Abstract
Background
The requirement for elective cholecystectomy in older patients is unclear. To determine predictors for requiring elective cholecystectomy in older patients, a prospective cohort study was performed.
Methods
All patients with gallstone disease who presented to our department from 2006 to 2018 were included if they met the following criteria: (1) age 75 years or older, (2) presentation for elective cholecystectomy, and (3) preoperative diagnosis of cholecystolithiasis. Two therapeutic options, elective surgery and a wait-and-see approach, were offered at their initial visit. Enrolled patients were assigned to one arm of the study according to their choice of the therapeutic options. The primary endpoint was the incidence of gallstone-related complications. The endpoint was compared between patients who underwent cholecystectomy (CH group) and those who chose a wait-and-see approach (No-CH group).
Results
During the study period, there were 344 patients in the CH group and 161 in the No-CH group. Among patients with a history of bile duct stones, the incidence of gallstone-related complications in the No-CH group was significantly higher (45% within 3 years, including two gallstone-related deaths) than that in the CH group (RR 2.66, 95% confidence interval 1.50–4.77, p = 0.0009). Among patients with no history of bile duct stones, the incidence of gallstone-related complications in the No-CH group reached only 10% over the 12 years.
Conclusion
Cholecystectomy is recommended for older patients with both histories of cholecystolithiasis and bile duct stones, whereas a wait-and-see approach is preferable for patients with no bile duct stone history. A history of bile duct stones is a good predictor for cholecystectomy in older patients.
Similar content being viewed by others
Introduction
Recent rapid increases in the aging population have created an impending “silver tsunami” in developed countries. Indications for surgical treatments in this population are a serious issue because most older patients have multiple concomitant systemic diseases. The incidence of gallstone disease is especially high among the older population, and the indications for treatment, including surgical procedures, are complicated. Gallstone disease is one of the most common and costly digestive diseases associated with aging. The current standard of care for patients presenting with cholecystolithiasis is early elective cholecystectomy to reduce gallstone-related complications (G-RCs) and medical costs. Although laparoscopic cholecystectomy is the best modality for gallstone disease, its safety in geriatric patients remains controversial because of multiple competing risks [1, 2].
Age is an independent predictor of poorer outcomes after cholecystectomy [3, 4]. Associated chronic illness increases the morbidity and mortality of elective cholecystectomy. Many older patients may have a limited life expectancy because of comorbidities and may succumb to chronic medical conditions, such as heart disease, before developing symptoms of gallstone disease. Older patients also have an increased risk of developing G-RCs [5,6,7,8,9,10]. Unless the expected life span is short, cholecystolithiasis and subsequent choledocholithiasis are likely to recur. Indeed, a meta-analysis that compared cholecystectomy after endoscopic sphincterotomy (EST) versus a wait-and-see approach showed a significantly higher risk of biliary complications and death in the latter group [11]. Once biliary complications occur, treatment-related morbidity and mortality rates significantly increase in this vulnerable population. However, management of older patients who present with symptomatic cholecystolithiasis has not been well described. Surgeons have recently become more aggressive in treating gallstone disease, especially in older patients. Despite this trend, many patients continue to be treated non-operatively [12, 13].
Because the selection criteria for non-operative management may have changed, the effect of this approach needs to be reinvestigated. This study aimed to compare the outcomes of cholecystectomy versus a wait-and-see approach in patients aged ≥75 years with cholecystolithiasis. We also examined predictors of the requirement for elective cholecystectomy after an episode of symptomatic cholecystolithiasis in this older population.
Patients and methods
This prospective cohort study was performed to examine predictors of whether elective cholecystectomy is indicated following an episode of symptomatic cholecystolithiasis in older patients. All consecutive patients with gallstone disease who presented for cholecystectomy at the Department of Surgery of Kansai Medical University, Hirakata Hospital from January 2006 to December 2018 were included if they met the following criteria: (1) age ≥75 years, (2) presentation for elective cholecystectomy, and (3) preoperative diagnosis of cholecystolithiasis. Exclusion criteria were as follows: (1) presentation for emergency surgery, (2) ongoing symptomatic cholecystolithiasis, (3) silent gallstones with no history of associated symptoms, and (4) preoperative diagnosis of concomitant gallbladder malignancy.
