Abstract
Background
The aim of this study was to explore the impact of chronic concomitant disease on the risk for postoperative complications following open groin hernia surgery.
Methods
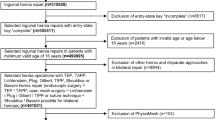
During the study period (2002–2011), 133,074 open repairs were registered in the Swedish Hernia Register. History of peripheral vascular disorders, connective tissue disease, chronic renal failure, obesity, and liver cirrhosis as well as data on hemorrhage or hematoma, wound dehiscence, postoperative infection, and reoperation for superficial infection or bleeding within 30 days after surgery were obtained by matching with the Swedish Patient Register.
Results
In the multivariate logistic regression analysis, a significantly increased risk for hemorrhage or hematoma within 30 days after surgery was seen for older patients, males, liver cirrhosis, peripheral vascular disease, and connective tissue disease (p < 0.05). High age (>80 years), previous history of peripheral vascular disease, connective tissue disease, and male gender were risk factors for wound dehiscence (p < 0.05). Liver cirrhosis, chronic kidney disease, BMI > 25, and male gender were associated with increased risk for postoperative wound infection (p < 0.05). A significantly increased risk for reoperation for superficial infection or bleeding was seen in patients with peripheral vascular disease and elderly patients (p < 0.05).
Conclusion
Risk for postoperative complications in open groin hernia surgery is increased in elderly patients, patients with liver cirrhosis, and those with peripheral vascular disease. The indications for surgery should be weighed against the risk for wound-healing complications in these patient groups. Watchful waiting may be an alternative, although this carries the risk of emergency surgery.
Similar content being viewed by others
References
Lundström KJ, Sandblom G, Smedberg S, Nordin P (2012) Risk factors for complications in groin hernia surgery; a National Register Study. Ann Surg 255(4):784–788
Fränneby U, Sandblom G, Nordin P, Nyrén O, Gunnarsson U (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244(2):212–219
Gopal SV, Warrier A (2013) Recurrence after groin hernia repair-revisited. Int J Surg. 11(5):374–377
The Swedish Hernia Register. Available at: http://www.svensktbrackregister.se. Accessed 27 June 2014
The National Patient Register. Available at: http://www.socialstyrelsen.se/register/halsodataregister/patientregistret/inenglish. Accessed 27 June 2014
Lisman T, Porte RJ (2010) Rebalanced hemostasis in patients with liver disease: evidence and clinical consequences. Blood 116(6):878–885
Johnson WC, Williford WO, Corson JD, Padberg FT Jr (2004) Hemorrhagic complications during long-term postoperative warfarin administration in patients undergoing lower extremity arterial bypass surgery. Vascular 12(6):362–368
Borg M, Brincat S, Camilleri G, Schembri-Wismayer P, Brincat M, Calleja-Agius J (2013) The role of cytokines in skin aging. Climacteric 16(5):514–521
Chana P, Chadwick MA, Pullyblank AM (2012) Achieving abdominal closure following emergency laparotomy in patients with connective tissue disorders. Ann R Coll Surg Engl 94(3):212–213
Pieringer H, Stuby U, Biesenbach G (2007) Patients with rheumatoid arthritis undergoing surgery: how should we deal with antirheumatic treatment? Semin Arthritis Rheum 36(5):278–286
Zawadowski M, Gjevre JA, Nair BV, Taylor-Gjevre RM (2011) Management of rheumatoid arthritis in the perioperative period. Can J Surg 54(5):E6–E7
Heller A, Westphal SE, Bartsch P, Haase M, Mertens PR (2014) Chronic kidney disease is associated with high abdominal incisional hernia rates and wound healing disturbances. Int Urol Nephrol 46(6):1175–1181
Silverstein P (1992) Smoking and wound healing. Am J Med 93(1A):22S–24S
Oh HK, Kim H, Ryoo S, Choe EK, Park KJ (2011) Inguinal hernia repair in patients with cirrhosis is not associated with increased risk of complications and recurrence. World J Surg 35(6):1229–1233
Canedo J, Ricciardi K, DaSilva G, Rosen L, Weiss EG, Wexner SD (2013) Are postoperative complications more common following colon and rectal surgery in patients with chronic kidney disease? Colorectal Dis 15(1):85–90
Compagna R, Rossi R, Fappiano F, Bianco T, Accurso A, Danzi M, Massa S, Aprea G, Amato B (2013) Emergency groin hernia repair: implications in elderly. BMC Surg 13(Suppl 2):S29
Azari Y, Perry Z, Kirshtein B (2015) Strangulated groin hernia in octogenarians. Hernia 19(3):443–447
Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J et al (2014) Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 18:151–163
Fitzgibbons RJ Jr, Forse RA (2015) Clinical practice. Groin hernias in adults. N Engl J Med 372(8):756–763
Hwang MJ, Bhangu A, Webster CE, Bowley DM, Gannon MX, Karandikar SS (2014) Unintended consequences of policy change to watchful waiting for asymptomatic inguinal hernias. Ann R Coll Surg Engl 96(5):343–347
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rühling, V., Gunnarsson, U., Dahlstrand, U. et al. Wound Healing Following Open Groin Hernia Surgery: The Impact of Comorbidity. World J Surg 39, 2392–2399 (2015). https://doi.org/10.1007/s00268-015-3131-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3131-4