Abstract
Background
Reports of an increased proportion of complicated appendicitis during the Covid-19 pandemic suggest a worse outcome due to delay secondary to the restrained access to health care, but may be explained by a concomitant decrease in uncomplicated appendicitis. We analyze the impact of the pandemic on the incidences of complicated and uncomplicated appendicitis.
Method
We did a systematic literature search in the PubMed, Embase and Web Of Science databases on December 21, 2022 with the search terms (appendicitis OR appendectomy) AND (“COVID” OR SARS-Cov2 OR “coronavirus”). Studies reporting the number of complicated and uncomplicated appendicitis during identical calendar periods in 2020 and the pre-pandemic year(s) were included. Reports with indications suggesting a change in how the patients were diagnosed and managed between the two periods were excluded. No protocol was prepared in advance. We did random effects meta-analysis of the change in proportion of complicated appendicitis, expressed as the risk ratio (RR), and of the change in number of patients with complicated and uncomplicated appendicitis during the pandemic compared with pre-pandemic periods, expressed as the incidence ratio (IR). We did separate analyses for studies based on single- and multi-center and regional data, age-categories and prehospital delay.
Results
The meta-analysis of 100,059 patients in 63 reports from 25 countries shows an increase in the proportion of complicated appendicitis during the pandemic period (RR 1.39, 95% confidence interval (95% CI 1.25, 1.53). This was mainly explained by a decreased incidence of uncomplicated appendicitis (incidence ratio (IR) 0.66, 95% CI 0.59, 0.73). No increase in complicated appendicitis was seen in multi-center and regional reports combined (IR 0.98, 95% CI 0.90, 1.07).
Conclusion
The increased proportion of complicated appendicitis during Covid-19 is explained by a decrease in the incidence of uncomplicated appendicitis, whereas the incidence of complicated appendicitis remained stable. This result is more evident in the multi-center and regional based reports. This suggests an increase in spontaneously resolving appendicitis due to the restrained access to health care. This has important principal implications for the management of patients with suspected appendicitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A large number of studies and meta-analyses have reported an increase in the proportion of complicated appendicitis during the Covid-19 pandemic, suggesting increased delay as explanation [1,2,3,4,5,6,7]. Some studies also report a concomitant decrease in the number of uncomplicated appendicitis, suggesting that undiagnosed uncomplicated appendicitis may resolve without treatment due to the restrained access to health care [4]. As the proportion of complicated appendicitis is determined by the number of complicated appendicitis as numerator and the total number of patients with appendicitis as denominator, the concomitant decrease in the number of patients with uncomplicated appendicitis must also have had an impact [4]. It is known that variations in the incidence rate of uncomplicated appendicitis are more closely associated with the proportion of complicated appendicitis [8], whereas the impact of the Covid pandemic on the proportion of complicated appendicitis has been analyzed in several meta-analyses we have not seen any previous analysis of the impact on the incidences of complicated and uncomplicated appendicitis separately [2,3,4,5,6,7].
The aim of this report is to analyze the impact of the Covid-19 pandemic on the incidence of complicated and uncomplicated appendicitis. The hypothesis is that an increase in the proportion of complicated appendicitis during the pandemic period may be the secondary effect of a decrease in the incidence of uncomplicated appendicitis rather than an increase in the incidence of complicated appendicitis [9]. This would suggest that cases of uncomplicated appendicitis were allowed to resolve undetected.
Methods
Study selection and search strategy
We follow the PRISMA (preferred reporting items for systematic reviews and meta-analysis) guidelines [10]. The PubMed, Embase and Web Of Science databases were searched on December 21, 2022 with the search terms (appendicitis OR appendectomy) AND (“COVID” OR SARS-Cov2 OR “coronavirus”). We also included all references from previously published meta-analysis on this issue to the search.
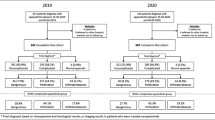
After removal of duplicates from the search strategy, titles and abstracts were screened for potentially eligible reports, which were reviewed in full text. RA and MA independently reviewed the records and reports. RA is responsible for the final selection. We included studies reporting number of patients with uncomplicated and complicated appendicitis treated within the 1st wave of the COVID-19 pandemic and the corresponding numbers during a reference period with the corresponding calendar dates in the preceding year(s), to control for seasonality. For studies reporting number of patients from more than one pre-pandemic year we used the mean numbers for these years. If result was reported as percentage the exact numbers were estimated from the percentages and total numbers. Studies with available full text in English, German, or Scandinavian language were eligible for selection.
Reasons for not including a report were: unclear definition of complicated and uncomplicated appendicitis [11, 12], indications suggesting change in referral area during the pandemic [13, 14], and inconsistent or incomplete data [15, 16]. Studies reporting similar number of patients treated non-operatively with antibiotics in the two periods were included but studies that only reported results from non-operative management or with strong increase in use of non-operative management for assumed uncomplicated appendicitis during the pandemic period were excluded [17,18,19,20]. Two studies with extremely small samples were also excluded [21, 22]. After exclusions there remained 63 reports for the meta-analysis. The study selection process is pictured in the PRISMA flowchart (Supplementary Fig. 1).
