Abstract
Purpose
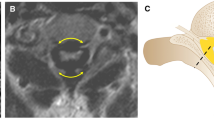
Mucopolysaccharidosis (MPS) are rare inherited metabolic diseases, causing lysosomal storage of mucopolysaccharides; clinical presentation involves skeletal system and particularly the spine. Anomalies include developing kyphosis at thoracolumbar junction, that can causes nervous symptoms, and dens hypoplasia with associated atlantoaxial subluxation that can cause myelopathy. We present our experience in the treatment of spine pathology in MPS.
Methods
Medical treatments of MPS seem to have little impact on spine disease: treatment of cervical instability often includes surgical decompression and stabilization, as in patient MPS1 that we present, while thoracic lumbar kyphosis is treated by bracing and, in severe cases, with surgery. Bracing is more effective in kyphosis under 40° Cobb. Our surgical cases with thoracic lumbar kyphosis over 40° Cobb, treatment include the first one ever described by only posterior approach with vertebrectomy in MPS and a case of lateral costo-transverse approach instrumented correction.
Results
Surgical patients had no major complications after surgery and CT scan at follow-up showed complete fusion without loss of correction, even if in a cervical case we used an adult rigid instrumentation in a four year-and-six month-old girl (11 years follow-up) and in thoracic lumbar kyphosis case treated by vertebrectomy due to diminutive anatomy we positioned interbody cage in suboptimal position.
Conclusions
Bracing is a viable treatment strategy in thoracic lumbar kyphosis and can obtain good clinical results at medium terms follow-up even if kyphosis deformity remains in radiographs. Surgical treatment is effective in severe evolving cases both at cervical and thoracic lumbar level, main difficulties arose from unavailability of dedicated instrumentation in very young patient, as even smallest devices available are often too big.





Similar content being viewed by others
References
Yanagishita (1993) M function of proteoglycans in the extracellular matrix. Acta Pathol Jpn 43(6):283–293
Clearly MA, Wraith JE (1995) The presenting features of mucopolysaccharidosis type IH (Hurler syndrome). Acta Paediatr 84:337–338
Aldenhoven M, Sakkers RJB, Boelens J, De Koning TJ, Wulffrat NM (2009) Musculoskeletal manifestations of lysosomal storage disorders. Ann Rheum Dis 68:1659–1665
Hobbs JR (1981) Bone marrow transplantation for inborn errors. Lancet 2:735–739
Peters C, Steward CG (2003) Hematopoietic cell transplantation for inherited metabolic diseases: an overview of outcomes and practice guidelines. Bone Marrow Transplant 41:1005–1011
Souillet G, Guffon N, Marie I et al (2003) Outcome of 27 patients with Hurler’s syndrome transplanted from either related or unrelated haematopoietic stem cell sources. Bone Marrow Transplant 31:1105–1117
Hugh-Jones K (1986) Psychomotor development of children with mucopolysaccharidosis type1-H following bone marrow transplantation. Birth Defects Orig Artic Ser 22:25–29
Breider MA, Shull RM, Constantopoulos G (1989) Long-term effects of bone marrow transplantation in dogs with mucopolysaccharidosis. I Am J Pathol 134:677–692
Van der Linden MH, Kruyt MC, Sakkers RJB, de Koning TJ, Oner FC, Castelein RM (2011) Orthopaedic management of Hurler’s disease after hematopoietic stem cell transplantation: a systematic review. J Inherit Metab Dis 34(3):657–669
Weisstein JS, Delgado E, Steinbach LS, Hart K, Packman S (2004) Musculoskeletal manifestations of Hurler syndrome. Long term follow-up after bone marrow transplantation. J Pediatr Orthop 24(1):97–101
Field RE, Buchanan JA, Copplemans MG, Aichroth PM (1994) Bone-marrow transplantation in Hurler’s syndrome. Effect on skeletal development. J Bone Joint Surg Br 76:975–981
Silveri CP, Kaplan FS, Fallon MD, Bayer E, August CS (1991) Hurler syndrome with special reference to hystologic abnormalities of the growth plate. Clin Orthop Relat Res 269:305–311
Vijay S, Wraith JE (2005) Clinical presentation and follow up of patients with the attenuated phenotype of mucopolysaccharidosis type I. Acta Paediatr 94:872–877
Mundada V, D’Souza N (2009) Lumbar gibbus: early presentation of dysostosis multiplex. Arch Dis Child 94:930–931
Tandon V, Williamson JB, Cowie RA (1996) Spinal problems in mucopolysaccharidosis I (hurler syndrome). J Bone Joint Surg Br 78:938–944
Clearly MA, Wraith JE (1995) The presenting features of mucopolysaccharidosis type IH. Acta Paediatr 84:337–339