In our institution, magnetic resonance cholangiography is routinely performed for patients with gallstone diseases. Per our institutional policy, if bile duct stones (BDSs) are found, these patients are supposed to be treated by gastroenterologists using an EST procedure, not with surgery. Therefore, most of the patients with BDSs were treated by gastroenterologists including an emergency EST before presentation to the surgical department.
Two therapeutic options, elective surgery and a wait-and-see approach, were offered at the initial visit of all patients who presented to our department for elective cholecystectomy. Enrolled patients were assigned to one arm of the study according to their choice of therapeutic option. If patients selected surgical treatment, laparoscopic cholecystectomy was planned within 2 months; patients were observed postoperatively at least once per year. Patients who chose the wait-and-see approach were also observed yearly. The primary endpoint was the incidence of G-RCs, and the secondary endpoint was overall survival. The definition of G-RCs was as follows: choledocholithiasis; cholangitis; obstructive jaundice resulting from BDS; pancreatitis resulting from BDS; and cholecystitis in patients who chose a wait-and-see approach. These complications were defined as those requiring admission. Outcomes were evaluated until death or at the end of the observation period. Additionally, information was obtained on patients’ characteristics, treatment modality for recurrence, and cause of death. Follow-up was performed by reviewing the medical records and conducting telephone interviews with patients, their families, or home doctors.
Informed consent was obtained from all patients for their being included in the study. All procedures followed were in accordance with the ethical standards of the institutional committee on human experimentation and with the Helsinki Declaration. This study received IRB approval from our institution (Protocol Number, 2016697).
Statistics
Statistical data analyses were performed with JMP version 10.0.2 (SAS Institute Inc., Cary, NC, USA). A continuous variable was analyzed with the Student’s t test. Categorical variables were analyzed with the chi-square test or Fisher’s exact test. Multivariate logistic regression analysis was performed to identify significant factors for predicting complications. The cumulative incidence of G-RCs and overall survival were calculated with the Kaplan–Meier method and compared between groups with the log-rank test. Risk ratios (RRs) and 95% confidence intervals (CIs) were calculated with a proportional hazards model. Statistical significance was set at p values <0.05.
Results
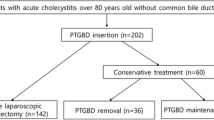
A flowchart of the current study is shown in Fig. 1. During 13 years from January 2006 to December 2018, 2736 consecutive patients presented to our institution with benign gallbladder disease. Of these 2736 patients, 2307 underwent laparoscopic cholecystectomy and 268 underwent open cholecystectomy. Among all 2736 patients, 505 met the inclusion and exclusion criteria, among whom 344 underwent cholecystectomy and 161 chose a wait-and-see approach. During the observation period, 19 patients who underwent cholecystectomy and four who chose a wait-and-see approach withdrew from follow-up. The remaining 325 patients who underwent cholecystectomy (CH group) and 157 who chose a wait-and-see policy (No-CH group) were compared. The follow-up rate was 94.5% in the CH group and 97.5% in the No-CH group.
The patients’ clinical background information is shown in Table 1. Age, performance status, and American Society of Anesthesiologists (ASA) classification scores in the No-CH group were significantly higher than those in the CH group. There were no significant differences in sex and a history of BDS between the groups. All patients with a history of BDS had undergone endoscopic retrograde cholangiography and EST to remove BDS before presentation to our department for cholecystectomy.