Data items
The included studies report on retrospective cohorts of patients treated for appendicitis during the pandemic and a reference period identified through administrative registers. We classified the outcome as complicated and uncomplicated based on the description of the severity in the reports. However, the classification of the grade of severity of appendicitis is not uniform between the reports. Some use the ICD codes only but most refer in general terms to information from imaging (to detect abscesses or phlegmon), perioperative findings or histopathologic examination of the specimen. Only a few studies mention histopathologic depth of inflammation or presence of necrosis in general terms but with no details on the criteria used for the grading of severity. Many studies just use terms like “simple,” “uncomplicated,” “complicated,” “perforated,” “abscess” or “phlegmon” without reporting the criteria used for the classification. Patients that had been treated non-operatively for abscess or phlegmon are classified as complicated and patients treated non-operatively for assumed uncomplicated appendicitis as uncomplicated. The classification of gangrenous appendicitis as complicated or uncomplicated varies between the studies. We have assigned gangrenous appendicitis as complicated if the numbers are reported. Some studies use only the ICD-10 codes for the classification of severity, which has been criticized for unclear definitions [23]. Some classify K35.3 (Acute appendicitis with localized peritonitis) as complicated and others as uncomplicated.
We have classified the reports related to the age categories as children, adults, and all ages. The definition of children varied from 12 to 18 years. If age was not specified, we classified the report as representing all ages. The study base for the reports is classified as single- or multi-center, and as regional for reports based on larger population based registers. We extracted data on delay before arrival to hospital from information on the time from onset of symptoms to hospitalization or operation. If this duration of symptoms differed significantly between the pandemic and the pre-pandemic periods we accepted this as an indication of delay associated with the Covid-19 pandemic, classified as “1” if significant and “0” if not significant. Too few reports give information on the use of diagnostic imaging for a meaningful analysis. Due to the heterogeneity of the reports and incomplete data on various factors we did not find it meaningful to prepare a protocol in advance as we were only interested in the change in the number of complicated and uncomplicated appendicitis during the two study periods, irrespective of how they were defined, assuming that the criteria used did not change between these periods. We excluded all studies with indications of a change in management during the pandemic period.
Statistical analyses
The extracted data were analyzed in three ways:
-
(1)
We did a random effects meta-analysis of the differences in the proportion of complicated appendicitis between the pandemic and pre-pandemic periods—expressed as the risk ratio (RR), visualized in a forest plot (Fig. 1).
-
(2)
We did separate random effects meta-analyses of the ratio of the number of patients with complicated and uncomplicated appendicitis between the pandemic and pre-pandemic periods, expressed as the incidence ratio (IR) with exact confidence limits, visualized in forest plots. The number of patients observed during the pandemic period is compared with the numbers in previous year(s). Separate analyses were performed for subsets according to the type of origin of the study (single- or multi-center or regional) and the included population (children, adult, or all ages).
-
(3)
We estimated the incidence ratio (IR) of complicated and uncomplicated appendicitis associated with the Covid-19 pandemic using a multilevel negative binomial regression model. The model was estimated using Bayesian inference and weighted by the square root of each reports sample size. Included in the model were covariates for origin of study (single- or multi-center or regional) and the included population (pediatric, adult, or all ages). The marginal posterior medians are reported as point estimates, alongside a compatibility interval (CoI) represented by the 2.5% and 97.5% percentiles of the posterior distribution.
Heterogeneity was analyzed with the I^2 test. Presence of bias was analyzed with funnel-plots and the egger test. Statistical analyses were performed using Stata 17 (StataCorp, College Station, TX, USA), R 4.0.4, and CmdStan 2.30.1.
Results
Descriptive results of selected studies
The primary search resulted in 836 unique references. After an initial screening of title and abstracts there remained 245 reports. A review of the full text resulted in exclusion of another 182 reports, leaving 63 reports with 100,059 patients from 25 countries (22,162 patients with complicated and 23,853 with uncomplicated appendicitis during the pandemic period, compared with 23,737 patients with complicated and 30,307 with uncomplicated appendicitis during the pre-pandemic period (Tables 1 and 2). The majority (41) were reports from single centers, 11 from multi-centers and 11 from geographic regions. Some 24 reports include all ages, 23 include only adults and 16 only pediatric patients.
The median duration of the pandemic study period was 72 days (range 27–365). The reference period was the same dates in previous year(s) as the for the pandemic period, in 42 reports from 2019, 12 reports included 2018 and 2019, and 9 reports included three years (2017–2019). For the reports with more than one year for the reference period we used the mean number of patients over the years for the analyses. The prehospital duration of symptoms was significantly longer, suggesting delay in 17 of 33 studies that reported this information (Table 2).
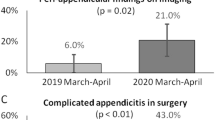
Impact on proportion of complicated appendicitis
The Covid pandemic was associated with an increased risk ratio (RR) of the proportion of complicated appendicitis compared to the pre-pandemic period (RR 1.39, confidence interval (CI) 1.25, 1.53) (Fig. 1 and Table 3). This was most marked for the single center reports (RR 1.61, CI 1.37, 1.88), while the increase was smaller in the multi-center and regional based reports (RR 1.13, CI 1.08, 1.19). The meta-analysis shows strong heterogeneity within and between the groups reflecting the differences in definitions of outcome, in level of restrained access and size of reports. This is also evident from the funnel plot, Supplementary Fig. 2. The Egger test is strongly significant (p < 0.001) suggesting small study bias.
Impact on number of complicated and uncomplicated appendicitis
The change in the absolute number of patients with complicated and uncomplicated appendicitis between the pre-pandemic and pandemic periods according to the type of report is graphically shown in Fig. 2. These graphs show a clear difference in trends between type of source. For complicated appendicitis the smaller, single center studies, show a pattern that suggest regression to the mean with some decreasing and some increasing numbers. This can be expected given the small numbers and short observation period. For most of the studies the numbers of complicated appendicitis remain at a stable level. For the numbers of uncomplicated appendicitis there is a marked trend toward a lower number during the pandemic period compared with the pre-pandemic period in most studies.
