Abstract
Background
Esophageal cancer occupies a vital position in fatal cancer-related disease, with esophagectomy procedures helping to improve patient survival. The timing when oral intake should be resumed after esophagectomy and whether early oral feeding (EOF) or delayed oral feeding (DOF) should be the optimal regimen are controversial.
Methods
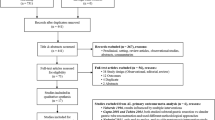
Databases (PubMed, Embase, Cochrane library) were searched. All records were screened by two authors through full-text reading. Data on the anastomotic leakage rate were extracted and synthesized in meta-analyses. Postoperative pneumonia rate and length of hospital stay were also assessed.
Results
Seven studies from 49 records were included after full-text reading; 1595 patients were totally included in the analysis. No significant difference was observed between the EOF and DOF groups (odds ratio [OR] 1.68; 95% confidence interval [CI] 0.70–4.03; p = 0.2495; I2 = 70%). Higher anastomotic leakage rate was observed in EOF compared with DOF (OR 2.89; 95% CI 1.56–5.34; p = 0.0007; I2 = 10%) in the open subgroup. No significant difference was observed in the MIE (OR 0.48; 95% CI 0.22–1.02; p = 0.0564; I2 = 0%). Patients performed similarly in pneumonia (OR 1.12; 95% CI 0.57–2.21; p = 0.745; I2 = 34%). In cervical subgroup, anastomosis leakage may be less in DOF (OR 2.42 95% CI 1.26–4.64; p = 0.0651; I2 = 58%), while in thoracic subgroup, there is no obvious difference (OR 0.86 95% CI 0.46–1.61; p = 0.01; I2 = 84.9%).
Conclusions
Anastomotic leakage related to the timing of oral feeding after open esophagectomy, which is more favorable to the DOF regimen. However, timing of oral feeding did not impair anastomotic healing in patients undergoing MIE.





Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Cooke DT, Lin GC, Lau CL et al (2009) Analysis of cervical esophagogastric anastomotic leaks after transhiatal esophagectomy: risk factors, presentation, and detection. Ann Thorac Surg 88:177–185
Etxaniz SL, Reyna JG, Orue JLE et al (2013) Cervical anastomotic leak after esophagectomy: diagnosis and management. Cirugia Espanola 91:31–37
Orringer MB, Marshall B, Chang AC et al (2007) Two thousand transhiatal Esophagectomies—changing trends, lessons learned. Ann Surg 246:363–374
Price TN, Nichols FC, Harmsen WS et al (2013) A comprehensive review of anastomotic technique in 432 esophagectomies. Ann Thorac Surg 95:1154–1161
O’Keefe SJD (2009) A guide to enteral access procedures and enteral nutrition. Nat Rev Gastroenterol Hepatol 6:207–215
Bauer JD, Capra S (2005) Nutrition intervention improves outcomes in patients with cancer cachexia receiving chemotherapy—a pilot study. Support Care Cancer 13:270–274
Hur H, Kim SG, Shim JH et al (2011) Effect of early oral feeding after gastric cancer surgery: a result of randomized clinical trial. Surgery 149:561–568
El Nakeeb A, Fikry A, El Metwally T et al (2009) Early oral feeding in patients undergoing elective colonic anastomosis. Int J Surg 7:206–209
Hur H, Si Y, Kang WK et al (2009) Effects of early oral feeding on surgical outcomes and recovery after curative surgery for gastric cancer: pilot study results. World J Surg 33:1454–1458. https://doi.org/10.1007/s00268-009-0009-3
Weijs TJ, Berkelmans GH, Nieuwenhuijzen GA et al (2016) Immediate postoperative oral nutrition following esophagectomy: a multicenter clinical trial. Ann Thorac Surg 102:1141–1148
Bailey L, Khan O, Willows E et al (2013) Open and laparoscopically assisted oesophagectomy: a prospective comparative study. Eur J Cardiothorac Surg 43:268–273
Nafteux P, Moons J, Coosemans W et al (2011) Minimally invasive oesophagectomy: a valuable alternative to open oesophagectomy for the treatment of early oesophageal and gastro-oesophageal junction carcinoma. Eur J Cardiothorac Surg 40:1455–1464
Sihag S, Wright CD, Wain JC et al (2012) Comparison of perioperative outcomes following open versus minimally invasive Ivor Lewis oesophagectomy at a single, high-volume centre. Eur J Cardiothorac Surg 42:430–437
Sun HB, Li Y, Liu XB et al (2018) Early oral feeding following McKeown minimally invasive esophagectomy: an open-label, randomized, controlled, noninferiority trial. Ann Surg 267:435–442
Berkelmans GHK, Fransen L, Weijs TJ et al (2018) The long-term effects of early oral feeding following minimal invasive esophagectomy. Dis Esophagus 31:1–8
