Abstract
This CIRSE Standards of Practice document is aimed at interventional radiologists and provides best practices for performing liver regeneration therapies prior to major hepatectomies, including portal vein embolization, double vein embolization and liver venous deprivation. It has been developed by an expert writing group under the guidance of the CIRSE Standards of Practice Committee. It encompasses all clinical and technical details required to perform liver regeneration therapies, revising the indications, contra-indications, outcome measures assessed, technique and expected outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The CIRSE Standards of Practice (SOP) Committee established a writing group which was tasked with producing up-to-date recommendations for performing portal vein embolization (PVE), with or without hepatic vein embolization (HVE). CIRSE SOP documents are not clinical practice guidelines or systematic reviews of the literature. CIRSE SOP documents are not intended to impose a standard of clinical patient care but recommend a reasonable approach to and best practices for performing PVE, with or without HVE. Institutions should regularly review their internal procedures for development and improvement, taking into account international guidance, local resources and regular internal morbidity and mortality reviews.
Methods
The writing group, which was established by the CIRSE SOP Committee, consisted of 5 clinicians with internationally recognised expertise in PVE. The current document updates the 2010 CIRSE SOP on PVE [1]. A summary of definitions and key recommendations on PVE, sequential PVE followed by HVE, double vein embolization (DVE or bi-embolization or PVE/HVE) and liver venous deprivation (LVD) can be found in Table 1. The writing group reviewed existing literature on PVE/HVE/DVE/LVD, performing a pragmatic evidence search using PubMed to select relevant publications in the English language and involving human subjects, preferably published from 2010 (last SOP document) to date. The final recommendations were formulated through consensus.
Background
Rationale: Post-Hepatectomy Liver Failure
Liver resection is considered the standard of care curative option in patients with secondary or primary liver tumours. Liver surgery for liver tumours is split between liver-sparing surgery, where tumours are resected with oncological margins (tumourectomy), and anatomical resection where the segment or lobe bearing the tumour is resected entirely. Anatomical liver resection is considered a major resection when more than three segments are resected in one surgery [2]. Despite refinements in surgical techniques and improvement in patient preparation and critical care, major hepatectomy still carries a significant risk of morbidity and mortality mainly due to post-hepatectomy liver failure (PHLF).
Reported incidence of PHLF varies widely between 1.2% and 32% due to variations in patient population and procedures, but also due to the lack of a universally accepted definition of PHLF [3]. The International Study Group of Liver Surgery (ISGLS) redefined PHLF based on bilirubin and international normalized ratio (INR) values measured at day 5 or thereafter and proposed a severity grading system [3]. Risk factors for PHLF are related to the volume of future liver remnant (FLR) [4], and also to the underlying liver status such as post-chemotherapy liver injury [5, 6] or chronic liver disease such as cirrhosis [7] or chronic cholestasis [8]. Recently, in complement to the FLR volume, FLR function appeared as an important factor associated with PHLF [9, 10]. To identify patients with insufficient liver function in the FLR, new nuclear medicine investigations have been developed such as mebrofenin scintigraphy [8, 9] allowing quantification of liver function.
Strategies to Increase the Volume of the Future Liver Remnant
Strategies to increase the FLR volume preoperatively have been developed over the years, allowing more patients to undergo successful surgical resection. The first is PVE, which consists of embolizing the portal branches of the future resected liver (i.e. usually right liver portal branches) 3–5 weeks before hepatectomy [11]. This method has a very low morbidity and is well tolerated [12] and carries a high success rate. However, in 15–20% of patients after PVE, the planned hepatectomy cannot be performed either due to tumour progression or due to insufficient hypertrophy [13]. There is a surgical equivalent technique which is portal vein ligation that can sometimes be used, especially when tumourectomies are to be performed on the FLR. With this surgery, one of the portal vein branches is ligated and can also be embolized with ethanol. Another option is to perform ablation of the FLR tumours and PVE at the same time. To reduce the risk of tumour progression, by decreasing the delay between liver preparation and resection, an aggressive surgical approach has been developed associating right portal vein ligation and liver partition—so called ALPPS (associating liver partition and portal vein ligation for staged hepatectomy) one week before hepatectomy [14]. Despite initial enthusiasm due to very rapid FLR hypertrophy, concerns were raised due to the high morbidity and mortality rates seen with this surgical strategy [15]. One possible explanation for these disappointing results is the fact that despite a rapid volumetric gain, the function of the FLR does not necessarily mirror the volumetric gain and may even decrease [16]. Preoperative FLR functional evaluation has been advised after studies assessing ALPPS series revealing that volumetric gain might not be followed by functional gain [16]. After ALPPS first-stage, liver functional gain was only half of the volumetric gain, explaining the high rate of morbidity and mortality following this regenerative surgical approach [16]. One other strategy has been explored in patients with insufficient liver volume gain four weeks after PVE, by adding HVE. This strategy, called sequential PVE followed by HVE, has shown to add further liver regeneration [17]. A major drawback of this approach is the delay between each procedure increasing the risk of liver or extrahepatic tumour progression. A delay of four weeks is necessary to assess liver volumetric gain after PVE followed by another four weeks after additional HVE [17,18,19]. In this context, the concept of combining PVE and HVE in the same procedure appeared recently under different descriptions in the literature such as LVD and DVE (i.e. bi-embolization) [20, 21]. The theoretical benefit is to accelerate and induce more hypertrophy than PVE alone and to reduce the risk of absent or insufficient hypertrophy. After PVE, portal vein collaterals between the FLR and the embolized liver develop and compromise FLR hypertrophy. Embolizing ipsilateral hepatic and portal vein branches with ALPPS or LVD/DVE will block the development of these portal vein collaterals between the FLR and the embolized liver. This will optimize flow and minimize hepatotrophic factor washout from the FLR, enhancing hypertrophy [14,15,16,17,18,19,20,21].