Graphical presentation linking the observed number of patients during the pre-pandemic and pandemic periods for each report, according to type of study base and severity of appendicitis. The y-axis is logarithmic. The smaller studies show large heterogeneity and also pattern suggesting regression to the mean. The larger studies show mainly stable incidence of complicated appendicitis and a trend toward decreasing incidence of uncomplicated appendicitis
The meta-analysis comparing the number of complicated appendicitis before and during the Covid-19 pandemic period, expressed as the Incidence Ratio (IR), shows an increase overall (IR 1.15, CI 1.04, 1.27), most marked in children (IR 1.29, CI 1.05, 1.57) but with a marked difference between the single center and the other source types. When the reports from multi-center and regional are combined there is no increase in the number of complicated appendicitis (IR 0.98, CI 0.90, 1.07) (Table 3, Fig. 3).
For uncomplicated appendicitis the meta-analysis shows a marked decrease in all the subsets with an IR of 0.66 (CI 0.59; 0.73) overall, with the strongest decrease in the single center studies (IR 0.62, CI 0.53: 0.73) and in reports based on adults (IR 0.57, CI 0.48; 0.69) (Table 3, Fig. 4).
Forest plot of the meta-analyses comparing the number of uncomplicated appendicitis before and during the Covid-19 pandemic, expressed as the incidence ratio. For the larger studies the incidence ratio is significant lower than 1.0, supporting a decrease in the incidence of uncomplicated appendicitis during the pandemic
Finally, the multilevel negative binomial regression model revealed that the posterior probability that the IR for complicated appendicitis associated with the Covid-19 pandemic was greater than 1 was 98.5% (median adjusted IR = 1.13, Compatibility Interval (CoI) = 1.01, 1.26), after having adjusted for both origin of study and included population. This posterior probability is the product of our Bayesian analysis [24], and can be interpreted as the proportion of all possible IR estimates which are, given the data and the model, compatible with the assertion that the association is greater than the null (IR = 1)—i.e., the probability that there was a difference between the two points in time. Similarly, the posterior probability that the IR for uncomplicated appendicitis associated with the Covid-19 pandemic was less than 1 was > 99.9% (median adjusted IR = 0.64, CoI = 0.57, 0.72). When removing single center studies, the posterior probability that the IR for complicated appendicitis associated with the Covid-19 pandemic was greater than 1 was 59.0% (median adjusted IR = 0.99, 95% CoI = 0.98, 1.10), i.e., when excluding single center studies the probability that there was a difference between the two points in time was much lower. For uncomplicated appendicitis on the other hand, the posterior probability that the IR associated with Covid-19 pandemic was less than 1 remained high, > 99.9%, with a median adjusted IR of 0.71 (95% CoI = 0.61, 0.82).
Overall, our analyses suggest strong evidence that uncomplicated appendicitis decreased substantially during the pandemic whereas the pandemic had little impact on the incidence of complicated appendicitis.
Association with delay
Delay was associated with higher proportion of complicated appendicitis, and higher incidence ratio of complicated appendicitis but had also the lowest incidence ratio of uncomplicated appendicitis (Table 3).
Quality of the reports and risk for bias
The studies show important heterogeneity with an I^2 statistic > 90% in all analyses. This is also evident from funnelplots of the IR of complicated and uncomplicated appendicitis (Supplementary Fig. 3 and 4). Possible reasons for this may be differences in level of limitation in access to health care during the pandemic (the exposure) and in definitions for grading the severity of appendicitis (the outcome). The sample size and length of the inclusion period also varies. Because of this heterogeneity a formal estimation of the overall effect of the pandemic on the incidence and outcome of appendicitis is not possible. However, the reports internal validity should be acceptable as it seems likely that the definition of the severity of appendicitis should be identical in the pandemic and reference periods for each of the type of sources, and the catchment population should also be identical as we have excluded studies showing indications suggesting changes in referrals. This is especially true for the regional studies, which should have higher attention for the interpretation of the results.
Discussion
In accordance with many previous reports, we found an increase in the proportion of complicated appendicitis during the first wave of the Covid-19 pandemic, compared with a representative pre-pandemic period. A common interpretation is that this indicates progression of severity because of delay. However, an increased proportion of complicated appendicitis (i.e., “perforation rate”) can be the result of both an increase in the number of complicated appendicitis as well as a decrease in the number of uncomplicated appendicitis [25].
In this meta-analysis, we found that the Covid-19 pandemic was associated with a consistent decrease in the number of uncomplicated appendicitis and a stable incidence of complicated appendicitis in the more reliable study sources. The increased proportion of complicated appendicitis during the pandemic is thus not a sign of an increased risk for the progression of the severity due to the limited access to health care, but the results in this meta-analysis rather suggest an increase in spontaneous resolution of uncomplicated appendicitis. This interpretation is also proposed in many reports [7, 26,27,28,29,30, 30,31,32,33,34,35,36,37,38].
Early diagnosis and treatment is by tradition regarded as important for preventing the progression of the inflammation that will eventually lead to perforation if left untreated. Due to limited data of questionable quality we could not analyze the direct impact of prehospital duration of symptoms, but the overall impact of the restrained access to health care in the present study support previous reports showing that an association between prehospital delay and the proportion of complicated appendicitis may be explained by selection of complicated cases with time as the uncomplicated cases resolve undiagnosed [9, 39, 40]. This is also supported by the safety of expectant management with in-hospital observation in up to 36 h or deferring operations to daytime [41, 42].
