/genotype in a large Japanese population. All Japanese patients diagnosed with COVID-19 were recruited through the Japan COVID-19 Task Force between February 2020 and October 2021. We conducted a retrospective cohort study involving 1790 Japanese COVID-19 patients whose DNA was used for a genome-wide association study. We compared the ABO blood group/genotype in a healthy population (n = 611, control) and COVID-19 patients and then analyzed their associations and clinical outcomes. Blood group A was significantly more prevalent (41.6% vs. 36.8%; P = 0.038), and group O was significantly less prevalent (26.2% vs. 30.8%; P = 0.028) in the COVID-19 group than in the control group. Moreover, genotype OO was significantly less common in the COVID-19 group. Furthermore, blood group AB was identified as an independent risk factor for most severe diseases compared with blood group O [aOR (95% CI) = 1.84 (1.00–3.37)]. In ABO genotype analysis, only genotype AB was an independent risk factor for most severe diseases compared with genotype OO. Blood group O is protective, whereas group A is associated with the risk of infection. Moreover, blood group AB is associated with the risk of the “most” severe disease.



Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Branch DR (2010) Blood groups and susceptibility to virus infection: new developments. Curr Opin Hematol 17:558–564. https://doi.org/10.1097/MOH.0b013e32833ece31
Cooling L (2015) Blood groups in infection and host susceptibility. Clin Microbiol Rev 28:801–870. https://doi.org/10.1128/CMR.00109-14
Cheng Y, Cheng G, Chui CH et al (2005) ABO blood group and susceptibility to severe acute respiratory syndrome. JAMA 293:1450–1451. https://doi.org/10.1001/jama.293.12.1450-c
Zhao J, Yang Y, Huang H et al (2021) Relationship between the ABO blood group and the coronavirus disease 2019 (COVID-19) susceptibility. Clin Infect Dis 73:328–331. https://doi.org/10.1093/cid/ciaa1150
Zietz M, Zucker J, Tatonetti NP (2020) Associations between blood type and COVID-19 infection, intubation, and death. Nat Commun 11:5761. https://doi.org/10.1038/s41467-020-19623-x
Ray JG, Schull MJ, Vermeulen MJ, Park AL (2021) Association between ABO and Rh blood groups and SARS-CoV-2 infection or severe COVID-19 illness: a population-based cohort study. Ann Intern Med 174:308–315. https://doi.org/10.7326/M20-4511
Valenti L, Villa S, Baselli G et al (2020) Association of ABO blood group and secretor phenotype with severe COVID-19. Transfusion 60:3067–3070. https://doi.org/10.1111/trf.16130
Liu N, Zhang T, Ma L et al (2021) The impact of ABO blood group on COVID-19 infection risk and mortality: a systematic review and meta-analysis. Blood Rev 48:100785. https://doi.org/10.1016/j.blre.2020.100785
Amano J, Oshima M (1999) Expression of the H type 1 blood group antigen during enterocytic differentiation of Caco-2 cells. J Biol Chem 274:21209–21216. https://doi.org/10.1074/jbc.274.30.21209
Bucardo F, Nordgren J, Carlsson B et al (2010) Asymptomatic Norovirus infections in Nicaraguan children and its association with viral properties and histo-blood group antigens. Pediatr Infect Dis J 29:934–939. https://doi.org/10.1097/INF.0b013e3181ed9f2f
Nakao M, Matsuo K, Ito H et al (2011) ABO genotype and the risk of gastric cancer, atrophic gastritis, and Helicobacter pylori infection. Cancer Epidemiol Biomarkers Prev 20:1665–1672. https://doi.org/10.1158/1055-9965.EPI-11-0213
Schetelig J, Baldauf H, Wendler S et al (2021) Blood group A epitopes do not facilitate entry of SARS-CoV-2. J Intern Med 290:223–226. https://doi.org/10.1111/joim.13256
Namkoong H, Edahiro R, Fukunaga K et al (2021) Japan COVID-19 Task Force: a nationwide consortium to elucidate host genetics of COVID-19 pandemic in Japan. Medrxiv. https://doi.org/10.1101/2021.05.17.21256513