Genevois KA, Garin C, Solla F, Guffon N, Kohler R (2014) Surgical management of thoracolumbar kyphosis in mucopolysaccharidosis type 1 in a reference center. J Inherit Metab Dis 37:69–78
Swishuk LE (1970) The beaked, notched, or hooked vertebra: its significance in infants and young children. Radiology 95:661–664
Levin TL, Berdon WE, Lachman RS (1997) Lumbar gibbus in storage diseases and bone dysplasias. Pediatr Radiol 27:289–294
Yasin MN, Sacho R, Oxborrow NJ et al (2014) Thoracolumbar kyphosis in treated mucopolysaccaridosis 1 (Hurler syndrome). Spine 39:381–387
Ebara S, Kinoshita T, Yuzawa Y (2003) A case of mucopolysaccharidosis IV with lower leg paresis due to thoracolumbar kyphoscoliosis. J Clin Neurosci 10:358–361
Hughes DG, Chadderton RD, Cowie RA, Wraith JE, Jenkins JP (1997) MRI of the brain and craniocervical junction in Morquio’s disease. Neuroradiology 39(5):381–385
Solanski GA, Lo WB, Hendriksz CJ (2013) MRI morphometric characterisation of the paediatric cervical spine and spinal cord in children with MPS IVA (Morquio-Brailsford syndrome). J Inherit Metab Dis 36(2):329–337
Solanski GA, Martin KW, Theroux MC, Lampe C, White KK et al (2013) Spinal involvement in mucopolysaccharidosis IVA (Morquio-Brailsford or Morquio A syndrome): presentation, diagnosis and management. J Inherit Metab Dis 36:339–355
Leone A, Rigante D, Amato DZ, Casale R, Pedone L et al (2015) Spinal involvement in mucopolysaccharidoses: a review. Child Nerv Syst 31:203–212
White AA, Punjabi MM (1984) The role of stabilization in the treatment of cervical spine injuries. Spine 9:512–522
Meikle PJ, Hopwood JJ, Clague AE, Carey WF (1999) Prevalence of lysosomal storage diseases. JAMA 281:249–254
Rasalkar DD, Chu WC, Hui J, Chu CM et al (2011) Pictorial review of mucopolysaccharidosis with emphasis on MRI features of brain and spine. Br J Radiol 84(1001):469–477
Mackenzie WG, Dhawale AA, Demczko MM, Ditro C, Rogers KJ et al (2013) Flexion-extension cervical spine MRI in children with skeletal dysplasia: is it safe and effective? J Pediatr Orthop 33:91–98
Caillaud C (2014) Principles of therapeutic approaches for mucopolisaccharidoses. Arch Pediatr 21(1):S39–S45
Noh H, Lee JI (2014) Current and potential therapeutic strategies for muchopolysaccharidoses. J Clin Pharm Ther 39(3):215–224
Lipson SJ (1977) Dysplasia of the odontoid process in Morquio’s syndrome causing quadriparesis. J Bone Joint Surg Am 59(3):340–344
Ransford AO, Crockard HA, Stevens JM, Modaghegh S (1996) Occipito-atlanto-axial fusion in Morquio-Brailsford syndrome. A ten-year experience. J Bone Joint Surg 78:307–313
Ashraf J, Crockard HA, Ransford AO, Stevens JM (1991) Transoral decompression and posterior stabilization in Morquio’s disease. Arch Dis Child 66(11):E306–E313
Siddique I, Sacho RH, Oxborrow N et al (2009) Thoracolumbar kyphosis in mucopolysaccharidosis I (Hurler syndrome) proceedings 44th annual meeting and course Scoliosis Research Society San Antonio paper. 48:43
McMaster MJ, Singh H (2001) The surgical management of congenital kyphosis and kyphoscoliosis. Spine 26:2146–2154
Garrido E, Tomé-Bermejo F, Adams CI (2014) Combined spinal arthrodesis with instrumentation for the management of progressive thoracolumbar kyphosis in children with mucopolysaccharidosis. Eur Spine J 23(12):2751–2757
Polgreen LE, Tolar J, Plog M, Himenes JH, Orchard PJ, Whitley CB, Miller BS, Petryk A (2008) Growth and endocrine function in patients with Hurler syndrome after hematopoietic stem cell transplantation. Bone Marrow Transplant 41:1005–1011
Dalvie SS, Noordeen MH, Vellodi A (2001) Anterior instrumented fusion for thoracolumbar kyphosis in mucopolysaccharidosis. Spine 26(23):E539–E541
Bekmez S, Demirkiran HG, Dede O, Ismayilov V, Yazici M (2018) Surgical management of progressive thoracolumbar kyphosis in mucopolysaccharidosis: is a posterior-only approach safe and effective? J Pediatr Orthop 38(7):354–359
Crostelli M, Mazza O, Mariani M (2013) Posterior approach lumbar and thoracolumbar hemivertebra resection in congenital scoliosis in children under 10 years of age: results with 3 years mean follow up. Eur Spine J 23(1):209–215
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Crostelli, M., Mazza, O., Mariani, M. et al. Spine challenges in mucopolysaccharidosis. International Orthopaedics (SICOT) 43, 159–167 (2019). https://doi.org/10.1007/s00264-018-4143-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4143-0