When interpreting the findings of this meta-analysis several limitations should be borne in mind. The studies show important heterogeneity. This is expected as there are probably large differences in the exposure (decrease in access to health care) as well as the outcome (definition of severity of appendicitis) between the studies. However, we can assume that within each report the definitions should be consistent over the two study periods, and consequently the direction of the changes should be consistent, except for smaller studies where regression toward the mean is a possible explanation. The results of the larger multi-center and regional studies also show a more homogenous direction of the association with a decrease in the incidence of uncomplicated and stable incidence of complicated appendicitis during the pandemic.
All included reports are retrospective observational studies from many different types of sources. To avoid bias due to seasonality we have only included reports that use the same calendar period for comparison between the pandemic and reference periods. We have excluded some reports with large differences in age and sex distribution between the study periods which suggest changes in the catchment population due to changed referral pathways. We have also excluded reports with large changes in the use of non-operative treatment with antibiotics for uncomplicated appendicitis. We have included six reports from Germany [26, 27, 43,44,45,46]. Some of these studies may be partly overlapping. Due to limited information on the geographical location of the included clinics, we cannot adjust for this possible overlap.
The findings in this study support the growing body of evidence showing that complicated and uncomplicated appendicitis are two different entities, one that progress to complicated appendicitis early and another that resolve spontaneously [8, 40, 47]. This has important principal implications for the management of patients with suspicion of appendicitis also outside the pandemic. The primary goal is the early detection and treatment of complicated appendicitis, whereas the detection and treatment of uncomplicated appendicitis are less urgent as they rarely progress to perforation but may heal spontaneously, as suggested by the results in this meta-analysis. The increased use of diagnostic imaging during the last decades has led to the increased detection of mild, uncomplicated appendicitis that was previously allowed to heal undetected [19, 31,32,33]. This increased detection and treatment of mild, uncomplicated appendicitis has been associated with a decrease in the proportion of complicated appendicitis but has not had any impact on the incidence rate of complicated appendicitis [48]. Spontaneous resolution of uncomplicated appendicitis has also an implication on the current trend toward antibiotics treatment of uncomplicated appendicitis. Two placebo-controlled studies show same healing rate irrespective if the patients were given placebo or antibiotics [49, 50]. This strongly suggests that the effect seen in studies of antibiotics treatment of uncomplicated appendicitis is to a large extent the result of spontaneous healing. This supports expectant management of patients with uncomplicated appendicitis.
Conclusion
We confirm previous reports of an increase in the proportion of complicated appendicitis during the Covid-19 pandemic. However, a more detailed analysis shows that this is the result of a substantial decrease in the incidence of uncomplicated appendicitis, whereas the incidence of complicated appendicitis remained stable.
This result suggests that the restrained access to health care during the Covid-19 pandemic resulted in an increase in resolution of undetected uncomplicated appendicitis. This support previous indications that complicated and uncomplicated appendicitis are different entities, and that uncomplicated appendicitis may resolve without treatment. This has important principal implications on the management of patients with suspicion of appendicitis also outside the pandemic.
References
Emile S, Hamid H, Khan S, Davis G (2021) Rate of application and outcome of non-operative management of acute appendicitis in the setting of COVID-19: systematic review and meta-analysis. J Gastrointest Surg 25:1905–1915. https://doi.org/10.1007/s11605-021-04988-1
Grossi U, Gallo G, Ortenzi M et al (2022) Changes in hospital admissions and complications of acute appendicitis during the COVID-19 pandemic: a systematic review and meta-analysis. Health Sci Rev Oxf Engl 3:100021. https://doi.org/10.1016/j.hsr.2022.100021
Kariya A, Krutsri C, Singhatas P et al (2022) Incidence of complicated appendicitis during the COVID-19 pandemic: a systematic review and meta-analysis. Int J Surg OPEN. https://doi.org/10.1016/j.ijso.2022.100512
Kohler F, Muller S, Hendricks A et al (2021) Changes in appendicitis treatment during the COVID-19 pandemic–a systematic review and meta-analysis. Int J Surg. https://doi.org/10.1016/j.ijsu.2021.106148
