Abstract
Background
Arterial lactate is frequently monitored to indicate tissue hypoxia and direct therapy. We sought to determine whether early post-hepatectomy lactate (PHL) is associated with adverse outcomes and define factors associated with PHL.
Methods
Hepatectomy patients at a single institution from 2003 to 2012 with PHL available were included. Univariable and multivariable analyses examined factors associated with PHL and the relationship between PHL and 30-day major morbidity (Clavien grade III–V), 90-day mortality, and length of stay (LOS).
Results
Of 749 hepatectomies, 490 were included of whom 71.4% had elevated PHL (≥2 mmol/L). Cirrhosis (coefficient 0.31, p = 0.039), Charlson comorbidity index (coefficient 0.05, p < 0.001), major resections (coefficient 0.34, p < 0.001), procedure time (coefficient 0.08, p < 0.001), and blood loss (coefficient 0.11, p < 0.001) were associated with PHL. As lactate increased from <2 to ≥6 mmol/L, morbidity rose from 11.6 to 40.6%, and mortality from 0.7 to 22.7%. PHL was independently associated with 90-day mortality (OR 1.52 p < 0.001) and 30-day morbidity (OR 1.19, p = 0.002), but not LOS (rate ratio 1.03, p = 0.071).
Conclusion
Patients with elevated PHL in the initial postoperative period should be carefully monitored due to increased risk of major morbidity and mortality. Further research on the impact of lactate-directed fluid therapy is warranted.


Similar content being viewed by others
References
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S et al (2002) Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg 236(4):397–406 (discussion -7)
Belghiti J, Hiramatsu K, Benoist S, Massault P, Sauvanet A, Farges O (2000) Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg 191(1):38–46
Farges O, Goutte N, Bendersky N, Falissard B, Group A-FHS (2012) Incidence and risks of liver resection: an all-inclusive French nationwide study. Ann Surg 256(5):697–704 (discussion -5)
Virani S, Michaelson JS, Hutter MM, Lancaster RT, Warshaw AL, Henderson WG et al (2007) Morbidity and mortality after liver resection: results of the patient safety in surgery study. J Am Coll Surg 204(6):1284–1292
Aloia TA, Fahy BN, Fischer CP, Jones SL, Duchini A, Galati J et al (2009) Predicting poor outcome following hepatectomy: analysis of 2313 hepatectomies in the NSQIP database. HPB (Oxford) 11(6):510–515
Shubert CR, Habermann EB, Truty MJ, Thomsen KM, Kendrick ML, Nagorney DM (2014) Defining perioperative risk after hepatectomy based on diagnosis and extent of resection. J Gastrointest Surg 18(11):1917–1928
Tzeng CW, Cooper AB, Vauthey JN, Curley SA, Aloia TA (2014) Predictors of morbidity and mortality after hepatectomy in elderly patients: analysis of 7621 NSQIP patients. HPB (Oxford) 16(5):459–468
Hyder O, Pulitano C, Firoozmand A, Dodson R, Wolfgang CL, Choti MA et al (2013) A risk model to predict 90-day mortality among patients undergoing hepatic resection. J Am Coll Surg 216(6):1049–1056
Etra JW, Squires MH, Fisher SB, Rutz DR, Martin BM, Kooby DA et al (2014) Early identification of patients at increased risk for hepatic insufficiency, complications and mortality after major hepatectomy. HPB (Oxford) 16(10):875–883
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D et al (2005) The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242(6):824–828 (discussion 8–9)
Herbert GS, Prussing KB, Simpson AL, D’Angelica MI, Allen PJ, DeMatteo RP et al (2015) Early trends in serum phosphate and creatinine levels are associated with mortality following major hepatectomy. HPB (Oxford) 17(12):1058–1065
Lim C, Dejong CH, Farges O (2015) Improving the quality of liver resection: a systematic review and critical analysis of the available prognostic models. HPB (Oxford) 17(3):209–221
Meyer ZC, Schreinemakers JM, Mulder PG, de Waal RA, Ermens AA, van der Laan L (2013) Determining the clinical value of lactate in surgical patients on the intensive care unit. J Surg Res 183(2):814–820
Bakker J, Nijsten MW, Jansen TC (2013) Clinical use of lactate monitoring in critically ill patients. Ann Intensive Care 3(1):12