Bolton JS, Conway WC, Abbas AE (2014) Planned delay of oral intake after esophagectomy reduces the cervical anastomotic leak rate and hospital length of stay. J Gastrointest Surg 18:304–309
Eberhard KE, Achiam MP, Rolff HC et al (2017) Comparison of “Nil by Mouth” versus early oral intake in three different diet regimens following esophagectomy. World J Surg 41:1575–1583. https://doi.org/10.1007/s00268-017-3870-5
Sun HB, Liu XB, Zhang RX et al (2015) Early oral feeding following thoracolaparoscopic oesophagectomy for oesophageal cancer. Eur J Cardiothorac Surg 47:227–233
Weijs TJ, Berkelmans GH, Nieuwenhuijzen GA et al (2015) Routes for early enteral nutrition after esophagectomy. A systematic review. Clin Nutr 34:1–6
Speicher JE, Gunn TM, Rossi NP, Iannettoni MD (2018) Delay in oral feeding is associated with a decrease in anastomotic leak following transhiatal esophagectomy. Semin Thorac Cardiovasc Surg 30:476–484
Tomaszek SC, Cassivi SD, Allen MS et al (2010) An alternative postoperative pathway reduces length of hospitalisation following oesophagectomy. Eur J Cardiothorac Surg 37:807–813
Lassen K, Kjaeve J, Fetveit T et al (2008) Allowing normal food at will after major upper gastrointestinal surgery does not increase morbidity: a randomized multicenter trial. Ann Surg 247:721–729
Jo DH, Jeong O, Sun JW et al (2011) Feasibility study of early oral intake after gastrectomy for gastric carcinoma. J Gastric Cancer 11:101–108
Shoar S, Naderan M, Mahmoodzadeh H et al (2016) Early oral feeding after surgery for upper gastrointestinal malignancies: a prospective cohort study. Oman Med J 31:182–187
Yamashita K, Watanabe M, Mine S et al (2018) Minimally invasive esophagectomy attenuates the postoperative inflammatory response and improves survival compared with open esophagectomy in patients with esophageal cancer: a propensity score matched analysis. Surg Endosc 32:4443–4450
Zingg U, McQuinn A, DiValentino D et al (2009) Minimally invasive versus open esophagectomy for patients with esophageal cancer. Ann Thorac Surg 87:911–919
Palanivelu C, Prakash A, Senthilkumar R et al (2006) Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position–experience of 130 patients. J Am Coll Surg 203:7–16
Martin JT, Federico JA, McKelvey AA, et al. Prevention of delayed gastric emptying after esophagectomy: a single center’s experience with botulinum toxin. Ann Thorac Surg 2009; 87:1708-13; discussion 1713–4
Lee HS, Kim MS, Lee JM et al (2005) Intrathoracic gastric emptying of solid food after esophagectomy for esophageal cancer. Ann Thorac Surg 80:443–447
Weijs TJ, Berkelmans GHK, Nieuwenhuijzen GAP et al (2015) Routes for early enteral nutrition after esophagectomy. A systematic review. Clinical Nutrition 34:1–6
Studer P, Raber G, Ott D et al (2016) Risk factors for fatal outcome in surgical patients with postoperative aspiration pneumonia. Int J Surg 27:21–25
Li Y, Sun HB, Liu XB et al (2016) Early oral feeding following mckeown minimally invasive esophagectomy: a randomized controlled study. Dis Esophagus 29:16A
Martin RE, Letsos P, Taves DH et al (2001) Oropharyngeal dysphagia in esophageal cancer before and after transhiatal esophagectomy. Dysphagia 16:23–31
Wang YJ, Liu XH, Mei LY et al (2016) Do alterations in plasma albumin and prealbumin after minimally invasive esophagectomy for squamous cell carcinoma influence the incidence of cervical anastomotic leak? Surg Endosc 30:3943–3949
Inoue T, Ito S, Ando M et al (2016) Changes in exercise capacity, muscle strength, and health-related quality of life in esophageal cancer patients undergoing esophagectomy. BMC Sports Sci Med Rehabil 8:34
Funding
This work was supported by the National Key R&D Program of China (No. 2018YFC0910700), Beijing Municipal Science & Technology Commission (No. Z161100000516063), Beijing Human Resources and Social Security Bureau (Beijing Millions of Talents Project, 2018A05), Beijing Municipal Administration of Hospitals' Youth Programme (QMS20191107), National Natural Science Foundation of China (No. 81972842), Beijing Natural Science Foundation (No. 7192036).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, X., Yan, S., Ma, Y. et al. Impact of Early Oral Feeding on Anastomotic Leakage Rate After Esophagectomy: A Systematic Review and Meta-analysis. World J Surg 44, 2709–2718 (2020). https://doi.org/10.1007/s00268-020-05489-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05489-z