Abstract
Background
A time interval between diagnosis and surgery for gastric cancer is necessary, although its impact on survival remains controversial. We evaluated the impact of preoperative time interval on survival in gastric cancer patients.
Methods
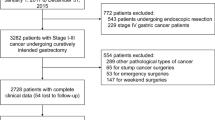
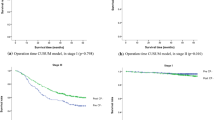
We enrolled 332 patients who underwent curative gastrectomy for clinical stage (cStage) I–III gastric cancer between 2012 and 2015. We separately analyzed early- (cStage I) and advanced-stage (cStages II and III) patients. Early-stage patients were divided according to preoperative time interval: short (≤ 42 days) and long (> 42 days) groups. Advanced-stage patients were also divided into short (≤ 21 days) and long (> 21 days) groups. We compared the survival between the short and long groups in early- and advanced-stage patients.
Results
The median preoperative time interval was 29 days, and no significant differences were found in patient characteristics between the short and long groups in early- and advanced-stage patients. In early-stage patients, the 5-year survival rates of the short and long groups were 86.5% and 88.4%, respectively (P = 0.917). In advanced-stage patients, the 5-year survival rates were 72.1% and 70.0%, respectively (P = 0.552). In multivariate analysis, a longer time interval was not selected as an independent prognostic factor in early- and advanced-stage patients.
Conclusions
In this study, survival difference was not found based upon preoperative time interval. The results do not affirm the delay of treatment without reason, however, imperative extension of preoperative time interval may be justified from the standpoint of long-term survival.



Similar content being viewed by others
References
Gray RE, Fitch MI, Phillips C et al (1999) Presurgery experiences of prostate cancer patients and their spouses. Cancer Pract 7(3):130–135
Robinson KM, Christensen KB, Ottesen B et al (2012) Diagnostic delay, quality of life and patient satisfaction among women diagnosed with endometrial or ovarian cancer: a nationwide Danish study. Qual Life Res 21(9):1519–1525
Brenkman HJF, Visser E, van Rossum PSN et al (2017) Association between waiting time from diagnosis to treatment and survival in patients with curable gastric cancer: a population-based study in the Netherlands. Ann Surg Oncol 24(7):1761–1769
Hudson AR (2006) Ontario wait time strategy. Can J Urol 13(Suppl 3):14–15
Fradet Y, Aprikian A, Dranitsaris G et al (2006) Does prolonging the time to bladder cancer surgery affect long-term cancer control: a systematic review of the literature. Can J Urol 13(Suppl 3):37–47
Bourgade V, Drouin SJ, Yates DR et al (2014) Impact of the length of time between diagnosis and surgical removal of urologic neoplasms on survival. World J Urol 32(2):475–479
Eriksson L, Bergh J, Humphreys K et al (2018) Time from breast cancer diagnosis to therapeutic surgery and breast cancer prognosis: a population-based cohort study. Int J Cancer 143(5):1093–1104
Bleicher RJ, Ruth K, Sigurdson ER et al (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339
Furukawa K, Irino T, Makuuchi R et al (2019) Impact of preoperative wait time on survival in patients with clinical stage II/III gastric cancer. Gastric Cancer 22(4):864–872
TNM Classification of Malignant Tumors, 7th edn.
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma: 3rd edn. Gastric Cancer 14(2):101–112
Japanese Gastric Cancer Association (2017) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20(1):1–19
Sasako M, Sakuramoto S, Katai H et al (2011) Five-year outcomes of a randomized phase III trial comparing adjuvant chemotherapy with S-1 versus surgery alone in stage II or III gastric cancer. J Clin Oncol 29(33):4387–4393
Sakuramoto S, Sasako M, Yamaguchi T et al (2007) Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med 357(18):1810–1820
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48(3):452–458
Yun YH, Kim YA, Min YH et al (2012) The influence of hospital volume and surgical treatment delay on long-term survival after cancer surgery. Ann Oncol 23(10):2731–2737
Shin DW, Cho J, Kim SY et al (2013) Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol 20(8):2468–2476
Mirkin KA, Hollenbeak CS, Wong J (2018) Time to surgery: a misguided quality metric in early stage pancreatic cancer. J Gastrointest Surg 22(8):1365–1375
Saad F, Finelli A, Dranitsaris G et al (2006) Does prolonging the time to prostate cancer surgery impact long-term cancer control: a systematic review of the literature. Can J Urol 13(Suppl 3):16–24
Visser E, Leeftink AG, van Rossum PS et al (2016) Waiting time from diagnosis to treatment has no impact on survival in patients with esophageal cancer. Ann Surg Oncol 23(8):2679–2689
Kumazu Y, Oba K, Hayashi T et al (2020) Relationship between the waiting times for surgery and survival in patients with gastric cancer. World J Surg 44(4):1209–1215
Kötz BS, Croft S, Ferry DR (2006) Do delays between diagnosis and surgery in resectable esophageal cancer affect survival? A study based on West Midlands cancer registration data. Br J Cancer 95(7):835–840
Matsuo K, Opper NR, Ciccone MA et al (2015) Time interval between endometrial biopsy and surgical staging for type I endometrial cancer: association between tumor characteristics and survival outcome. Obstet Gynecol 125(2):424–433
Crawford SC, Davis JA, Siddiqui NA et al (2002) The waiting time paradox: population based retrospective study of treatment delay and survival of women with endometrial cancer in Scotland. BMJ 325(7357):196
Funding
The authors have not received grant support or other forms of assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declared that there is no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
This study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of Tokyo Medical and Dental University (M2020-279).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Okuno, K., Tokunaga, M., Yamashita, Y. et al. Impact of Preoperative Time Interval on Survival in Patients With Gastric Cancer. World J Surg 45, 2860–2867 (2021). https://doi.org/10.1007/s00268-021-06187-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06187-0