Casserly B, Phillips GS, Schorr C, Dellinger RP, Townsend SR, Osborn TM et al (2015) Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med 43(3):567–573
Vandromme MJ, Griffin RL, Weinberg JA, Rue LW, Kerby JD (2010) Lactate is a better predictor than systolic blood pressure for determining blood requirement and mortality: could prehospital measures improve trauma triage? J Am Coll Surg 210(5):861–867 (7–9)
Phypers B, Pierce J (2006) Lactate physiology in health and disease. Contin Educ Anesth Crit Care Pain 6(3):128–132
Wiggans MG, Starkie T, Shahtahmassebi G, Woolley T, Birt D, Erasmus P et al (2013) Serum arterial lactate concentration predicts mortality and organ dysfunction following liver resection. Perioper Med (Lond) 2(1):21
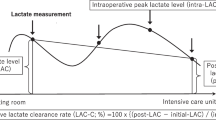
Vibert E, Boleslawski E, Cosse C, Adam R, Castaing D, Cherqui D et al (2015) Arterial lactate concentration at the end of an elective hepatectomy is an early predictor of the postoperative course and a potential surrogate of intraoperative events. Ann Surg 262(5):787–793
Meguro M, Mizuguchi T, Kawamoto M, Nishidate T, Ishii M, Tatsumi H et al (2014) Highest intraoperative lactate level could predict postoperative infectious complications after hepatectomy, reflecting the Pringle maneuver especially in chronic liver disease. J Hepatobiliary Pancreat Sci 21(7):489–498
Pietsch UC, Herrmann ML, Uhlmann D, Busch T, Hokema F, Kaisers UX et al (2010) Blood lactate and pyruvate levels in the perioperative period of liver resection with Pringle maneuver. Clin Hemorheol Microcirc 44(4):269–281
Cheng ES, Hallet J, Hanna SS, Law CH, Coburn NG, Tarshis J et al (2016) Is central venous pressure still relevant in the contemporary era of liver resection? J Surg Res 200(1):139–146
Melendez JA, Arslan V, Fischer ME, Wuest D, Jarnagin WR, Fong Y et al (1998) Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg 187(6):620–625
Pagano D, Tropea A, Cintorino D, Biondi A, Spada M, Gruttadauria S (2015) The unreliability of continuous postoperative lactate monitoring after extended hepatectomies: single center experience. Updates Surg. 67(1):33–37
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Bui L, Smith A, Bercovici M, Szalai J, Hanna S (2002) Minimising blood loss and transfusion requirements in hepatic resection. HPB 4(1):5–10
Watanabe I, Mayumi T, Arishima T, Takahashi H, Shikano T, Nakao A et al (2007) Hyperlactemia can predict the prognosis of liver resection. Shock 28(1):35–38
Lock JF, Malinowski M, Seehofer D, Hoppe S, Röhl RI, Niehues SM et al (2012) Function and volume recovery after partial hepatectomy: influence of preoperative liver function, residual liver volume, and obesity. Langenbecks Arch Surg 397(8):1297–1304
Luchette FA, Jenkins WA, Friend LA, Su C, Fischer JE, James JH (2002) Hypoxia is not the sole cause of lactate production during shock. J Trauma 52(3):415–419
James JH, Wagner KR, King JK, Leffler RE, Upputuri RK, Balasubramaniam A et al (1999) Stimulation of both aerobic glycolysis and Na(+)–K(+)–ATPase activity in skeletal muscle by epinephrine or amylin. Am J Physiol 277(1 Pt 1):E176–E186
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J et al (2004) Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Intensive Care Med 30(4):536–555
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B et al (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345(19):1368–1377
Boleslawski E, Vibert E, Pruvot FR, Le Treut YP, Scatton O, Laurent C et al (2014) Relevance of postoperative peak transaminase after elective hepatectomy. Ann Surg 260(5):815–820 (discussion 20-1)
Funding
No funding was provided for this project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lemke, M., Karanicolas, P.J., Habashi, R. et al. Elevated Lactate is Independently Associated with Adverse Outcomes Following Hepatectomy. World J Surg 41, 3180–3188 (2017). https://doi.org/10.1007/s00268-017-4118-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4118-0