Abstract
Introduction
To investigate the short- and medium-term efficacy of inter-spinal distraction fusion (ISDF) for lumbar disc herniation with a spinal internal fixation device, the BacFuse Spinous Process Fusion Plate.
Methods
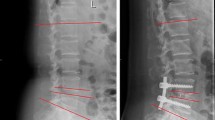
Ninety-five patients who received ISDF between January 2014 and January 2015 were included for the current retrospective study. The symptoms and imaging results before surgery, immediately after surgery, at six months, and at the last follow-up were assessed using the leg visual analogue scale (VAS), Oswestry disability index (ODI), and 12-item short-form survey (SF-12). The intra-operative intervertebral angle (IA), anterior disk height (ADH), posterior disk height (PDH), foramina height (FH), foramina width (FW), and range of motion (ROM) were assessed using X-rays. The foramina and herniated disc area were assessed using computed tomography (CT).
Results
The leg VAS, ODI, and SF-12 were significantly improved after surgery. All indices except ADH were also significantly improved after surgery. PDH and FH increased by 15.5% (P < 0.001) and 9.7% (P < 0.001) at the last follow-up. ROM was statistically different from before surgery. CT images indicated that the herniated disc area decreased by 3.1%, while the foramina areas increased by 5.7% at the last follow-up. 92.6% patients demonstrated successful outcome.
Conclusions
ISDF significantly alleviated the clinical symptoms, improved spinal structure, and partially retracted the herniated disc. Our findings imply that ISDF is an effective minimally invasive procedure in the treatment of lumbar disc herniation.





Similar content being viewed by others
References
Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S et al (2014) An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 14:180–189
Buttermann GR et al (2004) Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am 86:670–679
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS et al (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the spine patient outcomes research trial (SPORT). A randomized trial. JAMA 2006(296):2441–2450
Weber H (1983) Lumbar disc herniation: a controlled, prospective study with ten years of observation. Spine 8:131–140
Fan G, Han R, Gu X et al (2016) Navigation improves the learning curve of transforamimal percutaneous endoscopic lumbar discectomy[J]. Int Orthop 41(2):1–10
Du J, Tang X, Xin J et al (2016) Outcomes of percutaneous endoscopic lumbar discectomy via a translaminar approach, especially for soft, highly down-migrated lumbar disc herniation[J]. Int Orthop 40(6):1247–1252
Christie SD, Song JK, Fessler RG (2005) Dynamic interspinous process technology. Spine 30(16 Suppl):S73–S78
Kabir SM, Gupta SR, Casey AT (2010) Lumbar interspinous spacers: a systematic review of clinical and biomechanical evidence. Spine 35:E1499–E1506
Bellini CM, Galbusera F, Raimondi MT, Mineo GV, Brayda-Bruno M (2007) Biomechanics of the lumbar spine after dynamic stabilization. J Spinal Disord Tech 20:423–429
Holinka J, Krepler P, Matzner M et al (2011) Stabilising effect of dynamic interspinous spacers in degenerative low-grade lumbar instability.[J]. Int Orthop 35(3):395–400
Gazzeri R, Galarza M, Alfieri A (2014) Controversies about interspinous process devices in the treatment of degenerative lumbar spine diseases: past, present, and future. Biomed Res Int 2014:975052
Jiang YQ, Che W, Wang HR, Li RY, Li XL, Dong J (2015) Minimum 5 year follow-up of multi-segmental lumbar degenerative disease treated with discectomy and the Wallis interspinous device. J Clin Neurosci 22:1144–1149
Barbagallo GM, Olindo G, Corvino L, Albanese V (2009) Analysis of complications in patients treated with the X-STOP interspinous process decompression system: proposal for a novel anatomic scoring system for patients selection and review of the literature. Neurosurgery 66:1111–1119
Bowers C, Amini A, Dailey AT, Schmidt MH (2010) Dynamic interspinous process stabilization: review of complications associated with the X-STOP device. Neurosurg Focus 28:E8
Kim DH, Tantorski M, Shaw J, Martha J, Li L, Shanti N et al (2011) Occult spinous process fractures associated with interspinous process spacers. Spine 36:E1080–E1085
Kutcha J, Sobottke R, Cysel P, Simons P (2009) Two-year results of interspinous spacer (X-STOP) implantation of 175 patients with neurologic intermittent claudication due to lumbar spinal stenosis. Eur Spine J 18:823–829
Xu C, Ni WF, Tian NF et al (2013) Complications in degenerative lumbar disease treated with a dynamic interspinous spacer (Coflex)[J]. Int Orthop 37(11):2199–2204
Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Gabriel Rothman SL, Sze GK (2014) Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J 14:2525–2545
Wan Z, Wang S, Kozanek M, Xia Q, Mansfield FL, Lü G et al (2012) The effect of the X-stop implantation on intervertebral foramen, segmental spinal canal length and disc space in elderly patients with lumbar spinal stenosis. Eur Spine J 21:400–410
Kim HY, Choi BW (2013) Change of radiological parameters after interspinous implantation (X-stop®) in degenerative spinal stenosis. Eur J Orthop Surg Traumatol 23:281–285
Kumar N, Shah SM, Ng YH, Pannierselvam VK, Dasde S, Shen L (2014) Role of Coflex as an adjunct to decompression for symptomatic lumbar spinal stenosis. Asian Spine J 8:161–169
