Abstract
Purpose
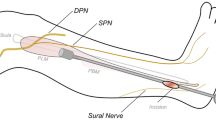
This study was conducted to provide anatomical data and surface markers for the safe and efficient exposure of surgical incisions for harvesting gracilis tendons (GT) and semitendinosus tendons (STT) while avoiding technical pitfalls and nerve injury during harvest for ligament reconstruction.
Methods
Seventy-four Chinese cadaveric lower limbs were dissected to expose the infrapatellar branch of the saphenous nerve (IPBSN) and pes anserinus (PA). Measurements of the borders and accessory bands of the PA tendons were taken. The arrangement of PA tendons and distribution of the IPBSN were assessed.
Results
The PA was roughly shaped like a quadrangle, with its superior border at the horizontal plane of the tibial tuberosity (TT). The GT and STT bifurcation point was located on the medial border of the PA. From medial side to lateral side, the sartorius tendons (ST), GT, and STT fused gradually and formed the lateral border of the PA at the distal end. The tendon arrangement of the PA was primarily affected by ST, which commonly covered GT and STT completely. Variant tendons were found in 41.9% of specimens. The insertion of the accessory bands was distal but close to the inferior border of the PA. Accessory bands were observed only in STT and ST, and STT accounted for the most. The width of the first accessory band of STT was similar to the width of the STT. Additionally, most of the IPBSNs were proximal to the horizontal plane of the TT.
Conclusion
For clearly exposing the GT and STT, it is crucial to expose the GT and STT bifurcation point on the medial border of the PA, whether directly or indirectly through the incision.The influence of ST insertion and the variability of tendons within the PA must be paid attention to during the operation. To protect IPBSNs highly, the incision should not be higher than the TT level.





Similar content being viewed by others
References
Keyhani S, Kazemi SM, Sajjadi MM, Elmi A (2020) A comparison between oblique and vertical incisions on the hamstring tendon harvesting in anterior cruciate ligament reconstruction and infrapatellar branch injury of the saphenous nerve. Rev Bras Ortop (Sao Paulo) 55:374–379
Paschos NK, Howell SM (2016) Anterior cruciate ligament reconstruction: principles of treatment. EFORT Open Rev 1:398–408
Marieswaran M, Jain I, Garg B, Sharma V, Kalyanasundaram D (2018) A Review on biomechanics of anterior cruciate ligament and materials for reconstruction. Appl Bionics Biomech 2018:4657824
Diermeier TA, Rothrauff BB, Engebretsen L, Lynch A, Svantesson E, Hamrin SEA, Meredith SJ, Rauer T, Ayeni OR, Paterno M, Xerogeanes JW, Fu FH, Karlsson J, Musahl V (2021) Treatment after ACL injury: panther symposium ACL treatment consensus group. Br J Sports Med 55:14–22
Evans J, Nielson J (2022) Anterior cruciate ligament knee injuries.