Tanaka H, Lee H, Morita A et al (2021) Clinical characteristics of patients with coronavirus disease (COVID-19): preliminary baseline report of Japan COVID-19 Task Force, a nationwide consortium to investigate host genetics of COVID-19. Int J Infect Dis 113:74–81. https://doi.org/10.1016/j.ijid.2021.09.070
Novel coronavirus: COVID-19 therapeutic trial synopsis. https://www.who.int/publications/i/item/covid-19-therapeutic-trial-synopsis. Accessed 26 Jun 2022
Yip SP (2002) Sequence variation at the human ABO locus. Ann Hum Genet 66:1–27. https://doi.org/10.1017/S0003480001008995
Cserti CM, Dzik WH (2007) The ABO blood group system and Plasmodium falciparum malaria. Blood 110:2250–2258. https://doi.org/10.1182/blood-2007-03-077602
Lane WJ, Westhoff CM, Gleadall NS et al (2018) Automated typing of red blood cell and platelet antigens: a whole-genome sequencing study. Lancet Haematol 5:e241–e251. https://doi.org/10.1016/S2352-3026(18)30053-X
Docherty AB, Harrison EM, Green CA et al (2020) Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO clinical characterisation protocol. Medrxiv. https://doi.org/10.1101/2020.04.23.20076042
Deng G, Yin M, Chen X, Zeng F (2020) Clinical determinants for fatality of 44,672 patients with COVID-19. Crit Care 24:179. https://doi.org/10.1186/s13054-020-02902-w
Cunningham JW, Vaduganathan M, Claggett BL et al (2020) Clinical outcomes in young US adults hospitalized with COVID-19. JAMA Intern Med 181:379–381. https://doi.org/10.1001/jamainternmed.2020.5313
Harrison SL, Fazio-Eynullayeva E, Lane DA, Underhill P, Lip GYH (2020) Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: a federated electronic medical record analysis. PLOS Med 17:e1003321. https://doi.org/10.1371/journal.pmed.1003321
Zeberg H, Pääbo S (2020) The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature 587:610–612. https://doi.org/10.1038/s41586-020-2818-3
Price-Haywood EG, Burton J, Fort D, Seoane L (2020) Hospitalization and mortality among black patients and white patients with COVID-19. N Engl J Med 382:2534–2543. https://doi.org/10.1056/NEJMsa2011686
Fujita Y, Tanimura M, Tanaka K (1978) The distribution of the ABO blood groups in Japan. J Hum Genet 23:63–109. https://doi.org/10.1007/BF02001790
Li J, Wang X, Chen J, Cai Y, Deng A, Yang M (2020) Association between ABO blood groups and risk of SARS-CoV-2 pneumonia. Br J Haematol 190:24–27. https://doi.org/10.1111/bjh.16797
Wu BB, Gu DZ, Yu JN, Yang J, Shen WQ (2020) Association between ABO blood groups and COVID-19 infection, severity and demise: a systematic review and meta-analysis. Infect Genet Evol 84:104485. https://doi.org/10.1016/j.meegid.2020.104485
Halim MR, Saha S, Haque IU et al (2021) ABO blood group and outcomes in patients with COVID-19 admitted in the intensive care unit (ICU): a retrospective study in a tertiary-level hospital in Bangladesh. J Multidiscip Healthc 14:2429–2436. https://doi.org/10.2147/JMDH.S330958
Muñiz-Diaz E, Llopis J, Parra R et al (2021) Relationship between the ABO blood group and COVID-19 susceptibility, severity and mortality in two cohorts of patients. Blood Transfus 19:54–63. https://doi.org/10.2450/2020.0256-20
Severe Covid-19 GWAS Group: Ellinghaus D, Degenhardt F et al (2020) Genome-wide association study of severe COVID-19 with respiratory failure. N Engl J Med 383:1522–1534. https://doi.org/10.1056/nejmoa2020283
Al-Youha SA, Alduaij W, Al-Serri A et al (2021) The impact of ABO blood groups on clinical outcomes and susceptibility to COVID-19: a retrospective study in an unselected population. Transfusion 61:1631–1641. https://doi.org/10.1111/trf.16365