Indications and Contra-Indications for Liver Regeneration Techniques Prior to Major Hepatectomies
Indications for these liver regeneration techniques are based on liver volume assessment by computed tomography (CT). All surgical groups agree that a FLR/TLV (total liver volume) ratio below 20% is an indication for a liver regeneration technique such as PVE, DVE, LVD or ALPPS. Debates about the use of either the functional liver volume measured by CT or the estimated total liver volume based on body surface area are still unresolved [22, 23]. Both methods can be used, but they carry some discrepancies in 5% of patients [24], potentially leading to decision errors regarding PVE indication. Of course, estimating the liver volume by CT does not estimate the function and regenerative capacity of FLR after resection. Many groups also consider the liver function estimated either by mebrofenin scintigraphy-CT or by MRI using hepato-specific contrast agent. These two imaging techniques can estimate hepatocyte function by quantitative imaging [8, 25, 26]. PVE/DVE/LVD can be proposed in patients bearing colorectal (or other less frequent) liver metastases, but also before major hepatectomy for hepatocellular carcinoma, or intrahepatic cholangiocarcinoma or hilar type (Klatskin) cholangiocarcinoma [27, 28]. The threshold of FLR/TLV ratio for PVE or DVE/LVD is different among these different groups and varies between 20% (colorectal metastases), 30% (colorectal metastases with post-chemotherapy liver injury) and 40% (hepatocellular carcinoma with underlying liver cirrhosis and Klatskin tumours) [27]. The suggested thresholds for resections are shown in Table 2. There are no absolute contra-indications for PVE or DVE/LVD if the patient is considered eligible for major hepatectomy. For patients with Klatskin tumours and obstructive jaundice, most centres recommend biliary drainage before liver regeneration treatments and bilirubin levels < 5–10 μmol/L, even though simultaneous biliary drainage and PVE has been shown to be safe and effective [28].
Patient Preparation
The decision for liver regeneration therapies should be made in multidisciplinary team meetings (MDT) of surgeons, hepatologists, oncologists, and interventional radiologists with respect to the individual patient’s performance status, tumour resectability and vascular invasion, FLR volume and function, type of tumour and underlying liver disease. Informed consent should be obtained 24 h ahead of treatment. In addition to routine laboratory parameters, particularly for coagulation and bilirubin, pre-surgical work-up (within the month preceding intervention) should include CT/MRI-based liver volume analysis (FLR/TLV/FLR ratio) and ideally should also include functional liver assessment. If additional ablations are planned within the FLR, the corresponding volumes must be considered in the calculation.
As biliary obstruction can impair liver regeneration and hypertrophy, the biliary tree of the FLR should be drained before PVE/DVE/LVD when bilirubin levels > 2 μmol/L (threshold for a safe major hepatectomy) [28]. For patients with hepatocellular carcinoma with underlying liver cirrhosis, transarterial chemoembolization may be performed 3–4 weeks before PVE/DVE/LVD, enhancing the regeneration of the FLR [29, 30]. The CIRSE SOP on Peri-operative Anticoagulation Management During Interventional Radiology Procedures should be followed for PVE/DVE/LVD [31]. There are guidelines for prophylactic antibiotic therapy in interventional radiology in general but not for PVE/DVE/LVD in particular; therefore, decisions should be made on a case-by-case basis considering individual risk factors (prior biliary manipulation or infection), the patient’s history and the therapeutic strategy including combinations of vascular/non-vascular interventions [32].
Portal Vein Embolization Technique
After skin disinfection and local anaesthesia, PVE is usually performed via ultrasound-guided percutaneous transhepatic portal vein access using a 21–22G needle and 0.018-inch guide wire included in dedicated tri-axial micropuncture kits (with a metallic stiffening cannula, a dilator, and a 10–20 cm long 4–6 Fr. sheath) [1, 11, 12]. Alternative routes include transileocolic and transsplenic approaches. The transileocolic technique necessitates a mini-laparotomy and can also be part of a two-stage surgical resection. The transhepatic route allows for the procedure to be conducted via either ipsilateral or contralateral puncture. The advantages of ipsilateral (i.e. right access for right PVE) access are: no damage to the FLR, ability to gain access to segment IV portal venous branches and reduced risk of radiation exposure to the operator’s hand. Its drawbacks include the need for reversed catheters that are used for PVE and for the completion portography, with longer and more complex procedures. The contralateral approach may induce damage to the FLR and poses more radiation exposure to the operator, but it provides more direct access to the target portal vein branches [1, 11, 12]. Catheters used are usually 4–5 Fr. reversed catheters for ipsilateral approach and 4–5 Fr. angled-tip catheters for contralateral approach. When the embolic agent used is n-butyl cyanoacrylate (NBCA), it is recommended to perform the embolization with 2.4–3.0 Fr. microcatheters. NBCA can adhere to the interior of catheters and migrate to untargeted portal vein branches. Thus, using super selective catheterization with microcatheters reduces the risk of untargeted embolization to portal vein branches of the FLR.