A total of 35 G-RCs occurred in 23 of 325 (7.1%) patients in the CH group, and 49 G-RCs occurred in 30 of 157 (19.1%) patients in the No-CH group (Table 2). Endoscopic retrograde cholangiography was performed 34 times in the CH group and 33 times in the No-CH group for recurrence or development of BDS. During the observation period, 14 patients in the No-CH group required cholecystectomy, including five urgent and nine elective surgeries. The five urgent surgeries were performed for acute cholecystitis. The remaining nine elective surgeries were performed because patients chose to undergo cholecystectomy to avoid repeated endoscopic retrograde cholangiography for recurrent BDS, a recurrent gallstone attack, or cholecystitis. Rate of urgent treatments including endoscopic and surgical procedures for the G-RCs was significantly higher in the No-CH group (19.7%) than in the CH group (4.3%) (p < 0.0001) (Table 2).
Most of the causes of death in both groups were non-specific and consistent with those common in the aging population (Table 2). However, two gallstone-related deaths occurred in the No-CH group, whereas no gallstone-related deaths occurred in the CH group. One case of gallstone-related mortality was an 84-year-old woman who died of severe acute pancreatitis resulting from BDS. The second case of mortality was an 87-year-old woman who died of sepsis resulting from acute gangrenous cholecystitis. Both patients had a history of BDS as indicated by asterisks in Figs. 2, 3 and 4.
Cumulative incidence of gallstone-related complications in patients who underwent cholecystectomy (black) and those who did not undergo cholecystectomy (gray). Asterisks (*) indicate gallstone-related deaths. One death resulted from acute gangrenous cholecystitis, and the second was from severe acute pancreatitis
Gallstone-related complications in subgroup analysis according to a history of bile duct stones. Solid gray line: patients without cholecystectomy with bile duct stones. Solid black line: patients with cholecystectomy with bile duct stones. Dotted gray line: patients without cholecystectomy without bile duct stones. Dotted black line: patients with cholecystectomy without bile duct stones. *, patients died of gallstone-related complications
Multivariate analysis of the predictors of G-RCs and overall survival are shown in Table 3. Cholecystectomy significantly reduced the incidence of G-RCs (p < 0.0012). In contrast, a history of BDS was significantly associated with an increased incidence of G-RCs (p < 0.0001). With regard to overall survival, age and ASA classification were significant variables (p = 0.016 and p < 0.0001, respectively), whereas cholecystectomy was not.
Kaplan–Meier analysis was performed to compare overall survival between the groups (Fig. 2). Although overall survival in the No-CH group tended to be lower than that in the CH group, this difference was not significant (RR 1.46, 95% CI 0.93–2.28; p = 0.10). During the observation period, 33 of 157 (21.0%) patients died in the No-CH group, including two gallstone-related deaths, and 46 of 325 (14.2%) patients died in the CH group.
Figure 3 shows that the cumulative incidence of G-RCs was significantly higher in the No-CH group than in the CH group (RR 2.88, 95% CI 1.70–4.93; p < 0.0001). In the No-CH group, the incidence of G-RCs, including the two gallstone-related deaths, reached 26% within 4 years, whereas this incidence reached 12% within 8 years in the CH group.
Because most of the G-RCs in both groups were BDS (Table 2), subgroup analysis was performed according to the presence or absence of a history of BDS. The results of subgroup analysis are shown in Fig. 4. Patients in the No-CH group with a history of BDS (BDS subgroup) had a 45% incidence of G-RCs within 3 years, whereas this incidence in this subgroup reached 30% within 8 years in the CH group. Among patients in the BDS subgroup, the RR for the occurrence of G-RCs in the No-CH group compared with the CH group was 2.66 (95% CI 1.50–4.77; p = 0.0009). Additionally, two gallstone-related deaths occurred in the BDS subgroup of the No-CH group. In contrast, among patients with no history of BDS (No-BDS subgroup), the incidence of G-RCs in the No-CH group reached only 10% within 12 years, while that in the CH group was only 2% within 12 years.
During the observation period, the rate of BDS among gallstone patients was increasing according to age, and it reached 47.5% among the gallstone patients aged 80 years or older (Figs. 5 and 6). Therefore, the rate of BDS in this study population was relatively high, and the average of the rate of BDS was 44.6% (215/482) at the time of their presentation (Table 1).
