Abstract
Background
Delayed gastric emptying (DGE) following hiatus hernia surgery may affect a substantial number of patients with adverse clinical consequences. Here, we aim to evaluate the impact of DGE following laparoscopic repair of very large hiatus hernias on patients’ quality of life, gastrointestinal symptomatology, and daily function.
Methods
Analysis of data collected from a multicenter prospective randomised trial of patients who underwent laparoscopic mesh versus sutured repair of very large hiatus hernias (>50% of stomach in chest). DGE was defined as gastric food retention visualised at endoscopy after 6 h of fasting at 6 months post-surgery. Quality of life (QOL), gastrointestinal symptomatology, and daily function were assessed with the SF-36 questionnaire, Visick scoring and structured surveys administered prior to surgery and at 1, 3, 6 and 12 months after surgery.
Results
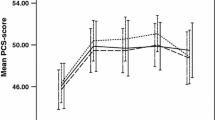
Nineteen of 102 (18.6%) patients had DGE 6 months after surgery. QOL questionnaires were completed in at least 80% of patients across all time points. Compared with controls, the DGE group demonstrated significantly lower SF-36 physical component scores, delayed improvement in health transition, more adverse gastrointestinal symptoms, higher Visick scores and a slower rate of return to normal daily activities. These differences were still present 12 months after surgery.
Conclusions
DGE following large hiatus hernia repair is associated with a negative impact on quality of life at follow-up to 12 months after surgery.





Similar content being viewed by others
References
Mitiek MO, Andrade RS (2010) Giant hiatal hernia. Ann Thorac Surg 89:2168–2173
Rashid F, Thangarajah T, Mulvey D et al (2010) A review article on gastric volvulus: a challenge to diagnosis and management. Int J Surg 8:18–24
Le Page PA, Furtado R, Hayward M et al (2015) Durability of giant hiatus hernia repair in 455 patients over 20 years. Ann R Coll Surg Engl 97:188–193
Engstrom C, Cai W, Irvine T et al (2012) Twenty years of experience with laparoscopic antireflux surgery. Br J Surg 99:1415–1421
Watson DI, Thompson SK, Devitt PG et al (2015) Laparoscopic repair of very large hiatus hernia with sutures versus absorbable mesh versus nonabsorbable mesh: a randomized controlled trial. Ann Surg 261:282–289
Koetje JH, Irvine T, Thompson SK et al (2015) Quality of life following repair of large hiatal hernia is improved but not influenced by use of mesh: results from a randomized controlled trial. World J Surg 39:1465–1473. https://doi.org/10.1007/s00268-015-2970-3
Dallemagne B, Kohnen L, Perretta S et al (2011) Laparoscopic repair of paraesophageal hernia. Long-term follow-up reveals good clinical outcome despite high radiological recurrence rate. Ann Surg 253:291–296
DeMeester SR (2013) Laparoscopic paraesophageal hernia repair: critical steps and adjunct techniques to minimize recurrence. Surg Laparosc Endosc Percutan Tech 23:429–435
Pallabazzer G, Santi S, Parise P et al (2011) Giant hiatal hernias: direct hiatus closure has an acceptable recurrence rate. Updates Surg 63:75–81
Wang Z, Bright T, Irvine T et al (2015) Outcome for asymptomatic recurrence following laparoscopic repair of very large hiatus hernia. J Gastrointest Surg 19:1385–1390
Cuschieri A, Hunter J, Wolfe B et al (1993) Multicenter prospective evaluation of laparoscopic antireflux surgery. Preliminary report. Surg Endosc 7:505–510
Trus TL, Bax T, Richardson WS et al (1997) Complications of laparoscopic paraesophageal hernia repair. J Gastrointest Surg 1:221–227
Tog C, Liu DS, Lim HK et al (2017) Risk factors for delayed gastric emptying following laparoscopic repair of very large hiatus hernias. BJS Open. https://doi.org/10.1002/bjs5.11
