Abstract
Purpose
The use of biophysical stimuli produced by extracorporeal shock wave therapy (ESWT) can improve the rehabilitation treatment of patients undergoing total knee arthroplasty (TKA). The aim of our study is to evaluate the short-term efficacy of early postoperative ESWT in combination with physiotherapy in terms of pain reduction and motor function recovery of patients undergoing TKA and compare it with conventional physiotherapy treatment.
Methods
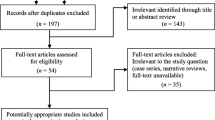
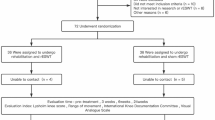
Fifty-six patients undergoing TKA were enrolled in the study from January 2019 to February 2020. Patients received two sessions of physiotherapy daily, with (experimental group) or without (control group) four sessions of ESWT within seven days after surgery. Patients were prospectively evaluated at baseline and at post-operative day two and seven. Assessment included active knee range of motion (aROM), timed up and go (TUG) test, visual analogue scale (VAS) for pain, and Borg scale.
Results
Fifty patients completed the study. Both treatments proved to be effective in reducing pain and improving the knee range of motion and functional scores at seven days after surgery: the aROM in the ESWT group was 36.8 ± 11.0 grades (p < 0.001), while in control group was 19.8 ± 7.8 grades (p < 0.001). TUG, VAS, and BORG scores showed a similar trend. Comparative analysis revealed superior clinical results for the experimental group in all the outcomes, in particular aROM (96.0 ± 5.40 vs. 81.20 ± 11.01, p < 0.001) and TUG test (17.4 ± 5.61 vs. 21.24 ± 5.88, p < 0.001), at day seven after surgery.
Conclusion
Early application of ESWT in addition to physiotherapy can positively influence the rehabilitation process after TKA. The treatment proved to be well tolerated and safe. Preliminary results demonstrated better pain control and functional scores compared to physiotherapy alone.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available to the authors and will be granted only upon reasoned request, subject to the authors’ evaluation.
References
Bijlsma JWJ, Berenbaum F, Lafeber FPJG (2011) Osteoarthritis: an update with relevance for clinical practice. Lancet Lond Engl 377(9783):2115–26. https://doi.org/10.1016/S0140-6736(11)60243-2
Monticone M, Frigau L, Sconza C, Foti C, Mola F, Respizzi S (2019) Italian version of the risk assessment and prediction tool: properties and usefulness of a decision-making tool for subjects’ discharge after total hip and knee arthroplasty. Int J Stat Med Res 4(8):8–16. https://doi.org/10.6000/1929-6029.2019.08.02
Bryan S, Goldsmith LJ, Davis JC, Hejazi S, MacDonald V, McAllister P, Randall E, Suryaprakash N, Wu AD, Sawatzky R (2018) Revisiting patient satisfaction following total knee arthroplasty: a longitudinal observational study. BMC Musculoskelet Disord 19(1):423. https://doi.org/10.1186/s12891-018-2340-z
Monticone M, Sconza C, Portoghese I, Nishigami T, Wand BM, Sorrentino G et al (2021) Cross-cultural adaptation, reliability and validity of the Fremantle Knee Awareness Questionnaire in Italian subjects with painful knee osteoarthritis. Health Qual Life Outcomes 19(1):114. https://doi.org/10.1186/s12955-021-01754-4
König A, Walther M, Kirschner S, Gohlke F (2000) Balance sheets of knee and functional scores 5 years after total knee arthroplasty for osteoarthritis: a source for patient information. J Arthroplasty 15(3):289–294. https://doi.org/10.1016/s0883-5403(00)90532-1
Healthcare Cost and Utilization Project (HCUP). HCUP facts and figures: statistics on hospital-based care in the United States, 2009 [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US). http://www.ncbi.nlm.nih.gov/books/NBK91984/. Accessed 2 June 2023
Mandeville D, Osternig LR, Chou L-S (2008) The effect of total knee replacement surgery on gait stability. Gait Posture 27(1):103–109. https://doi.org/10.1016/j.gaitpost.2007.02.009
Wada M, Kawahara H, Shimada S, Miyazaki T, Baba H (2002) Joint proprioception before and after total knee arthroplasty. Clin Orthop 403:161–167. https://doi.org/10.1097/00003086-200210000-00024
Mistry JB, Elmallah RDK, Bhave A, Chughtai M, Cherian JJ, McGinn T et al (2016) Rehabilitative guidelines after total knee arthroplasty: a review. J Knee Surg 29(3):201–217. https://doi.org/10.1055/s-0036-1579670
Domínguez-Navarro F, Igual-Camacho C, Silvestre-Muñoz A, Roig-Casasús S, Blasco JM (2018) Effects of balance and proprioceptive training on total hip and knee replacement rehabilitation: a systematic review and meta-analysis. Gait Posture 62:68–74. https://doi.org/10.1016/j.gaitpost.2018.03.003