Mogharab V, Ostovar M, Ruszkowski J et al (2022) Global burden of the COVID-19 associated patient-related delay in emergency healthcare: a panel of systematic review and meta-analyses. Glob Health. https://doi.org/10.1186/s12992-022-00836-2
Motazedian G, Aryanpoor P, Rahmanian E et al (2022) Incidence of pediatric perforated appendicitis during the COVID pandemic; a systematic review and meta-analysis. Arch Acad Emerg Med. https://doi.org/10.22037/aaem.v10i1.1421
Pogorelic Z, Anand S, Auvela T et al (2022) Incidence of complicated appendicitis during the COVID-19 pandemic versus the pre-pandemic period: a systematic review and meta-analysis of 2782 pediatric appendectomies. Diagnostics. https://doi.org/10.3390/diagnostics12010127
Andersson R, Hugander A, Thulin A et al (1994) Indications for operation in suspected appendicitis and incidence of perforation. BMJ 308:107–110
Andersson RE (2016) Does delay of diagnosis and treatment in appendicitis cause perforation? World J Surg 40:1315–1317. https://doi.org/10.1007/s00268-016-3489-y
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. https://doi.org/10.1136/bmj.n71
Zahra M, Kashif M, Ahmed S et al (2021) Influence of Covid -19 on the management of appendicitis. Pak J Med Health Sci 15:1718–1721. https://doi.org/10.53350/pjmhs211571718
Rusconi F, Di Fabrizio V, Puglia M et al (2021) Delayed presentation of children to the emergency department during the first wave of COVID-19 pandemic in Italy: area-based cohort study. Acta Paediatr Int J Paediatr 110:2796–2801. https://doi.org/10.1111/apa.16019
Wolf S, Schrempf M, Vlasenko D et al (2022) Acute appendicitis during the COVID-19 pandemic-changes in incidence and clinical presentation but not in patients’ outcome. Int J Qual Health CARE. https://doi.org/10.1093/intqhc/mzac005
Turanli S, Kiziltan G (2021) Did the COVID-19 pandemic cause a delay in the diagnosis of acute appendicitis? WORLD J Surg 45:18–22. https://doi.org/10.1007/s00268-020-05825-3
Ho S, Lau J, Wang C et al (2021) Impact of coronavirus disease 2019 (COVID-19) on acute appendicitis in Hong Kong: retrospective cohort study in a local cluster hospital. Surg Pract 25:25–31. https://doi.org/10.1111/1744-1633.12476
Ho SL, Wong KF, Leung SK (2021) Impact of COVID-19 on the clinical course of acute appendicitis. Surg Pract 25:18. https://doi.org/10.1111/1744-1633.12519
Kvasnovsky C, Shi Y, Rich B et al (2021) Limiting hospital resources for acute appendicitis in children: lessons learned from the US epicenter of the COVID-19 pandemic. J Pediatr Surg 56:900–904. https://doi.org/10.1016/j.jpedsurg.2020.06.024
Somers K, AbdElwahab S, Raza M et al (2021) Impact of the COVID-19 pandemic on management and outcomes in acute appendicitis: Should these new practices be the norm? Surg J R Coll Surg Edinb Irel 19:E310–E317. https://doi.org/10.1016/j.surge.2021.01.009
Place R, Lee J, Howell J (2020) Rate of pediatric appendiceal perforation at a children’s hospital during the CoVID-19 pandemic compared with the previous year. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2020.27948
Gerall C, DeFazio J, Kahan A et al (2021) Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg 56:905–910. https://doi.org/10.1016/j.jpedsurg.2020.10.008
Allen M, Thompson B, Atkinson B et al (2021) Emergency department presentations in the southern district of new Zealand during the 2020 COVID-19 pandemic lockdown. Emerg Med Australas 33:534–540. https://doi.org/10.1111/1742-6723.13749
Sheath C, Abdelrahman M, MacCormick A, Chan D (2021) Paediatric appendicitis during the COVID-19 pandemic. J Paediatr Child Health 57:986–989. https://doi.org/10.1111/jpc.15359
Andersson RE (2015) Confusing diagnosis coding prevents historical and international comparisons. Diagnosing should be unambiguous and consistent. Lakartidningen 112:DDWH
Bendtsen M (2018) A gentle introduction to the comparison between null hypothesis testing and bayesian analysis: reanalysis of two randomized controlled trials. J Med Internet Res 20:e10873. https://doi.org/10.2196/10873
Neufeld M, Sanchez S, Drake F (2021) Handle With care: use of proportions to assess changes in acute appendicitis during the 2020 COVID-19 “Surge.” J Am Coll Radiol 18:893–894. https://doi.org/10.1016/j.jacr.2021.02.027
Maneck M, Gunster C, Meyer H et al (2021) Influence of COVID-19 confinement measures on appendectomies in Germany-a claims data analysis of 9797 patients. Langenbecks Arch Surg 406:385–391. https://doi.org/10.1007/s00423-020-02041-4
Willms A, Oldhafer K, Conze S et al (2021) Appendicitis during the COVID-19 lockdown: results of a multicenter analysis in Germany. Langenbecks Arch Surg 406:367–375. https://doi.org/10.1007/s00423-021-02090-3
van Amstel P, El Ghazzaoui A, Hall N et al (2022) Paediatric appendicitis: international study of management in the COVID-19 pandemic. Br J Surg 109:1044–1048. https://doi.org/10.1093/bjs/znac239
Fersahoglu M, Ciyiltepe H, Fersahoglu A et al (2022) A comparison of patients who have appendectomy during the COVID-19 pandemic period with the period before the pandemic. Ulus Travma Ve Acil Cerrahi Derg-Turk J Trauma Emerg Surg 28:170–174. https://doi.org/10.14744/tjtes.2021.57946
