Abstract
Background
The Controlling Nutritional Status (CONUT) score is an objective tool widely used to assess nutritional status in patients with inflammatory disease, chronic heart failure, and chronic liver disease. The relationship between CONUT score and prognosis in patients who have undergone hepatic resection, however, has not been evaluated.
Methods
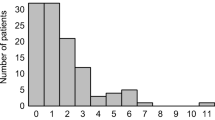
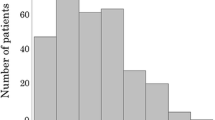
Data were retrospectively collected for 357 consecutive patients with hepatocellular carcinoma (HCC) who had undergone hepatic resection with curative intent between January 2004 and December 2015. The patients were assigned to two groups, those with preoperative CONUT scores ≤3 (low CONUT score) and >3 (high CONUT score), and their clinicopathological characteristics, surgical outcomes, and long-term survival were compared.
Results
Of the 357 patients, 69 (19.3%) had high (>3) and 288 (80.7%) had low (≤3) preoperative CONUT scores. High CONUT score was significantly associated with HCV infection, low serum albumin and cholesterol concentrations, low lymphocyte count, shorter prothrombin time, Child–Pugh B and liver damage B scores, and blood transfusion. Multivariate analysis identified six factors prognostic of poor overall survival (older age, liver damage B score, high CONUT score, poor tumor differentiation, the presence of intrahepatic metastases, and blood transfusion) and five factors prognostic of reduced recurrence-free survival (older age, higher ICGR15, larger tumor size, presence of intrahepatic metastasis, and blood transfusion).
Conclusions
In patients with HCC, preoperative CONUT scores are predictive of poorer overall survival, even after adjustments for other known predictors.


Similar content being viewed by others
References
Alberino F, Gatta A, Amodio P et al (2001) Nutrition and survival in patients with liver cirrhosis. Nutrition 17:445–450
Caregaro L, Alberino F, Amodio P et al (1996) Malnutrition in alcoholic and virus-related cirrhosis. Am J Clin Nutr 63:602–609
Takenaka K, Kawahara N, Yamamoto K et al (1996) Results of 280 liver resections for hepatocellular carcinoma. Arch Surg 131:71–76
Taketomi A, Kitagawa D, Itoh S et al (2007) Trends in morbidity and mortality after hepatic resection for hepatocellular carcinoma: an institute’s experience with 625 patients. J Am Coll Surg 204:580–587
Yamashita Y, Taketomi A, Itoh S et al (2007) Longterm favorable results of limited hepatic resections for patients with hepatocellular carcinoma: 20 years of experience. J Am Coll Surg 205:19–26
Lien YC, Hsieh CC, Wu YC et al (2004) Preoperative serum albumin level is a prognostic indicator for adenocarcinoma of the gastric cardia. J Gastointest Surg 8:1041–1048
Ray-Coquard I, Cropet C, Van Glabbeke M et al (2009) Lymphopenia as a prognostic factor for overall in advanced carcinomas, sarcomas, and lymphomas. Cancer Res 69:5383–5391
Schwegler I, von Holzen A, Gutzwiller JP et al (2010) Nutritional risk is a clinical predictor of postoperative mortality and morbidity in surgery for colorectal cancer. Br J Surg 97:92–97
de Ulibarri Perez JI, Gonzalez-Madrono A, de Villar NG et al (2005) CONUT: a tool for Controlling Nutritional Status. First validation in a hospital population. Nutr Hosp 20:38–45
Ueno T, Hirayama S, Ito M et al (2013) Albumin concentration determined by the modified bromocresol purple method is superior to that by the bromocresol green method for assessing nutritional status in malnourished patients with inflammation. Ann Clin Biochem 50:576–584
Nakagomi A, Kohashi K, Morisawa T et al (2016) Nutritional status is associated with inflammation and predicts a poor outcome in patients with chronic heart failure. J Atheroscler Thromb 23(6):713–727