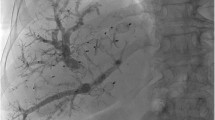
After gaining access to the portal system, 2D (20 ml of contrast medium; 10 ml/s contrast injection; right anterior oblique view of 25°) or 3D portography (35 ml of 1:1 or 3:2 iodine contrast to saline mixture; 5 ml/s contrast injection; with 2 s X-ray delay and 5 s acquisition/rotation time; volume of contrast adjusted to acquisition/rotation time) is recommended to assess the portal anatomy. With ipsilateral approaches, the portography should be performed with reversed catheters and selective embolization of portal vein branches can be performed via the same catheter when particles and coils are used. However, microcatheters should be used for embolization with NBCA. The same reversed catheter can be used for the completion portography. With contralateral approaches the same angled-tip catheter can be used for portography and embolization but a different catheter should be used for completion portography, when NBCA is used. Embolization of segment IV portal venous branches, although technically challenging, is safe in experienced hands and can improve hypertrophy and extend resectability [33] at the expense of a technically challenging procedure (4–6 branches usually supply segment IV). Cone-beam CT or angio-CT technologies with 3D road-mapping and microcatheters are therefore recommended.
Embolic materials used for PVE [34] include absolute ethanol [35,36,37], polyvinyl alcohol (PVA), gelatin sponge, fibrin glue, NBCA mixed with lipiodol [38], polidocanol-foam, or hybrid combinations of these agents with coils [39] or vascular plugs [40, 41]. Several studies showed a benefit of NBCA over PVA [42] and microparticles + coils [43,44,45] in terms of FLR hypertrophy, with similar complication rates. For particles, 200–1000 µm particles (spherical or non-spherical) are recommended followed by 8 mm–16 mm diameter coils placed in the portal vein branch being embolized, through 4–5 Fr. catheters. Plugs used are usually 8–18 mm in diameter (10–20% oversizing) and will require larger (6–8 Fr.) sheaths for deployment. NBCA/lipiodol dilutions of 1/4–1/8 are recommended and care must be taken to flush all catheters with dextrose 5% and to avoid saline. Continuous injection of glue or a sandwich technique (injection of small amounts of NBCA interspaced with dextrose flushing) are based on operator preference.
Double Vein Embolization and Liver Venous Deprivation Technique
The LVD technique was originally outlined as a fully transhepatic procedure [20]. Hepatic veins (HVs)—right, optional accessory right, and possibly middle (extended LVD)—are initially accessed with ultrasound guidance using a 21–22 G Chiba needle and a 0.018-inch wire, along with a micropuncture set. PVE is performed after wire/sheath access to the HVs. A 6–10 Fr. sheath is placed in each HV to deploy a vascular plug, positioning its distal end about 15 mm proximal to its junction with the vena cava. The plug positioning is crucial, so that surgical HV ligation with a stapler is not compromised during the planned hepatectomy. The vascular plug should be oversized by around 40% to prevent migration, and its accurate placement can be confirmed with ultrasound. Veno-venous collaterals quickly develop after proximal occlusion by the vascular plug, which is the reason why glue at a lower dilution (1/3–1/5) has been proposed to occlude not only distal venous branches but also these collaterals. These collaterals pose a challenge as they may lead to untargeted NBCA embolization to the lungs. This is one of the reasons why some centres prefer DVE over LVD. All transhepatic accesses can be embolized with glue, gelfoam or coils. The same LVD technique can be performed via a transjugular or transfemoral approach, with a micro-catheter in parallel to the vascular plug, to inject glue. The critical step is to prepare the glue and iodized oil mixture prior to plug deployment and to start injecting the mixture immediately behind the plug due to the quick expansion of these collaterals when outflow is blocked. Since, the middle HV drains approximately 2/3 of the right paramedian sector, the tolerance of LVD led to a proposal to extend LVD (extended LVD) embolizing not only the right (and accessory right HV when present) but also the middle HV using the exact same technique [46].