Domènech-Montoliu S, Puig-Barberà J, Pac-Sa MR et al (2021) ABO blood groups and the incidence of complications in COVID-19 patients: a population-based prospective cohort study. Int J Environ Res Public Health 18:10039. https://doi.org/10.3390/ijerph181910039
Latz CA, DeCarlo C, Boitano L et al (2020) Blood type and outcomes in patients with COVID-19. Ann Hematol 99:2113–2118. https://doi.org/10.1007/s00277-020-04169-1
Dai X (2020) ABO blood group predisposes to COVID-19 severity and cardiovascular diseases. Eur J Prev Cardiol 27:1436–1437. https://doi.org/10.1177/2047487320922370
Gérard C, Maggipinto G, Minon JM (2020) COVID-19 and ABO blood group: another viewpoint. Br J Haematol 190:e93–e94. https://doi.org/10.1111/bjh.16884
Garratty G (2000) Blood groups and disease: a historical perspective. Transfus Med Rev 14:291–301. https://doi.org/10.1053/tmrv.2000.16228
Zakai NA, Judd SE, Alexander K et al (2014) ABO blood type and stroke risk: the REasons for Geographic and Racial Differences in Stroke Study. J Thromb Haemost 12:564–570. https://doi.org/10.1111/jth.12507
Jukic I, Bingulac-Popovic J, Dogic V et al (2009) ABO blood groups and genetic risk factors for thrombosis in Croatian population. Croat Med J 50:550–558. https://doi.org/10.3325/cmj.2009.50.550
Nakao M, Matsuo K, Hosono S et al (2011) ABO blood group alleles and the risk of pancreatic cancer in a Japanese population. Cancer Sci 102:1076–1080. https://doi.org/10.1111/j.1349-7006.2011.01907.x
Shibeeb S, Khan A (2022) ABO blood group association and COVID-19. COVID-19 susceptibility and severity: a review. Hematol Transfus Cell Ther 44:70–75. https://doi.org/10.1016/j.htct.2021.07.006
Acknowledgements
We would like to thank all the participants involved in this study and all members of the Japan COVID-19 Task Force engaged in clinical and research work on COVID-19 daily. All the members contributed to this study.
Funding
This work was supported by the Japan Agency for Medical Research and Development (grant numbers JP20nk0101612, JP20fk0108415, JP21km0405211, JP21km0405217, and JP21wm0325031), the Core Research for Evolutionary Science and Technology (grant number JPMJCR20H2), the Precursory Research for Embryonic Science and Technology (grant number JPMJPR21R7), and the Ministry of Health, Labor and Welfare (grant number 20CA2054).
Author information
Authors and Affiliations
Contributions
Conceptualization: T.K., S.C., H.N., T.A., K.M., H.K., M.I., N.H., and K.F. Data curation: T.K., H.T., H.L., S.O., K.N., T.F., A.M., and M.W. Formal analysis: T.K., S.C., and H.N. Methodology: T.K., S.C., and H.N. Supervision: T.K., S.C., N.H., T.A., K.M., H.K, M.I., N.H., N.H., T.U., S.U., T.I., K.A., F.S., T.Y., Y.N., Y.M., Y.S., R.E., K.M., Y.S., Y.O., R.K., Y.K., K.T., A.K., S.I., S.M., S.O., T.K., and K.F. Visualization: T.K., S.C., and H.N. Writing—original draft: T.K., S.C., and H.N. Writing—review and editing: T.K., S.C., N.H., T.A., K.M., H.K, M.I., N.H., N.H., T.U., S.U., T.I., K.A., F.S., T.Y., Y.N., Y.M., Y.S., R.E., K.M., Y.S., Y.O., R.K., Y.K., K.T., A.K., S.I., S.M., S.O., T.K., and K.F. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All patients involved in this study provided written or oral consent, and the study design was approved by the ethics committees of Keio University School of Medicine (20200061) and the affiliated research institutions.
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 56 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kusumoto, T., Chubachi, S., Namkoong, H. et al. Association between ABO blood group/genotype and COVID-19 in a Japanese population. Ann Hematol 102, 3239–3249 (2023). https://doi.org/10.1007/s00277-023-05407-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05407-y