Narumi T, Arimoto T, Funayama A et al (2013) Prognostic importance of objective nutritional indexes in patients with chronic heart failure. J Cardiol 62:307–313
Taniguchi E, Kawaguchi T, Otsuka M et al (2013) Nutritional assessments for ordinary medical care in patients with chronic liver disease. Hepatol Res 43:192–199
Lopez-Larramona G, Lucendo AJ, Tenias JM (2015) Association between nutritional screening via the controlling nutritional status index and bone mineral density in chronic liver disease of various etiologies. Hepatol Res 45:618–628
Iseki Y, Shibutani M, Maeda K et al (2014) Impact of the preoperative controlling nutritional status (CONUT) score on the survival after curative surgery for colorectal cancer. PLoS ONE 10:e0132488
Hirahara N, Matsubara T, Hayashi H et al (2016) Prognostic importance of controlling nutritional status in patients undergoing curative thoracoscopic esophagectomy for esophageal cancer. Am J Ther. doi:10.1097/MJT.0000000000000414
Liver cancer study group of Japan (2003) General rules for the clinical and pathological study of primary liver cancer, Second English edition edn. Kanehara & Co, Tokyo, pp 34–35
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Shimada M, Takenaka K, Gion T et al (1996) Prognosis of recurrent hepatocellular carcinoma: a 10-year surgical experience in Japan. Gastroenterology 111:720–726
Rahbari NN, Koch M, Mehabi A et al (2009) Portal triad clamping versus vascular exclusion for vascular control during hepatic resection: a systematic review and meta-analysis. J Gastrointest Surg 13:558–568
de Ulibarri Perez JI, Femandez G, Rodriguez Salvanes F et al (2014) Nutritional screening control of clinical undernutrition with analytical parameters. Nutr Hosp 29:797–811
Yoshida N, Baba Y, Shigaki H, Harada K et al (2016) Preoperative nutritional assessment by controlling nutritional status (CONUT) is useful to estimate postoperative morbidity after esophagectomy for esophageal cancer. World J Surg 40(8):1910–1917. doi:10.1007/s00423-017-1553-1
Harimoto N, Shirabe K, Ikegami T et al (2015) Postoperative complications are predictive of poor prognosis in hepatocellular carcinoma. J Surg Res 199(2):470–477
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Mantovani A, Allavena P, Sica A et al (2008) Cancer-related inflammation. Nature 454:436–444
Roxburgh CS, McMillan DC (2010) Role of systemic inflammatory response in predicting survival in patients with primary operative cancer. Future Oncol 6:149–163
Katz SC, Shia J, Liau KH et al (2009) Operative blood loss independently predicts recurrence and survival after resection of hepatocellular carcinoma. Ann Surg 249:617–623
Harada N, Shirabe K, Maeda T et al (2015) Blood transfusion is associated with recurrence of hepatocellular carcinoma after hepatectomy in Child–Pugh class A patients. World J Surg 39:1044–1051. doi:10.1007/s00268-014-2891-6
Gascon P, Zoumbos NC, Young NS (1984) Immunological abnormalities in patients receiving multiple blood transfusions. Ann Intern Med 100:173–177
Kaplan J, Sarnaik S, Gitlin J et al (1984) Diminished helper/suppressor lymphocyte ratios and natural killer activity in recipients of repeated blood transfusions. Blood 64:308–310
Itoh S, Fukuzawa K, Shitomi Y, Okamoto M et al (2012) Impact of the VIO system in hepatic resection for patients with hepatocellular carcinoma. Surg Today 42:1176–1182
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There was no conflict of interest and financial support.
Rights and permissions
About this article
Cite this article
Harimoto, N., Yoshizumi, T., Sakata, K. et al. Prognostic Significance of Preoperative Controlling Nutritional Status (CONUT) Score in Patients Undergoing Hepatic Resection for Hepatocellular Carcinoma. World J Surg 41, 2805–2812 (2017). https://doi.org/10.1007/s00268-017-4097-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4097-1