The notion of DVE or bi-embolization has been introduced but is specific to deploying only vascular plugs ± coils in the HVs via transjugular or transhepatic access [21]. This method may leave distal collaterals open, which can bypass the vascular plug within minutes. Thus, multiple vascular plugs ± coils should be used to occlude the whole HV. LVD embolizes both proximal (via vascular plug) and distal venous branches (via NBCA), as well as potential collaterals. The use of multiple vascular plugs placed all along the HVs and their tributaries can be considered instead of vascular plug + glue [47]. No data are currently available on the most optimal technique. PVE should be performed prior to DVE or LVD to allow better glue penetration into portal vein branches and reduce the risk of contralateral non-target glue reflux [48].
Peri-Procedural and Follow-Up Care
PVE/DVE/LVD can be performed in an outpatient setting; however, a short (1-day) inpatient stay is usually preferred. According to the CIRSE SOP on Analgesia and Sedation for Interventional Radiology in Adults, accurate evaluation, monitoring and documentation of patient care is important to minimise the risk of adverse events [49]. Procedural medication and monitoring of the patient should be delivered by a team member other than the specialist performing the procedure [49]. PVE/DVE/LVD can be performed using only pain medication without sedation in most cases. Nevertheless, sedation or general anaesthesia is also possible and might be required when NBCA is used as it induces more inflammation and pain when compared to PVA and coils. Whenever deeper levels of sedation are required, anaesthetists should be involved [49]. Follow-up imaging to assess hypertrophy of the FLR should ideally be performed using the same modality as before the procedure and timed to coincide with the planned surgery, ideally 14–28 days after the intervention. The time from PVE/DVE/LVD to planned hepatectomy varies between teams and clinical scenarios ranging from 2–4 weeks in non-cirrhotics to 2–3 months in cirrhotics [11,12,13,14,15,16,17,18,19,20,21]. Asthenia may develop after LVD, thus routine multivitamin and phosphorus supplementation may be considered, which may also enhance FLR hypertrophy [20, 21, 46, 47].
Outcomes
Technical/Clinical Outcomes and Complications
Technical and clinical success after PVE (complete occlusion of all planned portal branches and enough FLR regeneration for the intended hepatectomy, respectively) is very high, and should be expected to be above 98% and 90%, respectively [34, 38]. Common reasons for technical failure are inability to access the portal system (blocked needle pathway due to liver tumour burden or altered portal anatomy caused by the tumour mass or unexpected thrombosis of the portal system) or incomplete embolization of the portal vein branches (missed portal vein branch during PVE) [44, 50]. Lack of the expected FLR regeneration after a technically successful performed PVE, measured by the degree of hypertrophy (DH) and kinetic growth rate (KGR), has been associated with a significantly higher incidence of PHLF [51, 52], and should be interpreted as an alert sign of a poor background liver function and reserve.
One of the most feared complications after PVE is that it may preclude the awaited liver surgery. A systematic review revealed that in 0.4% of cases, patients will not proceed to the planned hepatectomy due to major complications (severe cholangitis, large abscesses and sepsis, and portal venous or mesentericoportal venous thrombosis) [34]. As with other hepatic percutaneous procedures, complications after PVE may arise due to the transhepatic access, such as subcapsular haematoma, haemoperitoneum, pneumothorax, haemobilia, arteriovenous shunts, pseudoaneurysm, cholangitis and sepsis. Other complications such as post-embolization syndrome, non-target embolization, portal vein thrombosis and transient liver failure may also occur. The complication threshold for PVE should be expected to be 2.5% [53]. Mortality after PVE is rare and has been scarcely reported. In a meta-analysis consisting of 1088 patients, the overall morbidity rate for PVE was 2.2% without mortality [53]. In a single-institution large cohort of 146 patients, the thirty-day mortality was 0.7% [38]. Mortality rate after PVE should be expected to be maximum of 0.1% [34].
It has been suggested that PVE might lead to tumour progression and worse oncological outcomes in patients submitted to liver surgery [54, 55]. The arterial buffer phenomenon (increase of liver arterial perfusion after portal vein occlusion) [56] and the release of hypertrophic factors involved in the regeneration process may stimulate tumour growth. Nevertheless, larger studies, including a systematic review with meta-analysis, showed no adverse effect in the local liver tumour progression, nor in the overall survival of patients treated with liver surgery, with versus without prior PVE [57].
Future Liver Remnant Hypertrophy Outcome Measures
Regenerative results of PVE have been extensively reported. Commonly reported hypertrophy outcome parameters are FLR absolute hypertrophy, DH and KGR. FLR absolute hypertrophy is related to the FLR growth in relation to its initial volume. DH shows the increase in the FLR ratio after PVE. KGR is a dynamic outcome measurement, a time-lapse of the regenerative process. It is calculated by dividing DH by the waiting time after PVE, usually in weeks. KGR shows how fast the regenerative process takes place. KGR ≥ 2 has been directly correlated with the absence of PHLF and lower mortality after major hepatectomies [51]. Highly relevant clinical outcomes such as PHLF, peri-operative transfusion requirements, operative times, and complication rates after hepatectomies in patients submitted to liver regeneration therapies have been reported (Table 3). Patients who develop PHLF show longer intensive care and hospital stays and more postoperative complications (infectious; bile leaks; bleeding) [58, 59]. PHLF developed in 10% and 9% of the patients for the group submitted to major hepatectomies with and without PVE, respectively [59]. The five-year overall survival was similar between these two groups, being 38.2% and 37.9% for patients with and without PVE, respectively [59].