Discussion
Because the management of older patients who present with symptomatic cholecystolithiasis has not been well described, the decision to pursue elective cholecystectomy in this population is complicated [2]. Some of these patients choose non-operative management, while others undergo elective surgery. The reason for pursuing non-operative management may be a surgeon’s reticence to operate on very old patients, the patient’s preference, or the presence of comorbidities or complicated disease [5, 14,15,16]. Increased comorbidity, which for older patients may increase the risk of early death, is a protective factor for subsequent biliary complications. While this finding appears counterintuitive, the number of comorbidities in this vulnerable cohort of older patients likely limits their life expectancy. Many patients with multiple comorbidities may die from chronic medical conditions, such as heart disease and/or malignancies, before they develop symptoms of gallstone disease [2]. We estimated the effect of operative versus non-operative management in older patients with cholecystolithiasis and analyzed which patients experienced recurrence following operative versus non-operative treatment.
Although cholecystectomy is the standard of care for patients presenting with symptomatic cholecystolithiasis, approximately one-third of older patients with cholecystolithiasis in this study did not undergo elective cholecystectomy. Among these patients, 80% did not ultimately experience late biliary complications requiring surgery and/or hospitalization during the 13-year observation period. However, the remaining 20% of patients required repeated interventional treatments for choledocholithiasis and/or cholecystectomy. This incidence of 20% for biliary events over the 12-year period means a difficult decision for whether operative treatment or non-operative management is preferable for patients aged ≥75 years.
Because the presence of gallstones is a risk factor for recurrent biliary complications, subsequent cholecystectomy is approved as accepted management to prevent delayed biliary complications in patients with residual gallstones after endoscopic removal of BDS with EST [17, 18]. Two randomized studies reported that subsequent cholecystectomy reduced recurrent biliary events and should be recommended [19, 20]. Although these trials did not focus on older patients, cholecystectomy after EST resulted in superior outcomes compared with a wait-and-see policy. Many of the patients in the wait-and-see group developed recurrent biliary events, necessitating subsequent cholecystectomy in most cases. Cholecystectomy is commonly performed after endoscopic treatment, and it is assumed to be the standard medical care [21].
In the current study, the rate of BDS history among gallstone patients was relatively high compared with the rate of BDS in the general population. We recently reported that the rate of BDS among gallstone patients was increasing according to age in an aging society, and it reached over 40% among gallstone patients aged 80 years or older [10]. In this study, all patients were 75 years or older, which is the reason why the rate of BDS is high in this study. The prevalence of choledocholithiasis, which increases with age and approached 50% among octogenarians with gallstone disease at our institution, is shown in Figs. 5 and 6.
Our results indicated that G-RC recurrence was mainly attributable to the presence or absence of a history of BDS. Patients with retained gallstones in the BDS subgroup showed a high incidence of late G-RCs, most of which were recurrent BDS. All recurrent biliary complications in the CH group were recurrent BDS; 80% of biliary complications in the No-CH group were recurrence or development of BDS. Therefore, we performed subgroup analysis to estimate the rate of recurrent biliary events according to the BDS history. This analysis showed that, in the No-CH group, recurrent biliary complications in the BDS subgroup reached 45% within only 3 years, including two gallstone-related deaths. Therefore, cholecystectomy appears to be recommended for older patients with a history of BDS. However, even in the CH group, we found a high incidence of recurrent BDS in the BDS subgroup, which reached 30% during the observation period. There are several possible reasons for recurrent BDS after cholecystectomy. BDS may arise de novo within the bile duct. Additionally, EST might contribute to the development of recurrent de novo BDS. Although there is little evidence to confirm the effect of EST on BDS development [22], the finding that all patients in the BDS subgroup had undergone the previous EST treatment in the current study strongly suggests such an influence.