Wainwright TW, Gill M, McDonald DA, Middleton RG, Reed M, Sahota O et al (2020) Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop 91(1):3–19. https://doi.org/10.1080/17453674.2019.1683790
Sconza C, Coletta F, Magarelli N, D’Agostino MC, Egan CG, Di Matteo B, Respizzi S, Mazziotti G (2022) Multimodal conservative treatment of migrating bone marrow edema associated with early osteonecrosis of the hip. SAGE Open Med Case Rep. 10:2050313X211067617. https://doi.org/10.1177/2050313X211067617
Moya D, Ramón S, Schaden W, Wang C-J, Guiloff L, Cheng J-H (2018) The role of extracorporeal shockwave treatment in musculoskeletal disorders. JBJS 100(3):251–63. https://doi.org/10.2106/JBJS.17.00661
d’Agostino MC, Craig K, Tibalt E, Respizzi S (2015) Shock wave as biological therapeutic tool: From mechanical stimulation to recovery and healing, through mechanotransduction. Int J Surg Lond Engl 24(Pt B):147–153. https://doi.org/10.1016/j.ijsu.2015.11.030
Sukubo NG, Tibalt E, Respizzi S, Locati M, d’Agostino MC (2015) Effect of shock waves on macrophages: a possible role in tissue regeneration and remodeling. Int J Surg Lond Engl 24(Pt B):124–130. https://doi.org/10.1016/j.ijsu.2015.07.719
Garibaldi R, Altomare D, Sconza C, Kon E, Castagna A, Marcacci M, Monina E, Di Matteo B (2021) Conservative management vs surgical repair in degenerative rotator cuff tears: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 25(2):609–619. https://doi.org/10.26355/eurrev_202101_24619
Sansone V, D’Agostino MC, Bonora C, Sizzano F, De Girolamo L, Romeo P (2012) Early angiogenic response to shock waves in a three-dimensional model of human microvascular endothelial cell culture (HMEC-1). J Biol Regul Homeost Agents 26(1):29–37
Viganò M, Sansone V, d’Agostino MC, Romeo P, PeruccaOrfei C, de Girolamo L (2016) Mesenchymal stem cells as therapeutic target of biophysical stimulation for the treatment of musculoskeletal disorders. J Orthop Surg 11(1):163. https://doi.org/10.1186/s13018-016-0496-5
Kisch T, Wuerfel W, Forstmeier V, Liodaki E, Stang FH, Knobloch K et al (2016) Repetitive shock wave therapy improves muscular microcirculation. J Surg Res 201(2):440–445. https://doi.org/10.1016/j.jss.2015.11.049
Wang B, Zhou J, Banie L, Reed-Maldonado AB, Ning H, Lu Z et al (2018) Low-intensity extracorporeal shock wave therapy promotes myogenesis through PERK/ATF4 pathway. Neurourol Urodyn 37(2):699–707. https://doi.org/10.1002/nau.23380
Notarnicola A, Covelli I, Maccagnano G, Marvulli R, Mastromauro L, Ianieri G et al (2018) Extracorporeal shockwave therapy on muscle tissue: the effects on healthy athletes. J Biol Regul Homeost Agents 32(1):185–193
Auersperg V, Trieb K (2020) Extracorporeal shock wave therapy: an update. EFORT Open Rev 5(10):584–592. https://doi.org/10.1302/2058-5241.5.190067
Gatewood CT, Tran AA, Dragoo JL (2017) The efficacy of post-operative devices following knee arthroscopic surgery: a systematic review. Knee Surg Sports Traumatol Arthrosc 25(2):501–516. https://doi.org/10.1007/s00167-016-4326-4
Wang CJ, Ko JY, Chou WY, Hsu SL, Ko SF, Huang CC, Chang HW (2014) Shockwave therapy improves anterior cruciate ligament reconstruction. J Surg Res 188(1):110–118. https://doi.org/10.1016/j.jss.2014.01.050
Bade MJ, Kittelson JM, Kohrt WM, Stevens-Lapsley JE (2014) Predicting functional performance and range of motion outcomes after total knee arthroplasty. Am J Phys Med Rehabil 93(7):579–585. https://doi.org/10.1097/PHM.0000000000000065
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39(2):142–148. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x
Jensen MP, Chen C, Brugger AM (2003) Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain 4(7):407–414. https://doi.org/10.1016/s1526-5900(03)00716-8
Arena S (2017) Rate perceived exertion as a measure of exercise intensity. Home Healthc Now 35(10):570. https://doi.org/10.1097/NHH.0000000000000614
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–83
Tasso F, Simili V, Di Matteo B, Monteleone G, Martorelli F, De Angelis A, D’Amato T, Bovio M, Altomare D, Campofreda G, Marcacci M, Scardino M (2022) A rapid recovery protocol for hip and knee replacement surgery: a report of the outcomes in a referral center. Eur Rev Med Pharmacol Sci 26(10):3648–3655. https://doi.org/10.26355/eurrev_202205_28860
Armitage P, Berry G, Matthews JNS (2002) Statistical methods in medical research, 4th edn. Blackwell, Oxford
Gautschi OP, Stienen MN, Corniola MV, Joswig H, Schaller K, Hildebrandt G, Smoll NR (2017) Assessment of the minimum clinically important difference in the timed up and go test after surgery for lumbar degenerative disc disease. Neurosurgery 80(3):380–385. https://doi.org/10.1227/NEU.0000000000001320