After PVE, > 70% of patients undergo the planned liver surgery, and this threshold should be considered acceptable [34, 44, 59]. Nevertheless, 20–30% of patients submitted to PVE will not go through the planned hepatectomy, the main reason being disease progression in the waiting period after PVE. Another reason for not performing the planned liver resection is insufficient growth after PVE in 5–10% of patients [34, 44, 59].
Outcomes for Portal Vein Embolization, Double Vein Embolization and Liver Venous Deprivation
In 2021 two systematic reviews and one randomized trial evaluated the effect of different embolic materials in liver regeneration after PVE, showing the superiority of NBCA over PVA plus coils [44, 45, 58]; the beneficial increment in liver regeneration when segment IV embolization was performed; and the non-influence of neo-adjuvant systemic chemotherapy on PVE regenerative results [44]. In the aforementioned RCT [44], PHLF was 13% for the NBCA group and 27% for the PVA plus coils group (p = 0.27).
Different strategies have been proposed to overcome the potential insufficient regeneration after PVE, including sequential HVE after PVE [17], LVD [20], DVE [21] and ALPPS [14]. Sequential HVE has been shown to increase the volume of the FLR after insufficient PVE. The threshold of 5–10% increase in the FLR absolute growth should be expected 2 weeks after hepatic vein embolization in patients already submitted to PVE [17,18,19]. Interestingly, although sequential hepatic vein embolization is very well tolerated and complication rates are similar to PVE, reports of middle hepatic embolization erroneously recognized and embolized as the right hepatic vein have been reported from different groups [17, 60].
Up to now there were only small retrospective cohorts and systematic reviews comparing the regenerative results of PVE and LVD. The latter technique seems to promote superior regenerative results. One study [47] reported superior KGR and FLR absolute hypertrophy for LVD when compared to PVE. Another study found superior volumetric and functional FLR gain when using LVD compared to PVE [61]. FLR functional gain after LVD was obtained earlier than volumetric hypertrophy [62]. These findings suggest that the planned hepatectomy might be performed (1 or 2 weeks) earlier after LVD when compared to PVE [61, 62]. Interestingly, in these studies, KGR results (1.4%/week) and FLR volume increase (14–19%) for PVE were unusually low, maybe explaining the LVD superiority. Negative studies comparing PVE and LVD have also been reported. A prospective cohort of 14 patients submitted to LVD compared by matched analysis to PVE showed no FLR hypertrophy superiority for LVD before major hepatectomies [63]. Strong evidence about the indications, technique, complications, hypertrophy results and clinical outcomes of LVD and eLVD (extended LVD) as well as DVE will soon be available through ongoing multicentre clinical trials [64, 65]. DVE and LVD have shown similar safety and hypertrophy results, but direct comparative trials are lacking [61, 66, 67].
Abbreviations
- SOP:
-
Standards of Practice
- PVE:
-
Portal vein embolization
- LVD:
-
Liver venous deprivation
- DVE:
-
Double-vein embolization
- HVE:
-
Hepatic vein embolization
- PHLF:
-
Post-hepatectomy liver failure
- ALPPS:
-
Associating liver partition and portal vein ligation for staged hepatectomy
- FLR:
-
Future liver remnant
- TLV:
-
Total liver volume
- MDT:
-
Multidisciplinary team meeting
- NBCA:
-
n-Butyl cyanoacrylate
- PVA:
-
Polyvinyl alcohol
- DH:
-
Degree of hypertrophy
- KGR:
-
Kinetic growth rate
- eLVD:
-
Extended liver venous deprivation
References
Denys A, Bize P, Demartines N, Deschamps F, De Baere T. Quality improvement for portal vein embolization. Cardiovasc Intervent Radiol. 2010;33(3):452–6.
Reddy SK, Barbas AS, Turley RS, et al. A standard definition of major hepatectomy: resection of four or more liver segments. HPB (Oxford). 2011;13(7):494–502.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149(5):713–24.
Garcea G, Ong SL, Maddern GJ. Predicting liver failure following major hepatectomy. Dig Liver Dis. 2009;41(11):798–806.
Karoui M, Penna C, Amin-Hashem M, et al. Influence of preoperative chemotherapy on the risk of major hepatectomy for colorectal liver metastases. Ann Surg. 2006;243(1):1–7.
Zorzi D, Laurent A, Pawlik TM, Lauwers GY, Vauthey JN, Abdalla EK. Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases. Br J Surg. 2007;94(3):274–86.
Shirabe K, Shimada M, Gion T, et al. Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg. 1999;188(3):304–9.
Olthof PB, Coelen RJS, Bennink RJ, et al. Tc-mebrofenin hepatobiliary scintigraphy predicts liver failure following major liver resection for perihilar cholangiocarcinoma. HPB (Oxford). 2017;19(10):850–8.