Because adverse events of BDS may be serious and life threatening, BDSs are generally recommended to be removed. Although the incidence of post-EST complications in patients with choledocholithiasis is relatively high, such complications are easily managed with repeated endoscopic procedures. EST may be an option in high-risk patients with comorbidity if the dominating pathology is BDS, although repeated interventions are often necessary [23]. A higher incidence of perioperative complications of cholecystectomy might be expected in older patients because of the high prevalence of concomitant medical disorders, such as cardiopulmonary and cerebrovascular diseases, and the poor general condition of this population. Therefore, conservative management, such as endoscopic procedures, for these patients is an option, especially for patients who are poor candidates for surgery [21].
As shown in the subgroup analysis, patients with no history of BDS (No-BDS subgroup) had an unexpectedly low incidence of recurrent biliary events. Patients in the No-BDS subgroup who underwent cholecystectomy had a recurrence rate of only approximately 2% during 12 years. For patients without a history of BDS who did not undergo cholecystectomy, the recurrence rate was only 10% during this period. Therefore, for older patients with gallstones who have no history of BDS, who have concomitant medical disorders, and who are poor candidates for surgery, individualized management with a wait-and-see approach appears reasonable.
Overall survival in the No-CH group appeared to be lower than that in the CH group, although this was not significant. The main reasons for this finding are the higher mean age and higher ASA classification score in the No-CH group because these patients are likely to choose a wait-and-see approach. The overall survival results in this study indicated that cholecystectomy in older patients at least did not worsen overall survival. Overall survival in the CH group was similar to that in a common aging population. Perioperative mortality in the CH group was mainly caused by malignancy and vascular or respiratory diseases, which was also observed in the No-CH group. These causes of death are also similar to well-known causes of death in an aging society with the exception of two patients who died of G-RCs in the No-CH group.
Multivariate analysis showed that a history of BDS and cholecystectomy is a significant predictive variable for the G-RCs. Although the initial diagnosis was not significantly different between the two groups, the initial diagnosis of cholangitis or pancreatitis tended to increase the risk of G-RCs (OR 2.305, 95% CI 0.961–5.308, p = 0.061) compared with the initial diagnosis of cholecystitis. These diagnoses of cholangitis and pancreatitis might be a confounding factor for G-RC occurrence because all patients whose initial diagnosis was cholangitis or pancreatitis had a history of BDS.
There are some limitations to our study. BDS can be divided into two categories according to the site of stone formation as follows: primary stones, which are formed de novo in the bile duct; and secondary stones, which are formed in the gallbladder and exit into the bile duct. Secondary BDSs include cholesterol gallstones and pigment stones, whereas primary BDSs are typically pigment stones [24]. Therefore, the role of the gallbladder in recurrent BDS is different depending on whether cholesterol stones or pigment stones are the major component. The current study did not assess the type of BDS, and thus, we could not demonstrate the definitive role of the gallbladder in recurrent BDS. Further prospective studies are required to examine the influence of stone type on BDS recurrence.
Conclusion
Cholecystectomy is recommended for older patients with both histories of cholecystolithiasis and BDS, whereas a wait-and-see approach may be better for older patients with a history of cholecystolithiasis without a BDS history. The presence or absence of a history of BDS is an important predictor of the requirement for elective cholecystectomy in patients aged ≥75 years with gallstones.
