Abstract
Background
Right-sided hepatectomy is often selected for perihilar cholangiocarcinoma, due to the anatomic consideration that “the left hepatic duct is longer than that of the right hepatic duct”. However, only one study briefly mentioned the length of the hepatic ducts. Our aim is to investigate whether the consideration is correct.
Methods
In surgical study, the lengths of the resected bile duct were measured using pictures of the resected specimens in 475 hepatectomized patients with perihilar cholangiocarcinoma. In radiological study, the estimated lengths of the bile duct to be resected were measured using cholangiograms reconstructed from computed tomography images in 61 patients with distal bile duct obstruction.
Results
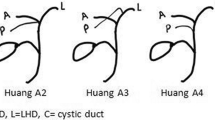
In surgical study, the length of the resected left hepatic duct was 25.1 ± 6.4 mm in right trisectionectomy (n = 37) and 14.9 ± 5.7 mm in right hepatectomy (n = 167). The length of the right hepatic duct was 14.1 ± 5.7 mm in left hepatectomy (n = 149) and 21.3 ± 6.4 mm in left trisectionectomy (n = 122). In radiological study, the lengths of the bile duct corresponding to the surgical study were 34.1 ± 7.8, 22.4 ± 7.1, 20.8 ± 4.8, and 31.6 ± 5.3 mm, respectively. Both studies determined that the lengths of the resected bile ducts were (1) similar between right and left hepatectomies, (2) significantly shorter in right hepatectomy than in left trisectionectomy, and (3) the longest in right trisectionectomy.
Conclusions
The aforementioned anatomical assumption is a surgeon’s biased view. Based on our observations, a flexible procedure selection is recommended.





Similar content being viewed by others
References
Nakeeb A, Pitt HA, Sohn TA et al (1996) Cholangiocarcinoma: a spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg 224:463–473
Ebata T, Kamiya J, Nishio H et al (2009) The concept of perihilar cholangiocarcinoma is valid. Br J Surg 96:926–934
Neuhaus P, Jonas S, Bechstein WO et al (1999) Extended resections for hilar cholangiocarcinoma. Ann Surg 230:808–818
Seyama Y, Kubota K, Sano K et al (2003) Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg 238:73–83
Kawasaki S, Imamura H, Kobayashi A et al (2003) Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg 238:84–92
Ikeyama T, Nagino M, Oda K et al (2007) Surgical approach to Bismuth type I and II hilar cholangiocarcinomas: audit of 54 consecutive cases. Ann Surg 246:1052–1057
Nagino M, Ebata T, Yokoyama Y et al (2013) Evolution of surgical treatment for perihilar cholangiocarcinoma: a single-center 34-year review of 574 consecutive resections. Ann Surg 258:129–140
Couinaud C (1999) Tell me more about liver anatomy. Paris Chirurgie 124:587–588
Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y (2006) “Anatomic” right hepatic trisectionectomy (extended right hepatectomy) with caudate lobectomy for hilar cholangiocarcinoma. Ann Surg 243:28–32
Kaneoka Y, Yamaguchi A, Isogai M et al (2000) Hepatectomy for cholangiocarcinoma complicated with right umbilical portion: anomalous configuration of the intrahepatic biliary tree. J Hepatobiliary Pancreat Surg 7:321–326
Ohkubo M, Nagino M, Kamiya J et al (2004) Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg 239:82–86
Natsume S, Ebata T, Yokoyama Y et al (2012) Clinical significance of left trisectionectomy for perihilar cholangiocarcinoma: an appraisal and comparison with left hepatectomy. Ann Surg 255:754–762
Matsumoto N, Ebata T, Igami T et al (2014) Appraisal of “anatomic” right hepatic trisectionectomy for perihilar cholangiocarcinoma. Br J Surg 101:261–268
Bismuth H (1982) Surgical anatomy and anatomical surgery of the liver. World J Surg 6:3–9. doi:10.1007/BF01656368
Couinaud C (1989) Surgical anatomy of the liver revisited. C. Couinaud, Paris
Chen HW, Pan AZ, Zhen ZJ et al (2006) Preoperative evaluation of resectability of Klatskin tumor with 16-MDCT angiography and cholangiography. Am J Roentgenol 186:1580–1586
Sasaki R, Kondo T, Oda T et al (2011) Impact of three-dimensional analysis of multidetector row computed tomography cholangioportography in operative planning for hilar cholangiocarcinoma. Am J Surg 202:441–448
Artioli D, Tagliabue M, Aseni P, Sironi S, Vanzulli A et al (2010) Detection of biliary and vascular anatomy in living liver donors: value of gadobenate dimeglumine enhanced MR and MDCT angiography. Eur J Radiol 76:e1–e5
Soga K, Ochiai J, Kasai K et al (2013) Development of a novel fusion imaging technique in the diagnosis of hepatobiliary-pancreatic lesions. J Med Imaging Radiat Oncol 57:306–313
Shimizu H, Kimura F, Yoshidome H et al (2010) Aggressive surgical resection for hilar cholangiocarcinoma of the left-side predominance: radicality and safety of left-sided hepatectomy. Ann Surg 251:281–286
Hosokawa I, Shimizu H, Yoshidome H et al (2014) Surgical strategy for hilar cholangiocarcinoma of the left-sided predominance: current role of left trisectionectomy. Ann Surg 259:1178–1185
Bismuth H, Corlette MB (1975) Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet 140:170–176
Bismuth H, Nakache R, Diamond T (1992) Management strategies in resection for hilar cholangiocarcinoma. Ann Surg 215:31–38
Yokoyama Y, Nishio H, Ebata T et al (2010) Value of indocyanine green clearance of the future liver remnant in predicting outcome after resection for biliary cancer. Br J Surg 97:1260–1268
Nagino M, Nimura Y, Kamiya J et al (1995) Right or left trisegment portal vein embolization before hepatic trisegmentectomy for hilar bile duct carcinoma. Surgery 117:677–681
Sugiura T, Nishio H, Nagino M et al (2008) Value of multidetector-row computed tomography in diagnosis of portal vein invasion by perihilar cholangiocarcinoma. World J Surg 32:1478–1484. doi:10.1007/s00268-008-9547-3
Fukami Y, Ebata T, Yokoyama Y et al (2012) Diagnostic ability of MDCT to assess right hepatic artery invasion by perihilar cholangiocarcinoma with left-sided predominance. J Hepatobiliary Pancreat Sci 19:179–186
Nagino M, Nimura Y, Nishio H et al (2010) Hepatectomy with simultaneous resection of the portal vein and hepatic artery for advanced perihilar cholangiocarcinoma: an audit of 50 consecutive cases. Ann Surg 252:115–123
Yoshioka Y, Ebata T, Yokoyama Y et al (2011) “Supraportal” right hepatic artery: an anatomic trap in hepatobiliary and transplant surgery. World J Surg 35:1340–1344. doi:10.1007/s00268-011-1075-x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirose, T., Igami, T., Ebata, T. et al. Surgical and Radiological Studies on the Length of the Hepatic Ducts. World J Surg 39, 2983–2989 (2015). https://doi.org/10.1007/s00268-015-3201-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3201-7