Cieslak KP, Runge JH, Heger M, Stoker J, Bennink RJ, van Gulik TM. New perspectives in the assessment of future remnant liver. Dig Surg. 2014;31(4–5):255–68.
Asenbaum U, Kaczirek K, Ba-Ssalamah A, et al. Post-hepatectomy liver failure after major hepatic surgery: not only size matters. Eur Radiol. 2018;28(11):4748–56.
de Baere T, Roche A, Elias D, Lasser P, Lagrange C, Bousson V. Preoperative portal vein embolization for extension of hepatectomy indications. Hepatology. 1996;24(6):1386–91.
Di Stefano DR, de Baere T, Denys A, et al. Preoperative percutaneous portal vein embolization: evaluation of adverse events in 188 patients. Radiology. 2005;234(2):625–30.
Alvarez FA, Castaing D, Figueroa R, et al. Natural history of portal vein embolization before liver resection: a 23-year analysis of intention-to-treat results. Surgery. 2018;163(6):1257–63.
Zhang GQ, Zhang ZW, Lau WY, Chen XP. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): a new strategy to increase resectability in liver surgery. Int J Surg. 2014;12(5):437–41.
Schadde E, Raptis DA, Schnitzbauer AA, et al. Prediction of mortality after ALPPS stage-1: an analysis of 320 patients from the international ALPPS registry. Ann Surg. 2015;262(5):780–5 (Discussion 785–6).
Sparrelid E, Jonas E, Tzortzakakis A, et al. Dynamic evaluation of liver volume and function in associating liver partition and portal vein ligation for staged hepatectomy. J Gastrointest Surg. 2017;21(6):967–74.
Hwang S. Sequential preoperative ipsilateral hepatic vein embolization after portal vein embolization to induce further liver regeneration in patients with hepatobiliary malignancy. Ann Surg. 2009;249:608–16.
Hwang S, Lee SG, Ko GY, et al. Preoperative sequential portal and hepatic vein embolization in patients with hepatobiliary malignancy. World J Surg. 2015;39:2990–8.
Munene G, Parker RD, Larrigan J, et al. Sequential preoperative hepatic vein embolization after portal vein embolization for extended left hepatectomy in colorectal liver metastases. World J Surg Oncol. 2013;11:134.
Guiu B, Chevallier P, Denys A, et al. Simultaneous trans-hepatic portal and hepatic vein embolization before major hepatectomy: the liver venous deprivation technique. Eur Radiol. 2016;26(12):4259–67.
Le Roy B, Perrey A, Fontarensky M, et al. Combined preoperative portal and hepatic vein embolization (biembolization) to improve liver regeneration before major liver resection: a preliminary report. World J Surg. 2017;41(7):1848–56.
Ribero D, Chun YS, Vauthey JN. Standardized liver volumetry for portal vein embolization. Semin Intervent Radiol. 2008;25(2):104–9.
DeLand FH, North WA. Relationship between liver size and body size. Radiology. 1968;91(6):1195–8.
Martel G, Cieslak KP, Huang R, van Lienden KP, Wiggers JK, Belbidia A, Dagenais M, Lapointe R, van Gulik TM. Comparison of techniques for volumetric analysis of the future liver remnant: implications for major hepatic resections. HPB. 2015;17(12):1051–7.
de Graaf W, van Lienden KP, Dinant S, et al. Assessment of future remnant liver function using hepatobiliary scintigraphy in patients undergoing major liver resection. J Gastrointest Surg. 2010;14(2):369–78.
Geisel D, Raabe P, Lüdemann L, et al. Gd-EOB-DTPA-enhanced MRI for monitoring future liver remnant function after portal vein embolization and extended hemihepatectomy: a prospective trial. Eur Radiol. 2017;27(7):3080–7.
Yamashita S, Sakamoto Y, Yamamoto S, et al. Efficacy of preoperative portal vein embolization among patients with hepatocellular carcinoma, biliary tract cancer, and colorectal liver metastases: a comparative study based on single-center experience of 319 cases. Ann Surg Oncol. 2017;24(6):1557–68.
Hocquelet A, Sotiriadis C, Duran R, Guiu B, Yamaguchi T, Halkic N, Melloul E, Demartines N, Denys A. Preoperative portal vein embolization alone with biliary drainage compared to a combination of simultaneous portal vein, right hepatic vein embolization and biliary drainage in klatskin tumor. Cardiovasc Intervent Radiol. 2018;41:1885–981.
Ogata S, Belghiti J, Farges O, Varma D, Sibert A, Vilgrain V. Sequential arterial and portal vein embolizations before right hepatectomy in patients with cirrhosis and hepatocellular carcinoma. Br J Surg. 2006;93(9):1091–8.
Yoo H, Kim JH, Ko GY, et al. Sequential transcatheter arterial chemoembolization and portal vein embolization versus portal vein embolization only before major hepatectomy for patients with hepatocellular carcinoma. Ann Surg Oncol. 2011;18(5):1251–7.
Hadi M, Walker C, Desborough M, et al. CIRSE standards of practice on peri-operative anticoagulation management during interventional radiology procedures. Cardiovasc Intervent Radiol. 2021;44(4):523–36.