Neufeld MY, Bauerle W, Eriksson E et al (2021) Where did the patients go? Changes in acute appendicitis presentation and severity of illness during the coronavirus disease 2019 pandemic: a retrospective cohort study. Surg U S 169:808–815. https://doi.org/10.1016/j.surg.2020.10.035
Horst K, Kolbe A, McDonald J et al (2021) Imaging pediatric acute appendicitis during the coronavirus disease 2019 (COVID-19) pandemic: collateral damage is variable. Pediatr Radiol 51:1991–1999. https://doi.org/10.1007/s00247-021-05128-2
Mowbray N, Hurt L, Powell-Chandler A et al (2021) Where have all the appendicectomies gone? Ann R Coll Surg Engl 103:250–254. https://doi.org/10.1308/rcsann.2020.7128
Meric S, Aktokmakyan T, Tokocin M et al (2021) Comparative analysis of the management of acute appendicitis between the normal period and COVID-19 pandemic. Ulus Travma Ve Acil Cerrahi Derg-Turk J Trauma Emerg Surg 27:22–25. https://doi.org/10.14744/tjtes.2020.46487
Hayatghaibi S, Trout A, Dillman J et al (2021) Trends in pediatric appendicitis and imaging strategies during Covid-19 in the United States. Acad Radiol 28:1500–1506. https://doi.org/10.1016/j.acra.2021.08.009
Patel V, Ye K, In H, Scheinfeld M (2021) Non-operative management for acute appendicitis during the COVID-19 pandemic does not increase the rate of complications. J Gastrointest Surg 25:1327–1329. https://doi.org/10.1007/s11605-020-04844-8
Rosenthal MG, Fakhry SM, Morse JL et al (2021) Where did all the appendicitis go? Impact of the COVID-19 pandemic on volume, management, and outcomes of acute appendicitis in a nationwide, multicenter analysis. Ann Surg. https://doi.org/10.1097/AS9.0000000000000048
Tamirian R, Klein M, Chui P et al (2022) Acute appendicitis during the COVID-19 pandemic: a multicenter, retrospective analysis from the US epicenter. Am Surg. https://doi.org/10.1177/00031348221103649
Scheijmans J, Borgstein A, Puylaert C et al (2021) Impact of the COVID-19 pandemic on incidence and severity of acute appendicitis: a comparison between 2019 and 2020. BMC Emerg Med. https://doi.org/10.1186/s12873-021-00454-y
Luckmann R (1989) Incidence and case fatality rates for acute appendicitis in California. a population-based study of the effects of age. Am J Epidemiol 129:905–918. https://doi.org/10.1093/oxfordjournals.aje.a115224
Andersson RE (2007) The natural history and traditional management of appendicitis revisited: spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J Surg 31:86–92
Li J, Xu R, Hu D-M et al (2019) Effect of delay to operation on outcomes in patients with acute appendicitis: a systematic review and meta-analysis. J Gastrointest Surg Off J Soc Surg Aliment Tract 23:210–223. https://doi.org/10.1007/s11605-018-3866-y
United Kingdom National Surgical Research Collaborative, Bhangu A (2014) Safety of short, in-hospital delays before surgery for acute appendicitis: multicentre cohort study, systematic review, and meta-analysis. Ann Surg 259:894–903. https://doi.org/10.1097/SLA.0000000000000492
Kohler F, Acar L, van den Berg A et al (2021) Impact of the COVID-19 pandemic on appendicitis treatment in Germany-a population-based analysis. Langenbecks Arch Surg 406:377–383. https://doi.org/10.1007/s00423-021-02081-4
Schäfer F-M, Meyer J, Kellnar S et al (2021) Increased incidence of perforated appendicitis in children during COVID-19 pandemic in a Bavarian multi-center study. Front Pediatr 9:683607. https://doi.org/10.3389/fped.2021.683607
Steffani M, Merz C, Stoss C et al (2021) Effects of the first COVID-19 wave on visceral surgery a retrospective comparison of case numbers from a university hospital and a primary care hospital. Chirurg 92:559–566. https://doi.org/10.1007/s00104-021-01434-5
Wichmann D, Schweizer U, Wulff D et al (2021) Incidence of perforated appendicitis during the COVID-19 pandemic: lessons to be considered in the second wave. J Gastrointest Surg 25:2404–2406. https://doi.org/10.1007/s11605-021-04915-4
Andersson RE (2008) Resolving appendicitis is common: further evidence. Ann Surg 247:553. https://doi.org/10.1097/SLA.0b013e318166177b. (Author reply 553)
Livingston EH, Woodward WA, Sarosi GA, Haley RW (2007) Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg 245:886–892. https://doi.org/10.1097/01.sla.0000256391.05233.aa
Park HC, Kim MJ, Lee BH (2017) Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. Br J Surg 104:1785–1790. https://doi.org/10.1002/bjs.10660
Salminen P, Sippola S, Haijanen J et al (2022) Antibiotics versus placebo in adults with CT-confirmed uncomplicated acute appendicitis (APPAC III): randomized double-blind superiority trial. Br J Surg 109:503–509. https://doi.org/10.1093/bjs/znac086
Aharoni M, Barash Y, Zager Y et al (2021) Management of acute appendicitis during the COVID-19 pandemic: a single tertiary center experience. Isr Med Assoc J 23:269–273
Al-Abid M, Petrucci R, Preda T et al (2022) Reduced number of admissions with acute appendicitis but not severe acute appendicitis at two Sydney hospitals during the first COVID-19 lockdown period. ANZ J Surg 92:1737–1741. https://doi.org/10.1111/ans.17793
Alakus U, Turker B, Sarigoz T, Meral U (2022) Impact of coronavirus disease on acute appendicitis cases. Ulus Travma Ve Acil Cerrahi Derg-Turk J Trauma Emerg Surg 28:285–289. https://doi.org/10.14744/tjtes.2020.38632