Danoff JR, Goel R, Sutton R, Maltenfort MG, Austin MS (2018) How much pain is significant? Defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty. J Arthroplasty. 33(7S):S71-S75.e2. https://doi.org/10.1016/j.arth.2018.02.029
Park KB, Shin JS, Lee J, Lee YJ, Kim MR, Lee JH, Shin KM, Shin BC, Cho JH, Ha IH (2017) Minimum clinically important difference and substantial clinical benefit in pain, functional, and quality of life scales in failed back surgery syndrome patients. Spine (Phila Pa 1976) 42(8):E474–E481. https://doi.org/10.1097/BRS.0000000000001950
Tashjian RZ, Deloach J, Porucznik CA, Powell AP (2009) Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 18(6):927–32. https://doi.org/10.1016/j.jse.2009.03.021
Maldonado DR, Kyin C, Owens JS, Rosinsky PJ, Jimenez AE, Lee MS, Domb BG (2022) Predictors of achieving the maximal outcome improvement threshold for willingness to undergo revision hip arthroscopy. Am J Sports Med 50(8):2174–2180. https://doi.org/10.1177/03635465221096872
Ries AL (2005) Minimally clinically important difference for the UCSD Shortness of Breath Questionnaire, Borg Scale, and Visual Analog Scale. COPD 2(1):105–110. https://doi.org/10.1081/copd-200050655
Escobar A, Quintana JM, Bilbao A, Aróstegui I, Lafuente I, Vidaurreta I (2007) Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis Cartilage 15(3):273–280. https://doi.org/10.1016/j.joca.2006.09.001
Ditton E, Johnson S, Hodyl N et al. (2020) Improving Patient outcomes following total knee arthroplasty: identifying rehabilitation pathways based on modifiable psychological risk and resilience factors. Front Psychol, 11:1061. Published 2020 May 29. https://doi.org/10.3389/fpsyg.2020.01061.
Natali F, Corradini L, Sconza C, Taylor P, Furlan R, Mercer SW, Gatti R (2023) Development of the Italian version of the Consultation and Relational Empathy (CARE) measure: translation, internal reliability, and construct validity in patients undergoing rehabilitation after total hip and knee arthroplasty. Disabil Rehabil 45(4):703–708. https://doi.org/10.1080/09638288.2022.2037742
Simplicio CL, Purita J, Murrell W, Santos GS, Dos Santos RG, Lana JFSD (2020) Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. J Clin Orthop Trauma 11(Suppl 3):S309–S318. https://doi.org/10.1016/j.jcot.2020.02.004
Sconza C, Anzà M, Di Matteo B, Lipina M, Kon E, Respizzi S, Tibalt E, D’Agostino MC (2022) Extracorporeal shock wave therapy for the treatment of osteonecrosis and bone vascular diseases: a systematic review of randomized controlled trials. Eur Rev Med Pharmacol Sci 26(8):2949–2959. https://doi.org/10.26355/eurrev_202204_28626
Rice DA, McNair PJ (2010) Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum 40(3):250–266. https://doi.org/10.1016/j.semarthrit.2009.10.001
ISMST Guidelines: https://www.shockwavetherapy.org/fileadmin/user_upload/ISMST_Guidelines.pdf. Accessed 2 June 2023
Acknowledgements
We would also thank our colleagues at the Department of Biomedical Sciences-Humanitas University (Rozzano, Italy), for their feedback and support throughout the research process.
Author information
Authors and Affiliations
Contributions
DM and MDA contributed to the concept and design of the study and performed the procedures described. CS, BDM, and FS collected the data and drafted the first version of the manuscript. EM and SR performed the data analysis and the interpretation of the results. GL and EK made a substantial contribution to the revision of the content of the study and updated the literature. All authors read and approved the content of the paper.
Corresponding author
Ethics declarations
Ethics approval
The Humanitas University Ethical Committee and Institutional Review Board approved the study protocol in the 24th July 2018 session with Authorization no. 2065.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for publication of all the images included in the paper.
Competing interests
The authors have no conflicts of interest to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Daniele Martini and Cristiano Sconza contributed equally to the article and should be considered first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martini, D., Sconza, C., Di Matteo, B. et al. Early application of extracorporeal shock wave therapy improves pain control and functional scores in patients undergoing total knee arthroplasty: a randomized controlled trial. International Orthopaedics (SICOT) 47, 2757–2765 (2023). https://doi.org/10.1007/s00264-023-05906-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-05906-7