Abstract
Background
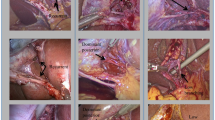
Primary aspect of hepatic navigation surgery is the identification of source vascular details to preserve healthy liver which has a vascular anatomy quite challenging for the young surgeons. The purpose was to determine whether three-dimensional (3D) vascular pattern models of preoperative computed tomography (CT) images will assist resident-level trainees for hepatic surgery.
Methods
This study was based on the perception of residents who were presented with 5 different hepatic source vascular patterns and required to compare their perception level of CT, and 1:1 models in terms of importance of variability, differential of patterns and preoperative planning.
Results
All residents agree that models provided better understanding of vascular source and improved preplanning. Five stations provided qualitative assessment with results showing the usefulness of porta-celiac models when used as anatomical tools in preplanning (p = 0.04), simulation of interventional procedures (p = 0.02), surgical education (p = 0.01). None of the cases had scored less than 8.5. Responses related to understanding variations were significantly higher in the perception of the 3D model in all cases, furthermore 3D models were more useful for seniors in more complex cases 3 and 5. Some open-ended answers: “The 3D model can completely change the operation plan” One of the major factors for anatomical resection of liver transplantation is the positional relationship between the hepatic arteries and the portal veins.
Conclusion
The plastic-like material presenting the hepatic vascularity enables the visualization of the origin, pattern, shape, and angle of the branches with appropriate spatial perception thus making it well-structured.













Similar content being viewed by others
References
Aloia TA, Vauthey JN (2012) Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): What is gained and what is lost? Ann Surg 256:e9-19
Andolfi C, Plana A, Kania P, Banerjee PP, Small S (2017) Usefulness of three-dimensional modeling in surgical planning, resident training, and patient education. J Laparoendosc Adv Surg Tech A 27:512–515
Atasoy C, Ozyurek E (2006) Prevalence and types of main and right portal vein branching variations on MDCT. AJR Am J Roentgenol 187:676–681
Baimakhanov Z, Soyama A, Takatsuki M, Hidaka M, Hirayama T, Kinoshita A, Natsuda K, Kuroki T, Eguchi S (2015) Preoperative simulation with a 3-dimensional printed solid model for one-step reconstruction of multiple hepatic veins during living donor liver transplantation. Liver Transpl 21:266–268
Balci D, Ahn CS (2019) Hepatic artery reconstruction in living donor liver transplantation. Curr Opin Organ Transplant 24:631–636
Bati AH, Guler E, Ozer MA, Govsa F, Erozkan K, Vatansever S, Ersin MS, Elmas ZN, Harman M (2020) Surgical planning with patient-specific three-dimensional printed pancreaticobiliary disease models—cross-sectional study. Int J Surg 80:175–183
Bressan AK, Edwards JP, Grondin SC, Dixon E, Minter RM, Jeyarajah DR, Ball CG (2015) The adequacy of Hepato-Pancreato-Biliary training: how closely do perceptions of fellows and programme directors align? HPB (Oxford) 17:791–795
Covey AM, Brody LA, Getrajdman GI, Sofocleous TC, Brown KT (2004) Incidence, patterns, and clinical relevance of variant portal vein anatomy. AJR Am J Roentgenol 183:1055–1064
Cromeens BP, Ray WC, Hoehne B, Abayneh F, Adler B, Besner GE (2017) Facilitating surgeon understanding of complex anatomy using a three-dimensional printed model. J Surg Res 216:18–25
Crossingham JL, Jenkinson J, Woolridge N, Gallinger S, Tait GA, Moulton CE (2009) Interpreting three-dimensional structures from two-dimensional images: a web-based interactive 3D teaching model of surgical liver anatomy. HPB (Oxford) 11:523–528
De Cecchis L, Hribernik M, Ravnik D, Gadzijev EM (2000) Anatomical variations in the pattern of the right hepatic veins: possibilities for type classification. J Anat 197(Pt 3):487–493
Donato P, Coelho P, Rodrigues H, Vigia E, Fernandes J, Caseiro-Alves F, Bernardes A (2007) Normal vascular and biliary hepatic anatomy: 3D demonstration by multidetector CT. Surg Radiol Anat 29:575–582
Erbay N, Raptopoulos V, Pomfret EA, Kamel IR, Kruskal JB (2003) Living donor liver transplantation in adults: vascular variants important in surgical planning for donors and recipients. AJR Am J Roentgenol 181:109–114
Fasel JH, Aguiar D, Kiss-Bodolay D, Montet X, Kalangos A, Stimec BV, Ratib O (2016) Adapting anatomy teaching to surgical trends: a combination of classical dissection, medical imaging, and 3D-printing technologies. Surg Radiol Anat 38:361–367
Hiatt JR, Gabbay J, Busuttil RW (1994) Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg 220:50–52
Ikegami T, Maehara Y (2013) Transplantation: 3D printing of the liver in living donor liver transplantation. Nat Rev Gastroenterol Hepatol 10:697–698
