Abstract
Background
Africa’s health workforce crisis has recently been emphasized by major international organizations. As a part of this discussion, it has become apparent that the workforce required to deliver surgical services has been significantly neglected.
Methods
This paper reviews some of the reasons for this relative neglect and emphasizes its importance to health systems and public health. We report the first comprehensive analysis of the surgical workforce in Uganda, identify challenges to workforce development, and evaluate current programs addressing these challenges. This was performed through a literature review, analysis of existing policies to improve surgical access, and pilot retrospective studies of surgical output and workforce in nine rural hospitals.
Results
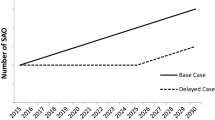
Uganda has a shortage of surgical personnel in comparison to higher income countries, but the precise gap is unknown. The most significant challenges to workforce development include recruitment, training, retention, and infrastructure for service delivery. Curricular innovations, international collaborations, and development of research capacity are some of the initiatives underway to overcome these challenges. Several programs and policies are addressing the maldistribution of the surgical workforce in urban areas. These programs include surgical camps, specialist outreach, and decentralization of surgical services. Each has the advantage of improving access to care, but sustainability has been an issue for all of these programs. Initial results from nine hospitals show that surgical output is similar to previous studies and lags far behind estimates in higher-income countries. Task-shifting to non-physician surgical personnel is one possible future alternative.
Conclusions
The experience of Uganda is representative of other low-income countries and may provide valuable lessons. Greater attention must be paid to this critical aspect of the global crisis in human resources for health.

Similar content being viewed by others
References
Garrett L (2007) The Challenge of Global Health. Foreign Affairs, Jan–Feb
Debas H, Gosselin R, McCord C, Thind A (2006) Surgery. In: Jamison D (ed) Disease control priorities in developing countries, 2nd edn. World Bank, Washington DC
Gosselin RA, Thind A, Bellardinelli A (2006) Cost/DALY averted in a small hospital in Sierra Leone: what is the relative contribution of different services? World J Surg 30:505–511
McCord C, Chowdhury Q (2003) A cost-effective small hospital in Bangladesh: what it can mean for emergency obstetric care. Int J Gynaecol Obstet 81:83–92
Laxminarayan R, Mills AJ, Breman JG, Measham AR, Alleyne G, Claeson M et al (2006) Advancement of global health: key messages from the Disease Control Priorities Project. Lancet 367(9517):1193–1208
Nordberg E, Holmberg S, Kiugu S (1995) Output of major surgery in developing countries. Towards a quantitative evaluation and planning tool. Trop Geogr Med 47:206–211
Fenton PM (1997) The epidemiology of district surgery in Malawi: a two-year study of surgical rates and indices in rural Africa. East Cent Afr J Surg 3:33–41
MacGowan WA (1987) Surgical manpower worldwide. Bull Am Coll Surg 72:5–9
Vaz F, Bergstrom S, Vaz ML, Langa J, Bugalho A (1999) Training medical assistants for surgery. Bull World Health Organ 77:688–691
Kruk M, Pereira C, Vaz F, Bergstrom S, Galea S (2007) Economic evaluation of surgically trained assistant medical officers in performing major obstetric surgery in Mozambique. BJOG 114:1253–1260
Longombe AO (1997) Surgical training of nurses for rural areas: necessity or aberration? East Cent Afr J Surg 3:43–47
The Bellagio Essential Surgery Group (2007) Increasing access to surgical services in resource-constrained settings in sub-Saharan Africa [in preparation]). Bellagio Essential Surgery Group, Italy
Bellagio Essential Surgery Group (2007) Improving Access to Surgery in sub-Saharan Africa. Available at: http://www.globalhealthsciences.ucsf.edu/bulletins/bulletins.aspx. Accessed 1 Oct 2007
WHO (2006) World Health Report: working together for health
Matsiko C, Kiwanuka J (2003) Overview of Human Resource for Health in Uganda. Health Policy and Development
Department of Surgery, Makerere University and Association of Surgeons of Uganda, 2007
Bickler SW, Rode H (2002) Surgical services for children in developing countries. Bull World Health Organ 80:829–835
El Khamlichi A (2005) Neurosurgery in Africa. Clin Neurosurg 52:214–217
Loefler IJ (2002) The specialist–generalist controversy. S Afr J Surg 40:87–89
Galukande M, Kijjambu S, Luboga S (2006) Improving recruitment of surgical trainees and training of surgeons in Uganda. East Cent Afr J Surg 11:17–24
Hodges SC, Mijumbi C, Okello M, McCormick BM, Walker IA, Wilson IH (2007) Anesthesia services in developing countries: defining the problems. Anesthesia 62:4–11
Angemi D, Oyugi J, Aziz I, Kyamukama T (2007) The money flows, the boy dies. International Herald Tribune, 25 April
Nsubuga FM, Jaakkola MS (2005) Needle stick injuries among nurses in sub-Saharan Africa. Trop Med Int Health 10:773–781
Newsom DH, Kiwanuka JP (2002) Needle-stick injuries in a Ugandan teaching hospital. Ann Trop Med Parasitol 96:517–522
Kiguli-Malwadde E, Kijjambu S, Kiguli S, Galukande M, Mwanika A, Luboga S et al (2006) Problem Based Learning, curriculum development and change process at Faculty of Medicine, Makerere University, Uganda. Afr Health Sci 6:127–130
Uyeno L, Watya S (2005) Strategies for improving surgical access in rural Uganda: evaluation of multifaceted outreach and specialist camps; presentation
Gruen RL, Bailie RS, Wang Z, Heard S, O’Rourke IC (2006) Specialist outreach to isolated and disadvantaged communities: a population-based study. Lancet 368(9530):130–138
Health subdistricts in Uganda. Ministry of Health, Kampala, 1999
Annual health sector performance report. Ministry of Health, Kampala, 2006
Watters DA, Bayley AC (1987) Training doctors and surgeons to meet the surgical needs of Africa. Br Med J (Clin Res Ed) 295(6601):761–763
Nabembezi JS, Nordberg E (2001) Surgical output in Kibaale district, Uganda. East Afr Med J 78:379–381
Levy LF, Chigwanda PC, Mauchaza B, Hatfill S, Bakasa R (1986) Prevalence of untreated disease in rural Zimbabwe. Cent Afr J Med 32:159–163
King M, Bewes P, Cairns J, Thornton J (1990) Primary surgery. Oxford University Press, Oxford
Saswata B, Omar F, Aubery RJ, Jaffer B, Walsh M (2005) Bridging the health gap in Uganda: the surgical role of the clinical officer. Afr Health Sci 5:86–89
Nundy S (1999) Difficulties of surgery in the developing world: a personal view. Lancet 353(Suppl 1):S121–S123
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ozgediz, D., Galukande, M., Mabweijano, J. et al. The Neglect of the Global Surgical Workforce: Experience and Evidence from Uganda. World J Surg 32, 1208–1215 (2008). https://doi.org/10.1007/s00268-008-9473-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9473-4