Moon E, Tam MD, Kikano RN, Karuppasamy K. Prophylactic antibiotic guidelines in modern interventional radiology practice. Semin Intervent Radiol. 2010;27(4):327–37.
Madoff DC, Abdalla EK, Gupta S, et al. Transhepatic ipsilateral right portal vein embolization extended to segment IV: improving hypertrophy and resection outcomes with spherical particles and coils. J Vasc Interv Radiol. 2005;16(2 Pt 1):215–25.
van Lienden KP, van den Esschert JW, de Graaf W, et al. Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol. 2013;36(1):25–34.
Sugawara S, Arai Y, Sone M, et al. Retrospective comparative study of absolute ethanol with n-butyl-2-cyanoacrylate in percutaneous portal vein embolization. J Vasc Interv Radiol. 2019;30(8):1215–22.
Sakuhara Y, Abo D, Hasegawa Y, et al. Preoperative percutaneous transhepatic portal vein embolization with ethanol injection. AJR Am J Roentgenol. 2012;198(4):914–22.
Ogasawara K, Uchino J, Une Y, Fujioka Y. Selective portal vein embolization with absolute ethanol induces hepatic hypertrophy and makes more extensive hepatectomy possible. Hepatology. 1996;23(2):338–45.
Giraudo G, Greget M, Oussoultzoglou E, Rosso E, Bachellier P, Jaeck D. Preoperative contralateral portal vein embolization before major hepatic resection is a safe and efficient procedure: a large single institution experience. Surgery. 2008;143(4):476–82.
Malinowski M, Geisel D, Stary V, et al. Portal vein embolization with plug/coils improves hepatectomy outcome. J Surg Res. 2015;194(1):202–11.
Bent CL, Low D, Matson MB, Renfrew I, Fotheringham T. Portal vein embolization using a nitinol plug (Amplatzer vascular plug) in combination with histoacryl glue and iodinized oil: adequate hypertrophy with a reduced risk of nontarget embolization. Cardiovasc Intervent Radiol. 2009;32(3):471–7.
Carling U, Røsok B, Berger S, Fretland ÅA, Dorenberg E. Portal vein embolization using n-butyl cyanoacrylate-glue: what impact does a central vascular plug have? Cardiovasc Intervent Radiol. 2022;45(4):450–8.
Jaberi A, Toor SS, Rajan DK, et al. Comparison of clinical outcomes following glue versus polyvinyl alcohol portal vein embolization for hypertrophy of the future liver remnant prior to right hepatectomy. J Vasc Interv Radiol. 2016;27(12):1897-1905.e1.
Guiu B, Bize P, Gunthern D, Demartines N, Halkic N, Denys A. Portal vein embolization before right hepatectomy: improved results using n-butyl-cyanoacrylate compared to microparticles plus coils. Cardiovasc Intervent Radiol. 2013;36(5):1306–12.
Luz JHM, Veloso Gomes F, Costa NV, et al. BestFLR trial: liver regeneration at CT before major hepatectomies for liver cancer-a randomized controlled trial comparing portal vein embolization with n-butyl-cyanoacrylate plus iodized oil versus polyvinyl alcohol particles plus coils. Radiology. 2021;299(3):715–24.
Ali A, Ahle M, Björnsson B, Sandström P. Portal vein embolization with n-butyl cyanoacrylate glue is superior to other materials: a systematic review and meta-analysis. Eur Radiol. 2021;31(8):5464–78.
Guiu B, Quenet F, Escal L, et al. Extended liver venous deprivation before major hepatectomy induces marked and very rapid increase in future liver remnant function. Eur Radiol. 2017;27(8):3343–52.
Kobayashi K, Yamaguchi T, Denys A, et al. Liver venous deprivation compared to portal vein embolization to induce hypertrophy of the future liver remnant before major hepatectomy: a single center experience. Surgery. 2020;167(6):917–23.
Najafi A, Schadde E, Binkert CA. Combined simultaneous embolization of the portal vein and hepatic vein (double vein embolization) - a technical note about embolization sequence. CVIR Endovasc. 2021;4(1):43.
Romagnoli S, Fanelli F, Barbani F, et al. CIRSE standards of practice on analgesia and sedation for interventional radiology in adults. Cardiovasc Intervent Radiol. 2020;43(9):1251–60.
de Baere T, Roche A, Vavasseur D, Therasse E, Indushekar S, Elias D, Bognel C. Portal vein embolization: utility for inducing left hepatic lobe hypertrophy before surgery. Radiology. 1993;188(1):73–7.
Shindoh J, Truty MJ, Aloia TA, et al. Kinetic growth rate after portal vein embolization predicts posthepatectomy outcomes: toward zero liver-related mortality in patients with colorectal liver metastases and small future liver remnant. J Am Coll Surg. 2013;216(2):201–9.
Leung U, Simpson AL, Araujo RL, et al. Remnant growth rate after portal vein embolization is a good early predictor of post-hepatectomy liver failure. J Am Coll Surg. 2014;219(4):620–30.
