Abstract
Purpose
Incorrect positioning of components during total knee arthroplasty (TKA) increases the risk of pain, instability, and early revision. The purpose of this study was to compare 3D planning-assisted and a conventional system for TKA positioning. We hypothesized that the use of three-dimensional CT-scan planning and custom cutting guides would increase the accuracy of component positioning.
Methods
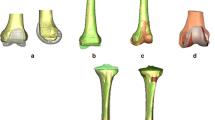
A randomized, controlled, prospective study of two groups was performed. In one group, patient-specific custom cutting guides (PSCG) were used for component positioning based on 3D CT-scan planning. In the control group, TKA was performed with a conventional ancillary system. The components’ positioning angles were measured on 3D reconstructions. The main evaluation criterion was the percentage of outliers outside of a target zone of ± 3° for the coronal positioning of the femoral component.
Results
Eighty patients were included. The percentage of outliers for the femoral component was significantly lower in the 3D-guided group (1 patient) compared to the control group (7 patients p = 0.02). The coronal femoral angle was restored with greater accuracy in the 3D-assisted group (− 0.1° ± 1.4°) compared to the control group (1.6° ± 2.5°). Surgery was significantly shorter in the 3D group. The clinical outcomes were better in the 3D group at the two year follow-up with fewer failures and a lower standard deviation in IKS scores.
Conclusion
The use of a 3D planning and custom guides can improve TKA component positioning by increasing the accuracy of implants alignment and reducing the percentage of outliers. The same benefit was not demonstrated for the global knee alignment and the clinical scores with no indisputable clinical advantage for the PSCG.









Similar content being viewed by others
References
Baker PN, Petheram T, Avery PJ, Gregg PJ, Deehan DJ (2012) Revision for unexplained pain following unicompartmental and total knee replacement. J Bone Joint Surg Am 94:e126. https://doi.org/10.2106/JBJS.K.00791
Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R (2015) Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am 97:715–720. https://doi.org/10.2106/JBJS.M.01534
Hardeman F, Londers J, Favril A, Witvrouw E, Bellemans J, Victor J (2012) Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:1049–1056. https://doi.org/10.1007/s00167-011-1624-8
Boonen B, Schotanus MG, Kerens B, Hulsmans FJ, Tuinebreijer WE, Kort NP (2015) Patient-specific positioning guides for total knee arthroplasty: no significant difference between final component alignment and pre-operative digital plan except for tibial rotation. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-015-3661-1
Chareancholvanich K, Narkbunnam R, Pornrattanamaneewong C (2013) A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Joint J 95-B:354–359. https://doi.org/10.1302/0301-620X.95B3.29903
Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C (2007) A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am 89:236–243. https://doi.org/10.2106/JBJS.F.00386
Hamilton WG, Parks NL (2014) Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplast 29:1508–1509. https://doi.org/10.1016/j.arth.2014.01.029
Marimuthu K, Chen DB, Harris IA, Wheatley E, Bryant CJ, MacDessi SJ (2014) A multi-planar CT-based comparative analysis of patient-specific cutting guides with conventional instrumentation in total knee arthroplasty. J Arthroplast 29:1138–1142. https://doi.org/10.1016/j.arth.2013.12.019
Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J (2014) Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res 472:263–271. https://doi.org/10.1007/s11999-013-2997-4
Woolson ST, Harris AH, Wagner DW, Giori NJ (2014) Component alignment during total knee arthroplasty with use of standard or custom instrumentation: a randomized clinical trial using computed tomography for postoperative alignment measurement. J Bone Joint Surg Am 96:366–372. https://doi.org/10.2106/JBJS.L.01722
Yau WP, Chiu KY, Zuo JL, Tang WM, Ng TP (2008) Computer navigation did not improve alignment in a lower-volume total knee practice. Clin Orthop Relat Res 466:935–945. https://doi.org/10.1007/s11999-008-0144-4
Roh YW, Kim TW, Lee S, Seong SC, Lee MC (2013) Is TKA using patient-specific instruments comparable to conventional TKA? A randomized controlled study of one system. Clin Orthop Relat Res 471:3988–3995. https://doi.org/10.1007/s11999-013-3206-1
Franceschi JP, Sbihi A, Computer Assisted Orthopedic Surgery F (2014) 3D templating and patient-specific cutting guides (knee-plan) in total knee arthroplasty: postoperative CT-based assessment of implant positioning. Orthop Traumatol Surg Res 100:S281–S286. https://doi.org/10.1016/j.otsr.2014.04.003
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 13–14
Thienpont E, Schwab PE, Fennema P (2017) Efficacy of patient-specific instruments in total knee arthroplasty: a systematic review and meta-analysis. J Bone Joint Surg Am 99:521–530. https://doi.org/10.2106/JBJS.16.00496
De Vloo R, Pellikaan P, Dhollander A, Vander Sloten J (2017) Three-dimensional analysis of accuracy of component positioning in total knee arthroplasty with patient specific and conventional instruments: a randomized controlled trial. Knee 24:1469–1477. https://doi.org/10.1016/j.knee.2017.08.059
Abane L, Zaoui A, Anract P, Lefevre N, Herman S, Hamadouche M (2018) Can a single-use and patient-specific instrumentation be reliably used in primary total knee arthroplasty? A multicenter controlled study. J Arthroplast 33:2111–2118. https://doi.org/10.1016/j.arth.2018.02.038
Kosse NM, Heesterbeek PJC, Schimmel JJP, van Hellemondt GG, Wymenga AB, Defoort KC (2018) Stability and alignment do not improve by using patient-specific instrumentation in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 26:1792–1799. https://doi.org/10.1007/s00167-017-4792-3
Anderl W, Pauzenberger L, Kolblinger R, Kiesselbach G, Brandl G, Laky B, Kriegleder B, Heuberer P, Schwameis E (2016) Patient-specific instrumentation improved mechanical alignment, while early clinical outcome was comparable to conventional instrumentation in TKA. Knee Surg Sports Traumatol Arthrosc 24:102–111. https://doi.org/10.1007/s00167-014-3345-2
Keshmiri A, Maderbacher G, Baier C, Benditz A, Grifka J, Greimel F (2018) Kinematic alignment in total knee arthroplasty leads to a better restoration of patellar kinematics compared to mechanic alignment. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5284-9
d'Amato M, Ensini A, Leardini A, Barbadoro P, Illuminati A, Belvedere C (2018) Conventional versus computer-assisted surgery in total knee arthroplasty: comparison at ten years follow-up. Int Orthop. https://doi.org/10.1007/s00264-018-4114-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Intellectual property rights: royalties from Symbios SA.
Ethical approval
The study was approved by the local ethical committee.
Informed consent
All of the patients provided informed consent to participate in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Therapeutic Level I.
Rights and permissions
About this article
Cite this article
Sariali, E., Kajetanek, C. & Catonné, Y. Comparison of custom cutting guides based on three-dimensional computerized CT-scan planning and a conventional ancillary system based on two-dimensional planning in total knee arthroplasty: a randomized controlled trial. International Orthopaedics (SICOT) 43, 2529–2538 (2019). https://doi.org/10.1007/s00264-019-04357-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04357-3