References
Novello M, Gori D, Saverio SD et al (2018) How safe is performing cholecystectomy in the oldest old? A 15-year retrospective study from a single institution. World J Surg 42:73–81. https://doi.org/10.1007/s00268-017-4147-8
Parmar AD, Sheffield KM, Adhikari D et al (2015) PREOP-gallstones: a prognostic nomogram for the management of symptomatic cholelithiasis in older patients. Ann Surg 261:1184–1190
Nielsen LBJ, Harboe KM, Bardram L (2014) Cholecystectomy for the elderly: no hesitation for otherwise healthy patients. Surg Endosc 28:171–177
Kuy S, Sosa JA, Roman SA et al (2011) Age matters: a study of clinical and economic outcomes following cholecystectomy in elderly Americans. Am J Surg 201:789–796
Arthur JD, Edwards PR, Chagla LS (2003) Management of gallstone disease in the elderly. Ann R Coll Surg Engle 85:91–96
Dubecz A, Langer M, Stadlhuber RJ et al (2012) Cholecystectomy in the very elderly—is 90 the new 70? J Gastrointest Surg 16:282–285
Hazzan D, Geron N, Golijanin D et al (2003) Laparoscopic cholecystectomy in octogenarians. Surg Endosc 17:773–776
Lo CM, Lai EC, Fan ST et al (1996) Laparoscopic cholecystectomy for acute cholecystitis in the elderly. World J Surg 20:983–986. https://doi.org/10.1007/s002689900148
Maxwell JG, Tyler BA, Rutledge R et al (1998) Cholecystectomy in patients aged 80 and older. Am J Surg 176:627–631
Matsui Y, Hirooka S, Yamaki S et al (2019) Assessment of clinical outcome of cholecystectomy according to age in preparation for the “Silver Tsunami”. Am J Surg 218:567–570
McAlister V, Davenport E, Renouf E (2007) Cholecystectomy deferral in patients with endoscopic sphincterotomy. The Cochrane database of systematic reviews CD006233
Trust MD, Sheffield KM, Boyd CA et al (2011) Gallstone pancreatitis in older patients: are we operating enough? Surgery 150:515–525
Bergmann S, Sourial N, Vedel I et al (2011) Gallstone disease in the elderly: are older patients managed differently? Surg Endosc 25:55–61
Siegel JH, Kasmin FE (1997) Biliary tract diseases in the elderly: management and outcomes. Gut 41:433–435
Sugiyama M, Atomi Y (1997) Treatment of acute cholangitis due to choledocholithiasis in elderly and younger patients. Arch Surg 132:1129–1133
Bergman S, Al-Bader M, Sourial N et al (2015) Recurrence of biliary disease following non-operative management in elderly patients. Surg Endosc 29:3485–3490
Williams EJ, Green J, Beckingham I et al (2008) Guidelines on the management of common bile duct stones (CBDS). Gut 57:1004–1021
Mutha P, Shah T, Heuman D et al (2016) Choledocholithiasis without cholelithiasis: should the gallbladder stay or should it go? Dig Dis Sci 61:961–962
Lau JYW, Leow CK, Fung TMK (2006) Cholecystectomy or gallbladder insitu after endoscopic sphincterotomy and bile duct stone removal in Chinese patients. Gastroenterology 130:96–103
Boerma D, Rauws EAJ, Keulemans YCA et al (2002) Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomized trial. Lancet 360:761–765
Fujimoto T, Tsuyuguchi T, Sakai Y et al (2010) Long-term outcome of endoscopic papillotomy for choledocholithiasis with cholecystolithiasis. Dig Endosc 22:95–100
Tanaka M, Takahata S, Konomi H et al (1998) Long-term consequence of endoscopic sphincterotomy for bile duct stones. Gastrointest Endosc 48:465–469
Langerth A, Sandblom G, Karlson BM (2015) Long-term risk for acute pancreatitis, cholangitis, and malignancy more than 15 years after endoscopic sphincterotomy: a population-based study. Endoscopy 47:1132–1136
Kim MH, Yeo SJ, Jung MK et al (2016) The impact of gallbladder status on biliary complications after the endoscopic removal of choledocholithiasis. Dig Dis Sci 61:1165–1171
Acknowledgements
We would like to express our sincere appreciation to secretaries Ayaka Fujimoto of the Department of Surgery, Kansai Medical University.
Funding
The authors declare no funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures followed were in accordance with the ethical standards of the institutional committee on human experimentation and with the Helsinki Declaration.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study received IRB approval from our institution (Protocol Number, 2016697).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Matsui, Y., Hirooka, S., Sakaguchi, T. et al. Bile Duct Stones Predict a Requirement for Cholecystectomy in Older Patients. World J Surg 44, 721–729 (2020). https://doi.org/10.1007/s00268-019-05241-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05241-2