Abulkhir A, Limongelli P, Healey AJ, et al. Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg. 2008;247(1):49–57.
de Graaf W, van den Esschert JW, van Lienden KP, van Gulik TM. Induction of tumor growth after preoperative portal vein embolization: is it a real problem? Ann Surg Oncol. 2009;16(2):423–30.
Hoekstra LT, van Lienden KP, Doets A, Busch OR, Gouma DJ, van Gulik TM. Tumor progression after preoperative portal vein embolization. Ann Surg. 2012;256(5):812–7 (Discussion 817–8).
Lautt WW. Mechanism and role of intrinsic regulation of hepatic arterial blood flow: hepatic arterial buffer response. Am J Physiol. 1985;249(5 Pt 1):G549–56.
Giglio MC, Giakoustidis A, Draz A, et al. Oncological outcomes of major liver resection following portal vein embolization: a systematic review and meta-analysis. Ann Surg Oncol. 2016;23(11):3709–17.
Soykan EA, Aarts BM, Lopez-Yurda M, Kuhlmann KFD, Erdmann JI, Kok N, van Lienden KP, Wilthagen EA, Beets-Tan RGH, van Delden OM, Gomez FM, Klompenhouwer EG. Predictive factors for hypertrophy of the future liver remnant after portal vein embolization: a systematic review. Cardiovasc Intervent Radiol. 2021;44(9):1355–66.
Ironside N, Bell R, Bartlett A, McCall J, Powell J, Pandanaboyana S. Systematic review of perioperative and survival outcomes of liver resections with and without preoperative portal vein embolization for colorectal metastases. HPB (Oxford). 2017;19(7):559–66.
Le Roy B, Gallon A, Cauchy F, et al. Combined biembolization induces higher hypertrophy than portal vein embolization before major liver resection. HPB (Oxford). 2020;22(2):298–305.
Guiu B, Quenet F, Panaro F, et al. Liver venous deprivation versus portal vein embolization before major hepatectomy: future liver remnant volumetric and functional changes. Hepatobiliary Surg Nutr. 2020;9(5):564–76.
Deshayes E, Schadde E, Piron L, Quenet F, Guiu B. Extended Liver Venous Deprivation Leads to a Higher Increase in Liver Function that ALPPS in Early Assessment: A comment to "Sparrelid, E. et al. Dynamic Evaluation of Liver Volume and Function in Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy. Journal of Gastrointestinal Surgery (2017)". J Gastrointest Surg. 2017;21(10):1754–5.
Böning G, Fehrenbach U, Auer TA, et al. Liver venous deprivation (LVD) versus portal vein embolization (PVE) alone prior to extended hepatectomy: a matched pair analysis. Cardiovasc Intervent Radiol. 2022;45(7):950–7.
Deshayes E, Piron L, Bouvier A, et al. Study protocol of the HYPER-LIV01 trial: a multicenter phase II, prospective and randomized study comparing simultaneous portal and hepatic vein embolization to portal vein embolization for hypertrophy of the future liver remnant before major hepatectomy for colo-rectal liver metastases. BMC Cancer. 2020;20(1):574.
Korenblik R, Olij B, Aldrighetti LA, et al. Dragon 1 protocol manuscript: training, accreditation, implementation and safety evaluation of portal and hepatic vein embolization (PVE/HVE) to accelerate future liver remnant (FLR) hypertrophy. Cardiovasc Intervent Radiol. 2022;45(9):1391–8.
Heil J, Korenblik R, Heid F, et al. Preoperative portal vein or portal and hepatic vein embolization: DRAGON collaborative group analysis. Br J Surg. 2021;108(7):834–42.
Della Corte A, Santangelo D, Augello L, et al. Single-center retrospective study comparing double vein embolization via a trans-jugular approach with liver venous deprivation via a trans-hepatic approach. Cardiovasc Intervent Radiol. 2023;46(12):1703–12.
Balzan S, Belghiti J, Farges O, et al. The “50–50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005;242(6):824–8 (Discussion 828–9).
Rahbari NN, Reissfelder C, Koch M, Elbers H, Striebel F, Büchler MW, Weitz J. The predictive value of postoperative clinical risk scores for outcome after hepatic resection: a validation analysis in 807 patients. Ann Surg Oncol. 2011;18(13):3640–9.
Funding
Open access funding provided by FCT|FCCN (b-on). None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tiago Bilhim is a paid consultant for Merit Medical and has received speaker fees for Philips Medical, Cook Medical, and Terumo and is a stock holder for EmbolX. Boris Guiu is a consultant for Roche, Astra Zeneca, BMS, Boston Scientific, Guerbet, Terumo, and Canon Medical. All other authors declare that they have no conflict of interest.
Consent for publication
All authors had control of the publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bilhim, T., Böning, G., Guiu, B. et al. CIRSE Standards of Practice on Portal Vein Embolization and Double Vein Embolization/Liver Venous Deprivation. Cardiovasc Intervent Radiol (2024). https://doi.org/10.1007/s00270-024-03743-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00270-024-03743-8