Wang Y, Qian B, Li B, Qin G, Zhou Z, Qiu Y et al (2013) Metal artifacts reduction using monochromatic images from spectral CT: evaluation of pedicle screws in patients with scoliosis. Eur J Radiol 82:e360–e366
Veresciagina K, Spakauskas B, Ambrozaitis KV (2010) Clinical outcomes of patients with lumbar disc herniation, selected for one-level open-discectomy and microdiscectomy. Eur Spine J 9:1450–1458
Hoogland T, Schubert M, Miklitz B, Ramirez A (2006) Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine 31:E890–E897
Righesso O, Falavigna A, Avanzi O (2007) Comparison of open discectomy with microendoscopic discectomy in lumbar disc herniations: results of a randomized controlled trial. Neurosurgery 61:545–549
Heyrani N, Picinic Norheim E, Elaine Ku Y, Nick SA (2012) Interspinous process implantation for the treatment of neurogenic intermittent claudication. Anesth Pain Med 2:36–41
Siddiqui M, Smith FW, Wardlaw D (2007) One-year results of X-STOP interspinous implant for the treatment of lumbar spinal stenosis. Spine 32:1345–1348
Postacchini F, Postacchini R, Menchetti PP, Sessa P, Paolino M, Cinotti G (2016) Lumbar interspinous process fixation and fusion with stand-alone interlaminar lumbar instrumented fusion implant in patients with degenerative spondylolisthesis undergoing decompression for spinal stenosis. Asian Spine J 10:27–37
Fabrizi AP, Maina R, Schiabello L (2011) Interspinous spacers in the treatment of degenerative lumbar spinal disease our experience with DIAM and Aperius devices. Eur Spine J 20(Suppl 1):S20–S26
Xu D, Chen YH, Zeng HB, Chi YL, Xu HZ (2009) A short-term follow-up results of herniation, a clinical comparison study. Chin J Surg 47:1379–1382
Xu D, Xu HZ, Chen YH, Chi YL, Ni WF, Huang QS et al (2013) Discectomy and discectomy plus Coflex fixation for lumbar disc herniation, a clinical comparison study. Chin J Surg 51:147–151
Wilke HJ, Drumm J, Häussler K, Mack C, Steudel WI, Kettler A (2008) Biomechanical effect of different lumbar interspinous implants on flexibility and intradiscal pressure. Eur Spine J 17:1049–1056
Richards JC, Majumdar S, Lindsey DP, Beaupré GS, Yerby SA (2005) The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine 30:744–749
Hirsch C, Breque C, Ragot S, Pascal-Mousselard H, Richer JP, Scepi M et al (2015) Biomechanical study of dynamic changes in L4-L5 foramen surface area in flexion and extension after implantation of four interspinous process devices. Orthop Traumatol Surg Res 101:215–219
Lee J, Hida K, Seki T et al (2004) An interspinous process distractor (X-STOP) for lumbar spinal stenosis in elderly patients: preliminary experiences in 10 consecutive cases. J Spinal Disord Tech 17:72–77
Sobottke R, Schlüter-Brust K, Kaulhausen T, Iwasaki Y, Minoru A (2009) Interspinous implants (X Stop, Wallis, Diam) for the treatment of LSS is there a correlation between radiological parameters and clinical outcome. Eur Spine J 18:1494–1503
Park SC, Yoon SH, Hong YP, Kim KJ, Chung SK, Kim HJ (2009) Minimum 2-year follow-up result of degenerative spinal stenosis treated with interspinous u (coflex). J Korean Neurosurg Soc 46:292–299
Guehring T, Unglaub F, Lorenz H, Omlor G, Wilke HJ, Kroeber MW (2006) Intradiscal pressure measurements in normal discs, compressed discs and compressed discs treated with axial posterior disc distraction: an experimental study on the rabbit lumbar spine model. Eur Spine J 15:597–604
Hartmann F, Dietz SO, Kuhn S, Hely H, Rommens PM, Gercek E (2011) Biomechanical comparison of an interspinous device and a rigid stabilization on lumbar adjacent segment range of motion. Acta Chir Orthop Traumatol Cechoslov 78:404–409
Nandakumar A, Clark NA, Peehal JP, Bilolikar N, Wardlaw D, Smith FW (2010) The increase in dural sac area is maintained at 2 years after X-stop implantation for the treatment of spinal stenosis with no significant alteration in lumbar spine range of movement. Spine J 10:762–768
Kroeber M, Unglaub F, Guehring T, Nerlich A, Hadi T, Lotz J et al (2005) Effects of controlled dynamic disc distraction on degenerated intervertebral discs: an in vivo study on the rabbit lumbar spine model. Spine 30:181–187
Kamanli A, Karaca-Acet G, Kaya A, Koc M, Yildirim H (2010) Conventional physical therapy with lumbar traction; clinical evaluation and magnetic resonance imaging for lumbar disc herniation. Bratisl Lek Listy 111:541–544
Choi J, Lee S, Hwangbo G (2015) Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation. J Phys Ther Sci 27:481–483
Sari H, Akarirmak U, Karacan I, Akman H (2005) Computed tomographic evaluation of lumbar spinal structures during traction. Physiother Theory Pract 21:3–11
Ozturk B, Gunduz OH, Ozoran K, Bostanoglu S (2006) Effect of continuous lumbar traction on the size of herniated disc material in lumbar disc herniation. Rheumatol Int 26:622–626
BenEliyahu DJ (1996) Magnetic resonance imaging and clinical follow-up: study of 27 patients receiving chiropractic care for cervical and lumbar disc herniations. J Manip Physiol Ther 19:597–606
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Wei, H., Tang, H., Zhang, T. et al. Preliminary efficacy of inter-spinal distraction fusion which is a new technique for lumbar disc herniation. International Orthopaedics (SICOT) 43, 899–907 (2019). https://doi.org/10.1007/s00264-018-4188-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4188-0