Javan R, Zeman M (2018) A prototype educational model for hepatobiliary interventions: unveiling the role of graphic designers in medical 3D printing. J Digit Imaging 31:133–143
Kim TS, Noh YN, Lee S, Song SH, Shin M, Kim JM, Kwon CH, Kim SJ, Lee SK, Joh JW (2012) Anatomic similarity of the hepatic artery and portal vein according to the donor-recipient relationship. Transplant Proc 44:463–465
Langridge B, Momin S, Coumbe B, Woin E, Griffin M, Butler P (2018) Systematic review of the use of 3 dimensional printing in surgical teaching assessment. J Surg Educ 75:209–221
Lee KK, Lee SK, Moon IS, Kim DG, Lee MD (2008) Surgical techniques according to anatomic variations in living donor liver transplantation using the right lobe. Transplant Proc 40:2517–2520
Madoff DC, Hicks ME, Vauthey JN, Charnsangavej C, Morello FA Jr, Ahrar K, Wallace MJ, Gupta S (2002) Transhepatic portal vein embolization: anatomy, indications, and technical considerations. Radiographics 5:1063–1076
Malik HH, Darwood ARJ, Shaunak S, Kulatilake P, El-Hilly AA, Mulki O, Baskaradas A (2015) Three-dimensional printing in surgery: a review of current surgical applications. J Surg Res 199:512–522
Marro A, Bandukwala T, Mak W (2016) Three-dimensional printing and medical imaging: a review of the methods and applications. Curr Probl Diagn Radiol 45:2–9
Martelli N, Serrano C, van den Brink H, Pineau J, Prognon P, Borget I, El Batti S (2016) Advantages and disadvantages of 3-dimensional printing in surgery: a systematic review. Surgery 159:1485–1500
Mattar SG, Alseidi AA, Jones DB, Jeyarajah DR, Swanstrom LL, Aye RW, Wexner SD, Martinez JM, Ross SB, Awad MM, Franklin ME, Arregui ME, Schirmer BD, Minter RM (2013) General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg 258:440–449
Mochizuki K, Takatsuki M, Soyama A, Hidaka M, Obatake M, Eguchi S (2012) The usefulness of a high-speed 3D-image analysis system in pediatric living donor liver transplantation. Ann Transplant 17:31–34
Nemeth K, Deshpande R, Mathe Z, Szuák A, Kiss M, Korom C, Nemeskéri Á, Kóbori L (2015) Extrahepatic arteries of the human liver-anatomical variants and surgical relevancies. Transpl Int 28:1216–1226
Ohshima S (2014) Volume analyzer synapse vincent for liver analysis. J Hepatobiliary Pancreat Sci 21:235–238
Olthoff KM, Abecassis MM, Emond JC, Kam I, Merion RM, Gillespie BW, Tong L (2011) Outcomes of adult living donor liver transplantation: comparison of the adult-to-adult living donor liver transplantation cohort study and the national experience. Liver Transplant 17:789–797
Ozturk AM, Ozer MA, Suer O, Derin O, Govsa F, Aktuglu K (2020) Evaluation of the effects of using 3D - patient specific models of displaced intra - articular calcaneal fractures in surgery. Injury 13:S0020-1383(20)30402–2
Perica ER, Sun Z (2018) A systematic review of three-dimensional printing in liver disease. J Digit Imaging 31:692–701
Radtke A, Sotiropoulos GC, Sgourakis G, Molmenti EP, Schroeder T, Saner FH, Beckebaum S, Broelsch CE, Broering DC, Malago M (2010) Hepatic venous drainage: how much can we learn from imaging studies? Anatomic-functional classification derived from three-dimensional computed tomography reconstructions. Transplantation 89:1518–1525
Satou S, Sugawara Y, Tamura S, Kishi Y, Kaneko J, Matsui Y, Kokudo N, Makuuchi M (2007) Three-dimensional computed tomography for planning donor hepatectomy. Transplant Proc 39:145–149
Seshadri RM, Ali N, Warner S (2015) Training and practice of the next generation HPB surgeon: analysis of the 2014 AHPBA residents’ and fellows’ symposium survey. HPB (Oxford) 17:1096–1104
Uchida K, Taniguchi M, Shimamura T, Suzuki T, Yamashita K, Ota M, Kamiyama T, Matsushita M, Furukawa H, Todo S (2010) Three-dimensional computed tomography scan analysis of hepatic vasculatures in the donor liver for living donor liver transplantation. Liver Transpl 16:1062–1068
Tani K, Shindoh J, Akamatsu N, Arita J, Kaneko J, Sakamoto Y, Hasegawa K, Kokudo N (2016) Venous drainage map of the liver for complex hepatobiliary surgery and liver transplantation. HPB (Oxford) 18:1031–1038
Yeo CT, MacDonald A, Ungi T, Lasso A, Jalink D, Zevin B, Fichtinger G, Nanji S (2018) Utility of 3D reconstruction of 2D liver computed tomography/magnetic resonance images as a surgical planning tool for residents in liver resection surgery. J Surg Educ 75:792–797
Funding
This study has no funding.
Author information
Authors and Affiliations
Contributions
AC, AU: project idea, project development. OVU: data collection, data analysis. AC: data analysis, surgery simulation. AHB: data analysis. EG: data collection, data analysis. MAO: 3D printing, 3D patient-specific models. FG: manuscript writing, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare to conflict of interest in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozer, M.A., Uguz, A., Unalp, O.V. et al. Perceptions of porta-celiac vascular models for hepatic surgery and their use in residency training. Surg Radiol Anat 43, 1359–1371 (2021). https://doi.org/10.1007/s00276-021-02724-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-021-02724-7