Koetje JH, Oor JE, Roks DJ et al (2017) Equal patient satisfaction, quality of life and objective recurrence rate after laparoscopic hiatal hernia repair with and without mesh. Surg Endosc. https://doi.org/10.1007/s00464-016-5405-9
Coleski R, Baker JR, Hasler WL (2016) Endoscopic gastric food retention in relation to scintigraphic gastric emptying delays and clinical factors. Dig Dis Sci 61:2593–2601
Brazier JE, Harper R, Jones NM et al (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30:473–483
Rijnhart-De Jong HG, Draaisma WA, Smout AJ et al (2008) The Visick score: a good measure for the overall effect of antireflux surgery? Scand J Gastroenterol 43:787–793
Yu D, Ramsey FV, Norton WF et al (2017) The burdens, concerns, and quality of life of patients with gastroparesis. Dig Dis Sci 62:879–893
Woodhouse S, Hebbard G, Knowles SR (2017) Psychological controversies in gastroparesis: a systematic review. World J Gastroenterol 23:1298–1309
Congreve DP (1992) Laparoscopic paraesophageal hernia repair. J Laparoendosc Surg 2:45–48
Falk GL, Brancatisano R (1992) Early recovery from laparoscopic repair of hiatus hernia. Med J Aust 156:440
Karim MA, Maloney J, Ali A (2016) Laparoscopic repair of intrathoracic stomach: clinical and health-related quality of life outcomes. Surg Laparosc Endosc Percutan Tech 26:484–487
Castelijns PSS, Ponten JEH, Van de Poll MCG et al (2017) Subjective outcome after laparoscopic hiatal hernia repair for intrathoracic stomach. Langenbecks Arch Surg 402:521–530
Poghosyan T, Gaujoux S, Chirica M et al (2011) Functional disorders and quality of life after esophagectomy and gastric tube reconstruction for cancer. J Visc Surg 148:327–335
Hamrick MC, Davis SS, Chiruvella A et al (2013) Incidence of delayed gastric emptying associated with revisional laparoscopic paraesophageal hernia repair. J Gastrointest Surg 17:213–217
Stein B, Everhart KK, Lacy BE (2015) Gastroparesis: a review of current diagnosis and treatment options. J Clin Gastroenterol 49:550–558
Gerritsen A, Furnee EJ, Gooszen HG et al (2013) Evaluation of gastrectomy in patients with delayed gastric emptying after antireflux surgery or large hiatal hernia repair. World J Surg 37:1065–1071. https://doi.org/10.1007/s00268-013-1953-5
Zhang L, Hou SC, Miao JB et al (2017) Risk factors for delayed gastric emptying in patients undergoing esophagectomy without pyloric drainage. J Surg Res 213:46–50
Zahiri HR, Weltz AS, Sibia US et al (2017) Primary versus redo paraesophageal hiatal hernia repair: a comparative analysis of operative and quality of life outcomes. Surg Endosc. https://doi.org/10.1007/s00464-017-5583-0
Suppiah A, Sirimanna P, Vivian SJ et al (2017) Temporal patterns of hiatus hernia recurrence and hiatal failure: quality of life and recurrence after revision surgery. Dis Esophagus 30:1–8
Zhang C, Liu D, Li F et al (2017) Systematic review and meta-analysis of laparoscopic mesh versus suture repair of hiatus hernia: objective and subjective outcomes. Surg Endosc. https://doi.org/10.1007/s00464-017-5586-x
Acknowledgements
This research was supported by project grants from the National Health and Medical Research Council (NHMRC) of Australia (375111 and 1022722).
Author information
Authors and Affiliations
Contributions
DSL and CT performed data acquisition and analysis. DSL, CT, PS and HKL were involved in the interpretation of the data. CT, DSL, HKL, SKT, PS, DIW and AA contributed to study design as well as preparing, editing, reviewing and approving the submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interests.
Rights and permissions
About this article
Cite this article
Liu, D.S., Tog, C., Lim, H.K. et al. Delayed Gastric Emptying Following Laparoscopic Repair of Very Large Hiatus Hernias Impairs Quality of Life. World J Surg 42, 1833–1840 (2018). https://doi.org/10.1007/s00268-017-4362-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4362-3