Ali S, Khan MA, Rehman IU, Uzair M (2020) Impact of covid 19 pandemic on presentation, treatment and outcome of paediatric surgical emergencies. J Ayub Med Coll Abbottabad JAMC 32(Suppl 1):S621–S624
Angeramo CA, Schlottmann F (2021) Impact of COVID-19 on surgical residency programs: a glass half-full reflection. Int J Surg Lond Engl 89:105958. https://doi.org/10.1016/j.ijsu.2021.105958
Bada-Bosch I, de Agustín JC, de la Torre M et al (2021) Pediatric surgical activity during the SARS-CoV-2 pandemic: experience at a tertiary hospital. Cirugia Pediatr Organo Soc Espanola Cirugia Pediatr 34:28–33
Bellini T, Rotulo GA, Carlucci M et al (2021) Complicated appendicitis due to diagnosis delay during lockdown period in Italy. Acta Paediatr Int J Paediatr 110:1959–1960. https://doi.org/10.1111/apa.15756
Burgard M, Cherbanyk F, Nassiopoulos K et al (2021) An effect of the COVID-19 pandemic: significantly more complicated appendicitis due to delayed presentation of patients! PLoS ONE. https://doi.org/10.1371/journal.pone.0249171
Büyükakıncak S, Turan M, Ateş G et al (2022) The effect of the COVID-19 pandemic on acute appendicitis cases. J Exp Clin Med Turk 39:398–402. https://doi.org/10.52142/omujecm.39.2.17
Celik S, Lapsekili E, Alakus U (2022) Impact of the COVID-19 pandemic on emergency general surgery outcomes: a single-center retrospective cohort study. Ulus Travma Ve Acil Cerrahi Derg-Turk J Trauma Emerg Surg 28:900–910. https://doi.org/10.14744/tjtes.2021.89287
Ceresoli M, Coccolini F, Magnone S et al (2021) The decrease of non-complicated acute appendicitis and the negative appendectomy rate during pandemic. Eur J Trauma Emerg Surg 47:1359–1365. https://doi.org/10.1007/s00068-021-01663-7
Dreifuss NH, Schlottmann F, Sadava EE, Rotholtz NA (2020) Acute appendicitis does not quarantine: surgical outcomes of laparoscopic appendectomy in COVID-19 times. Br J Surg 107:e368–e369. https://doi.org/10.1002/bjs.11806
Drysdale H, Ooi S, Nagra S et al (2020) Clinical activity and outcomes during Geelong’s general surgery response to the coronavirus disease 2019 pandemic. ANZ J Surg 90:1573–1579. https://doi.org/10.1111/ans.16207
Ergun E, Sozduyar S, Gurbanova A et al (2021) An indirect effect of COVID-19 pandemic: increased pediatric perforated appendicitis rate due to delayed admission. Turk J Surg 37:318–323. https://doi.org/10.47717/turkjsurg.2021.5277
Ernudd I, Alga A, Sandblom G et al (2022) Treatment strategies and perforation rate of acute appendicitis during the early phase of the Covid-19 pandemic: a Swedish cohort study. J Surg Res 280:450–458. https://doi.org/10.1016/j.jss.2022.07.007
Esparaz J, Chen M, Beierle E et al (2021) Perforated appendicitis during a pandemic: the downstream effect of COVID-19 in children. J Surg Res 268:263–266. https://doi.org/10.1016/j.jss.2021.07.008
Fonseca M, Trindade E, Costa O et al (2020) Impact of COVID-19 outbreak on the emergency presentation of acute appendicitis. Am Surg 86:1508–1512. https://doi.org/10.1177/0003134820972098
Ginchereau JB, Bellavance M-A, Hamel A et al (2022) Impact of the SARS-COV2 on surgical treatment of acute appendicitis: a retrospective cohort multi-centre study. J Surg Res 5:275–283
Guadalajara H, de Nova J, Yiasemidou M et al (2021) The SARS-CoV-2 first wave impact in the acute inflammatory surgical pathologies. Sci Rep. https://doi.org/10.1038/s41598-021-98878-w
Göksoy B, Akça MT, İnanç ÖF (2020) The impacts of the covid-19 outbreak on emergency department visits of surgical patients. Ulus Travma Ve Acil Cerrahi Derg 26:685–692. https://doi.org/10.14744/tjtes.2020.67927
Hrishikesh S, Aladeojebi A, Murcott D et al (2021) Emergency appendicectomy during COVID-19 pandemic-a single UK centre experience. Pol J Surg 93:32–38. https://doi.org/10.5604/01.3001.0014.8090
Huijgen D, De Wijkerslooth E, Janssen J et al (2022) Multicenter cohort study on the presentation and treatment of acute appendicitis during the COVID-19 pandemic. Int J Colorectal Dis 37:1087–1095. https://doi.org/10.1007/s00384-022-04137-3
Hutchings A, Moonesinghe R, Zapata S et al (2022) Impact of the first wave of COVID-19 on outcomes following emergency admissions for common acute surgical conditions: analysis of a national database in England. Br J Surg 109:984–994. https://doi.org/10.1093/bjs/znac233
Jantzen A, Bang-Nielsen A, Bertelsen C et al (2022) Incidence of appendicitis during COVID-19 lockdown: a nationwide population-based study. Scand J Surg. https://doi.org/10.1177/14574969221089387
La Pergola E, Sgro A, Rebosio F et al (2020) Appendicitis in children in a large Italian COVID-19 pandemic area. Front Pediatr. https://doi.org/10.3389/fped.2020.600320
Lee-Archer P, Blackall S, Campbell H et al (2020) Increased incidence of complicated appendicitis during the COVID-19 pandemic. J Paediatr Child Health 56:1313–1314. https://doi.org/10.1111/jpc.15058
Li C, Saleh A (2022) Effect of COVID-19 on pediatric appendicitis presentations and complications. J Pediatr Surg 57:861–865. https://doi.org/10.1016/j.jpedsurg.2021.12.047