Joshi S, Shetty UC, Salim MD, Meena N, Kumar RS, Rao VKV (2021) Peroneus longus tendon autograft for anterior cruciate ligament reconstruction: a safe and effective alternative in nonathletic patients. Niger J Surg 27:42–47
Zeng C, Gao SG, Li H, Yang T, Luo W, Li YS, Lei GH (2016) Autograft versus allograft in anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials and systematic review of overlapping systematic reviews. Arthroscopy 32:153-163.e118
Yucens M, Aydemir AN (2019) Trends in anterior cruciate ligament reconstruction in the last decade: a web-based analysis. J Knee Surg 32:519–524
Ilahi OA, Stautberg EFR, Mansfield DJ, Qadeer AA (2017) Relationship of musculotendinous junction location to harvested semitendinosus and gracilis tendon length. Orthop J Sports Med 5:2325967117704630
Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH (2014) Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc 22:1467–1482
Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC (2005) Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy 21:791–803
Hudgens JL, Gillette BP, Krych AJ, Stuart MJ, May JH, Levy BA (2013) Allograft versus autograft in posterior cruciate ligament reconstruction: an evidence-based systematic review. J Knee Surg 26:109–115
Li J, Kong F, Gao X, Shen Y, Gao S (2016) Prospective randomized comparison of knee stability and proprioception for posterior cruciate ligament reconstruction with autograft, hybrid graft, and gamma-irradiated allograft. Arthroscopy 32:2548–2555
Mochizuki T, Akita K, Muneta T, Sato T (2004) Pes anserinus: layered supportive structure on the medial side of the knee. Clin Anat 17:50–54
Olewnik L, Gonera B, Podgorski M, Polguj M, Jezierski H, Topol M (2019) A proposal for a new classification of pes anserinus morphology. Knee Surg Sports Traumatol Arthrosc 27:2984–2993
Zhong S, Wu B, Wang M, Wang X, Yan Q, Fan X, Hu Y, Han Y, Li Y (2018) The anatomical and imaging study of pes anserinus and its clinical application. Medicine (Baltimore) 97:e0352
Amatuzzi MM, Cocco LF, Di Dio LJ, Gotfryd AO (2002) Surgical anatomy of the variations of the arrangement of the tendons of the muscles of the pes anserinus in male adults. Ital J Anat Embryol 107:29–35
Curtis BR, Huang BK, Pathria MN, Resnick DL, Smitaman E (2019) Pes anserinus: anatomy and pathology of native and harvested tendons. AJR Am J Roentgenol 213:1107–1116
Letartre R, Isida R, Pommepuy T, Miletic B (2014) Horizontal posterior hamstring harvest. Orthop Traumatol Surg Res 100:959–961
Khanna K, Janghala A, Pandya NK (2018) Use of posterior hamstring harvest during anterior cruciate ligament reconstruction in the pediatric and adolescent population. Orthop J Sports Med 6:2325967118775597
Yasin MN, Charalambous CP, Mills SP, Phaltankar PM (2010) Accessory bands of the hamstring tendons: a clinical anatomical study. Clin Anat 23:862–865
Boyle J, Eason A, Hartnett N, Marks P (2021) Infrapatellar branch of the saphenous nerve: a review. J Med Imaging Radiat Oncol 65:195–200
Arthornthurasook A, Gaew-Im K (1988) Study of the infrapatellar nerve. Am J Sports Med 16:57–59
Pekala PA, Tomaszewski KA, Henry BM, Ramakrishnan PK, Roy J, Mizia E, Walocha JA (2017) Risk of iatrogenic injury to the infrapatellar branch of the saphenous nerve during hamstring tendon harvesting: a meta-analysis. Muscle Nerve 56:930–937
Mousavi H, Mohammadi M, Aghdam HA (2018) Injury to the infrapatellar branch of the saphenous nerve during ACL reconstruction with hamstring tendon autograft: a comparison between oblique and vertical incisions. Arch Bone Jt Surg 6:52–56
Ruffilli A, De Fine M, Traina F, Pilla F, Fenga D, Faldini C (2017) Saphenous nerve injury during hamstring tendons harvest: does the incision matter? A systematic review. Knee Surg Sports Traumatol Arthrosc 25:3140–3145
Kalthur SG, Sumalatha S, Nair N, Pandey AK, Sequeria S, Shobha L (2015) Anatomic study of infrapatellar branch of saphenous nerve in male cadavers. Ir J Med Sci 184:201–206
Sharaby MMF, Alfikey A, Alhabsi IS, Al-Ghannami S (2019) No difference in sensory outcome between vertical and oblique incisions for hamstring graft harvest during ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27:146–152