McGuinness M, Hsee L (2020) Impact of theCOVID-19 national lockdown on emergency general surgery: Auckland City Hospital’s experience. ANZ J Surg 90:2254–2258. https://doi.org/10.1111/ans.16336
Meyer T (2021) Impact of the COVID-19 pandemic on appendicitis in COVID-19 negative children. Monatsschr Kinderheilkd 169:633–638. https://doi.org/10.1007/s00112-021-01161-5
Nassiri A, Pruden R, Holan C et al (2022) Pediatric appendicitis in the time of the COVID-19 pandemic: a retrospective chart review. J Am Coll Emerg Physicians Open. https://doi.org/10.1002/emp2.12722
Orthopoulos G, Santone E, Izzo F et al (2021) Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am J Surg 221:1056–1060. https://doi.org/10.1016/j.amjsurg.2020.09.026
Pellicciaro M, Vanni G, Grande S et al (2022) Acute appendicitis during coronavirus disease 2019 (COVID-19): increasing incidence of complicate appendicitis, severity and length of hospitalization. In Vivo 36:1325–1332. https://doi.org/10.21873/invivo.12833
Percul C, Cruz M, Meza A et al (2021) Impact of the COVID-19 pandemic on the pediatric population with acute appendicitis: experience at a general, tertiary care hospital. Arch Argent Pediatr 119:224–229. https://doi.org/10.5546/aap.2021.eng.224
Perea del Pozo E, Aparicio-Sánchez D, Hinojosa Ramírez F et al (2020) A prospective cohort study of the impact of Covid19 world pandemic on the management of emergency surgical pathology. Br J Surg 107:e463–e464. https://doi.org/10.1002/bjs.11918
Raffaele A, Cervone A, Ruffoli M et al (2020) Critical factors conditioning the management of appendicitis in children during COVID-19 pandemic: experience from the outbreak area of Lombardy, Italy. Br J Surg 107:E529–E530. https://doi.org/10.1002/bjs.12004
Riveros S, Artigas G, Inzunza M et al (2021) Double prevalence of appendicular peritonitis during COVID times. Br J Surg 108:E133–E134. https://doi.org/10.1093/BJS/ZNAA169
Roberts K, ANZSCRAFT Collaborative (2022) Impact of COVID-19 on appendicitis presentations in children in Australia and New Zealand. ANZ J Surg 92:736–741. https://doi.org/10.1111/ans.17566
Rudnicki Y, Soback H, Mekiten O et al (2022) The impact of COVID-19 pandemic lockdown on the incidence and outcome of complicated appendicitis. Surg Endosc Interv Tech 36:3460–3466. https://doi.org/10.1007/s00464-021-08667-9
Sartori A, Podda M, Botteri E et al (2021) Appendectomy during the COVID-19 pandemic in Italy: a multicenter ambispective cohort study by the Italian society of endoscopic surgery and new technologies (the CRAC study). Updat Surg 73:2205–2213. https://doi.org/10.1007/s13304-021-01126-z
Sukmanee J, Butchon R, Sarajan MH et al (2022) Estimating the potential overdiagnosis and overtreatment of acute appendicitis in Thailand using a secondary data analysis of service utilization before, during and after the COVID-19 lockdown policy. PLoS ONE. https://doi.org/10.1371/journal.pone.0270241
Surek A, Ferahman S, Gemici E et al (2021) Effects of COVID-19 pandemic on general surgical emergencies: are some emergencies really urgent? Level 1 trauma center experience. Eur J Trauma Emerg Surg 47:647–652. https://doi.org/10.1007/s00068-020-01534-7
Theodorou C, Beres A, Nguyen M et al (2021) Statewide impact of the COVID pandemic on pediatric appendicitis in California: a multicenter study. J Surg Res 267:132–142. https://doi.org/10.1016/j.jss.2021.05.023
Turhan N, Arican C (2022) The effects of COVID-19 pandemic on patients with acute appendicitis. Ulus Travma Ve Acil Cerrahi Derg-Turk J Trauma Emerg Surg 28:756–761. https://doi.org/10.14744/tjtes.2021.53929
Wang A, Prieto J, Ikeda D et al (2021) Perforated appendicitis: an unintended consequence during the Coronavirus-19 pandemic. Mil Med 186:E94–E97. https://doi.org/10.1093/milmed/usaa527
Wang F, Wu J, Lin Y et al (2022) Coronavirus disease pandemic effect on medical-seeking behaviors even in one resource-competent community: a case controlled study. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph191710822
Yang Y, Li Y, Du X (2021) Acute complex appendicitis during the COVID-19 epidemic: a single-institution retrospective analysis based on real-world data. Am J Emerg Med 46:74–77. https://doi.org/10.1016/j.ajem.2021.03.022
Zhang P, Zhang Q, Zhao H (2022) COVID-19 pandemic changed the management and outcomes of acute appendicitis in northern Beijing: a single-center study. World J Clin Cases 10:820–829. https://doi.org/10.12998/wjcc.v10.i3.820
Zhou Y, Cen L (2020) Managing acute appendicitis during the COVID-19 pandemic in Jiaxing, China. World J Clin Cases 8:4349–4359. https://doi.org/10.12998/wjcc.v8.i19.4349
Funding
Open access funding provided by Linköping University. We have not received any funding specifically for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Andersson, R.E., Agiorgiti, M. & Bendtsen, M. Spontaneous Resolution of Uncomplicated Appendicitis may Explain Increase in Proportion of Complicated Appendicitis During Covid-19 Pandemic: a Systematic Review and Meta-analysis. World J Surg 47, 1901–1916 (2023). https://doi.org/10.1007/s00268-023-07027-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-023-07027-z