Sabat D, Kumar V (2013) Nerve injury during hamstring graft harvest: a prospective comparative study of three different incisions. Knee Surg Sports Traumatol Arthrosc 21:2089–2095
Henry BM, Tomaszewski KA, Pekala PA, Graves MJ, Pekala JR, Sanna B, Mizia E (2018) Oblique incisions in hamstring tendon harvesting reduce iatrogenic injuries to the infrapatellar branch of the saphenous nerve. Knee Surg Sports Traumatol Arthrosc 26:1197–1203
Conte EJ, Hyatt AE, Gatt CJ Jr, Dhawan A (2014) Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy 30:882–890
Cha PS, Brucker PU, West RV, Zelle BA, Yagi M, Kurosaka M, Fu FH (2005) Arthroscopic double-bundle anterior cruciate ligament reconstruction: an anatomic approach. Arthroscopy 21:1275
Prodromos CC (2010) Posterior mini-incision hamstring harvest. Sports Med Arthrosc Rev 18:12–14
Gobbi A (2010) Single versus double hamstring tendon harvest for ACL reconstruction. Sports Med Arthrosc Rev 18:15–19
Grassi A, Perdisa F, Samuelsson K, Svantesson E, Romagnoli M, Raggi F, Gaziano T, Mosca M, Ayeni O, Zaffagnini S (2018) Association between incision technique for hamstring tendon harvest in anterior cruciate ligament reconstruction and the risk of injury to the infra-patellar branch of the saphenous nerve: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 26:2410–2423
Tillett E, Madsen R, Rogers R, Nyland J (2004) Localization of the semitendinosus-gracilis tendon bifurcation point relative to the tibial tuberosity: an aid to hamstring tendon harvest. Arthroscopy 20:51–54
Reina N, Abbo O, Gomez-Brouchet A, Chiron P, Moscovici J, Laffosse JM (2013) Anatomy of the bands of the hamstring tendon: how can we improve harvest quality? Knee 20:90–95
Ebraheim NA, Mekhail AO (1997) The infrapatellar branch of the saphenous nerve: an anatomic study. J Orthop Trauma 11:195–199
Kartus J, Ejerhed L, Eriksson BI, Karlsson J (1999) The localization of the infrapatellar nerves in the anterior knee region with special emphasis on central third patellar tendon harvest: a dissection study on cadaver and amputated specimens. Arthroscopy 15:577–586. https://doi.org/10.1053/ar.1999.v15.015057001
Ivey M, Prud’Homme J (1993) Anatomic variations of the pes anserinus: a cadaver study. Orthopedics 16:601–606
Funding
The study was financially supported by the National Natural Science Foundation of China (81802172, 82172416), Guangdong Basic and Applied Basic Research Foundation (2021A1515012337, 2019A1515011684), Natural Science Foundation of Guangdong Province (2017A030313854), and Guangdong Science and Technology Collaborative Innovation Center for Sports (2019B110210004). We thank medical illustrator Deng Yuan for making illustrations.
Author information
Authors and Affiliations
Contributions
Jialong Luo: conceptualized the study, designed the research, performed the experiments, interpreted the data, wrote the manuscript, and submitted the manuscript. Shuzhen Li: designed the research, performed the experiments, interpreted the data, and wrote the manuscript. Chenyu Wang: designed the research, performed the experiments, and wrote the manuscript. Qibo Li: designed the research, performed the experiments, and wrote the manuscript. Jianghua Lin: designed the research, performed the experiments, and wrote the manuscript. Yuan Shen: designed the research, performed the experiments, and wrote the manuscript. Yuchen Wang: designed the research, performed the experiments, and wrote the manuscript. Dazheng Xu: designed the research, performed the experiments, and wrote the manuscript. Bin Song: donceptualized the study, designed the research, and wrote the manuscript. Chuan Jiang: conceptualized the study, designed the research and wrote the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Sun Yat-sen Memorial Hospital, Sun Yat-sen University.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, J., Li, S., Wang, C. et al. Optimization of surgical exposure for harvesting gracilis-semitendinosus tendons. International Orthopaedics (SICOT) 47, 131–140 (2023). https://doi.org/10.1007/s00264-022-05598-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05598-5